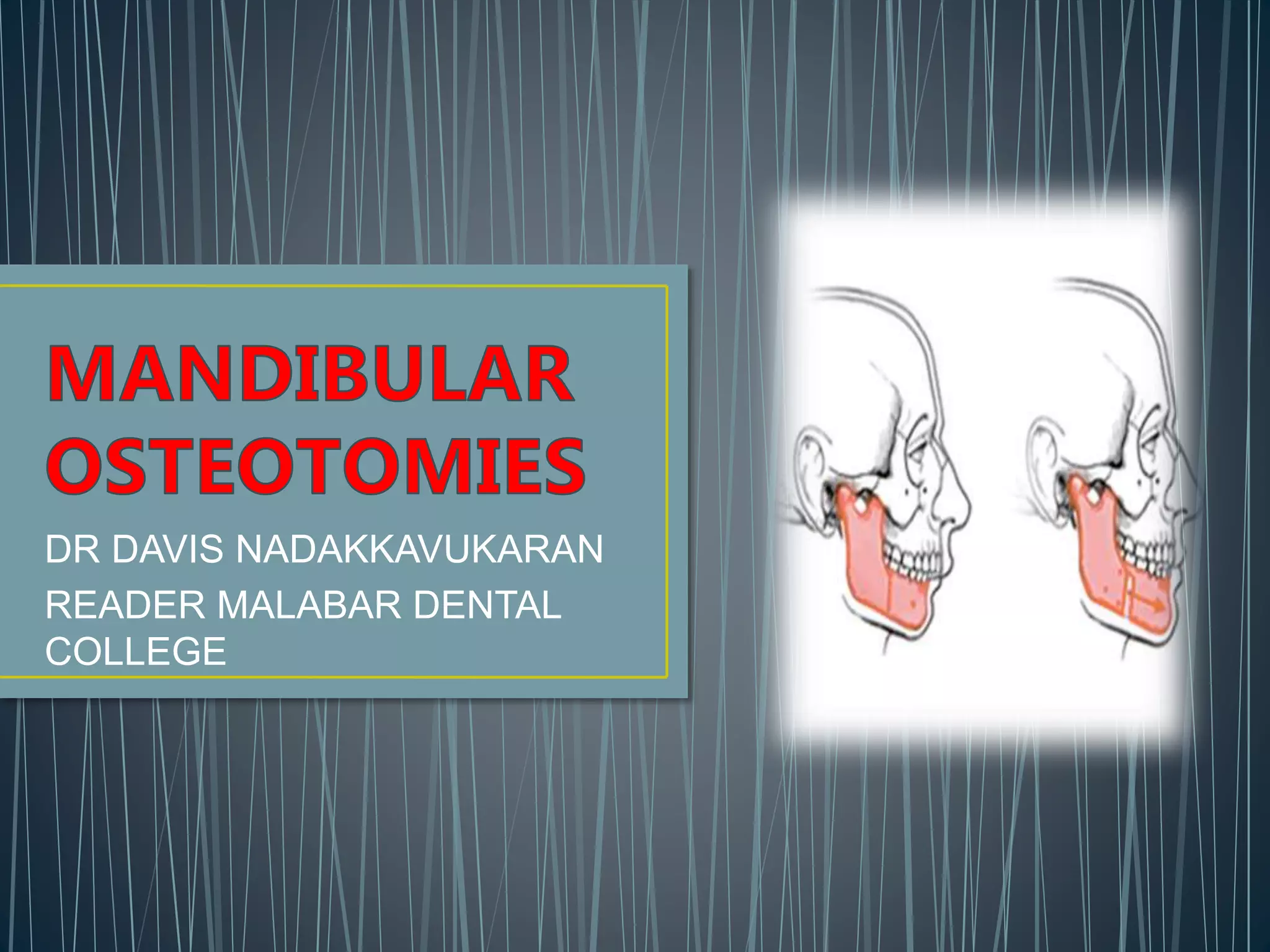
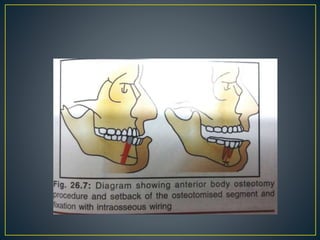
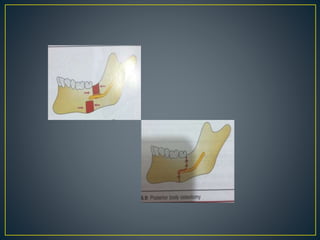
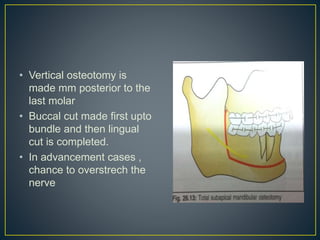
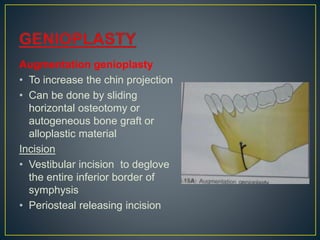
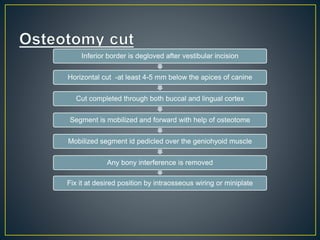
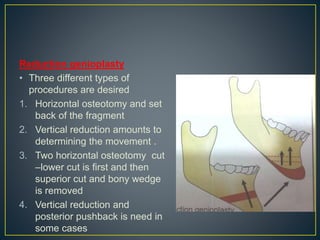
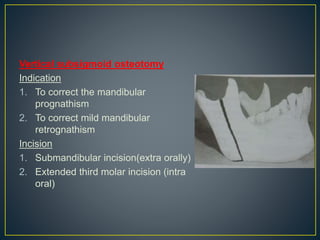
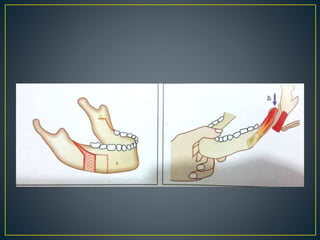
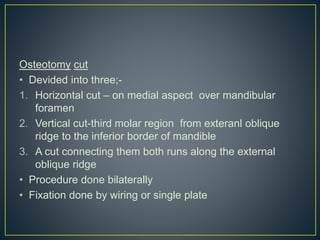
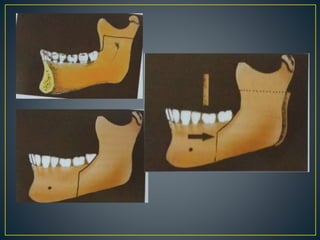
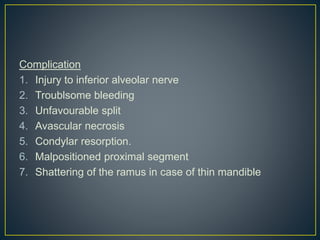
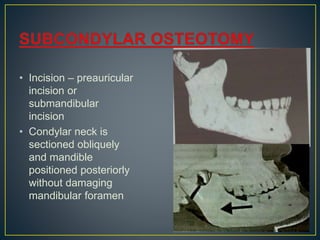
This document provides an overview of various orthognathic surgery procedures for correcting jaw deformities, including different types of mandibular osteotomies and ramus osteotomies. It describes the indications, incisions, osteotomy cuts, and complications for procedures like anterior/posterior body osteotomies, genioplasty, subapical mandibular osteotomies, sagittal split osteotomies, vertical ramus osteotomies, and condylectomies. The goal of these combined orthodontic and surgical techniques is to realign the jaws and associated structures to improve function, aesthetics, and stability.