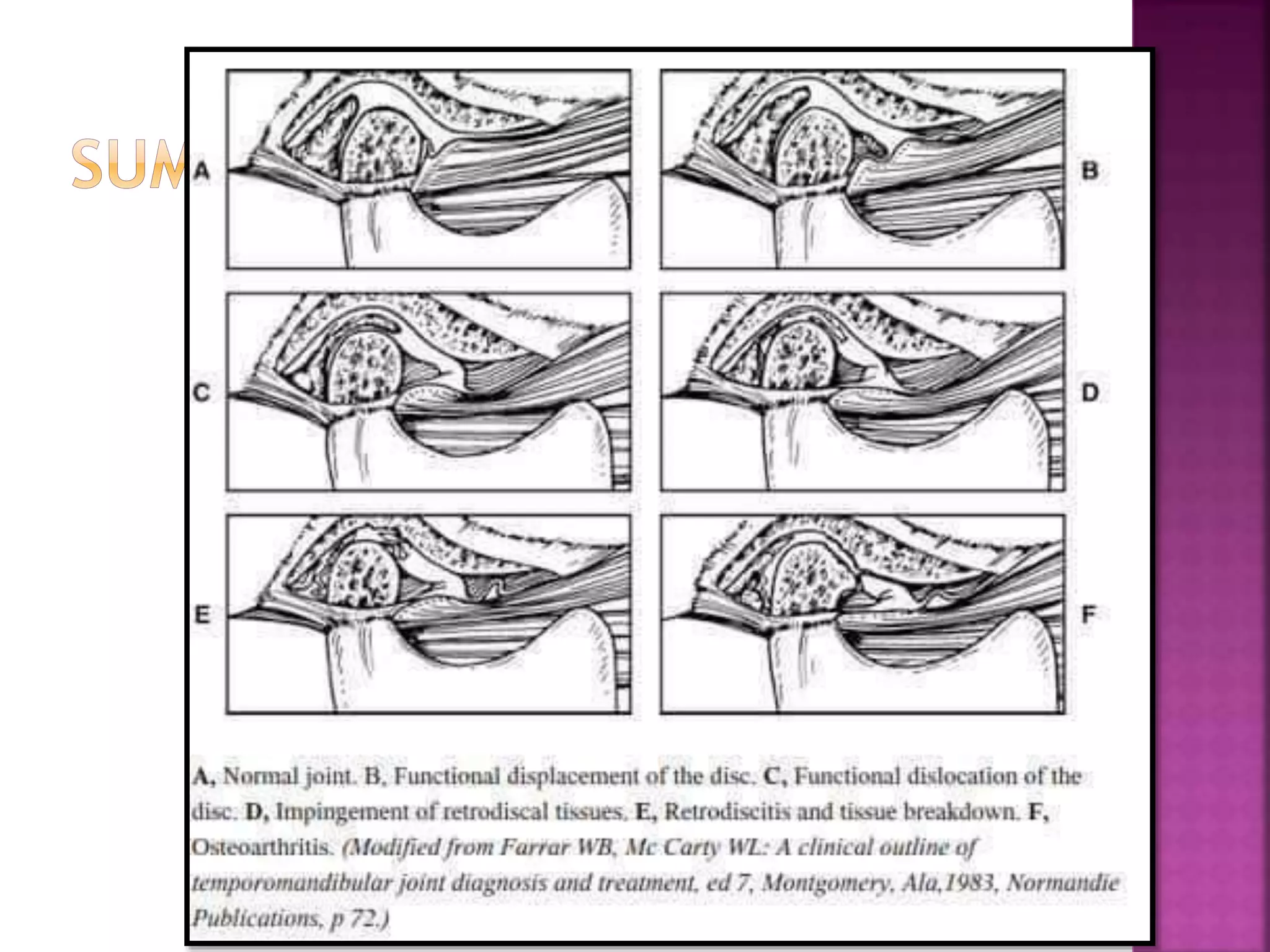
The document provides a comprehensive overview of temporomandibular disorders (TMDs), including their definition, classification, clinical signs, and management strategies. It details various types of jaw movements, diagnostic imaging techniques, and specific disorders related to the temporomandibular joint, along with their epidemiology and differential diagnoses. Additionally, it discusses etiological factors contributing to TMDs and various therapeutic approaches for treatment.