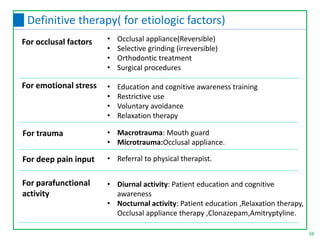
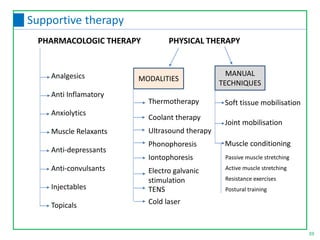
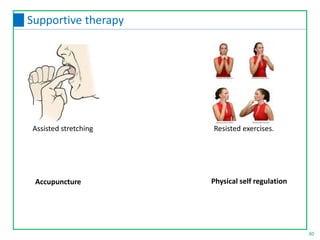
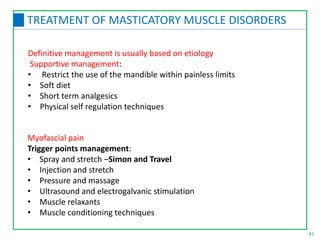
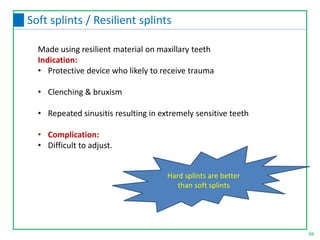
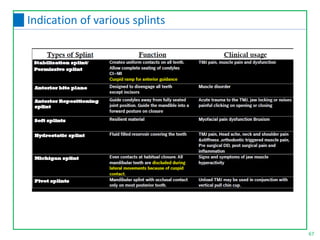
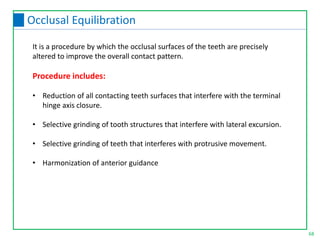
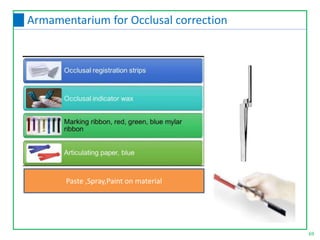
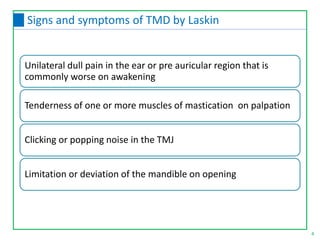
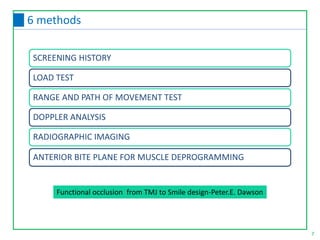
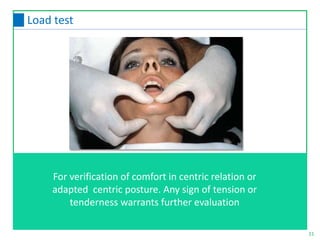
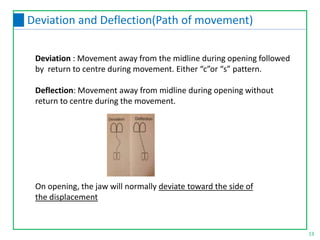
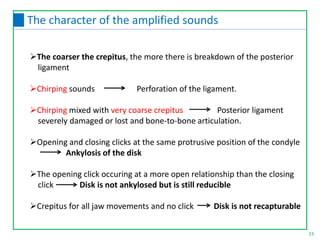
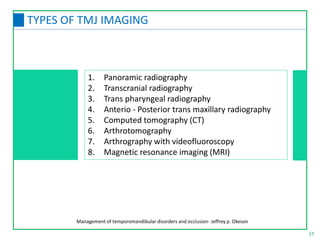
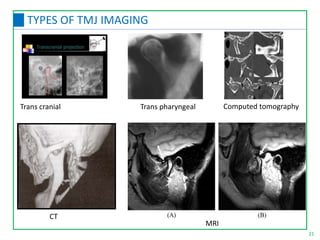
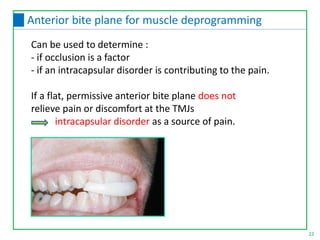
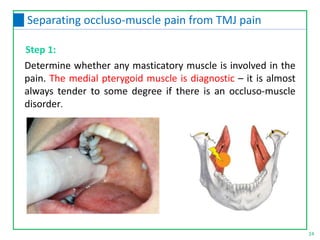
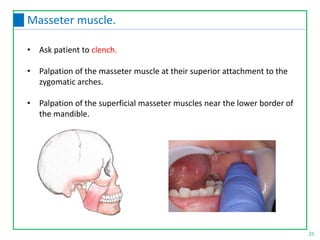
This document discusses the diagnosis and management of temporomandibular joint disorders (TMD). It defines TMD and covers the functional anatomy, etiology, epidemiology, classification, diagnosis, and treatment. For diagnosis, it describes various tests including screening history, load testing, range of motion testing, Doppler analysis, and various radiographic imaging techniques. Treatment involves identifying and addressing the underlying causes, which may include occlusal factors corrected through appliances, selective grinding, or orthodontics, as well as non-occlusal approaches like education, relaxation therapy, and avoidance of micro/macrotrauma.

![Test 1: Clench test
If a patient can clench the teeth together and feel tenderness
in any tooth when the mouth is empty -Positive
Test 2: Anterior deprogramming test
Firmly clench against a cotton roll laid across the arch at
the premolars - If pain is relieved occluso-muscle problem
If clenching on the cotton roll produces discomfort in either
TMJ intracapsular disorder .
Flat anterior deprogramming device [discluder splint] overnight
36
Confirmation of diagnosis of occlusomuscular pain](https://image.slidesharecdn.com/sharitmdsecondpart-210908104914/85/TEMPOROMANDIBULAR-JOINT-DISORDERS-second-part-36-320.jpg)