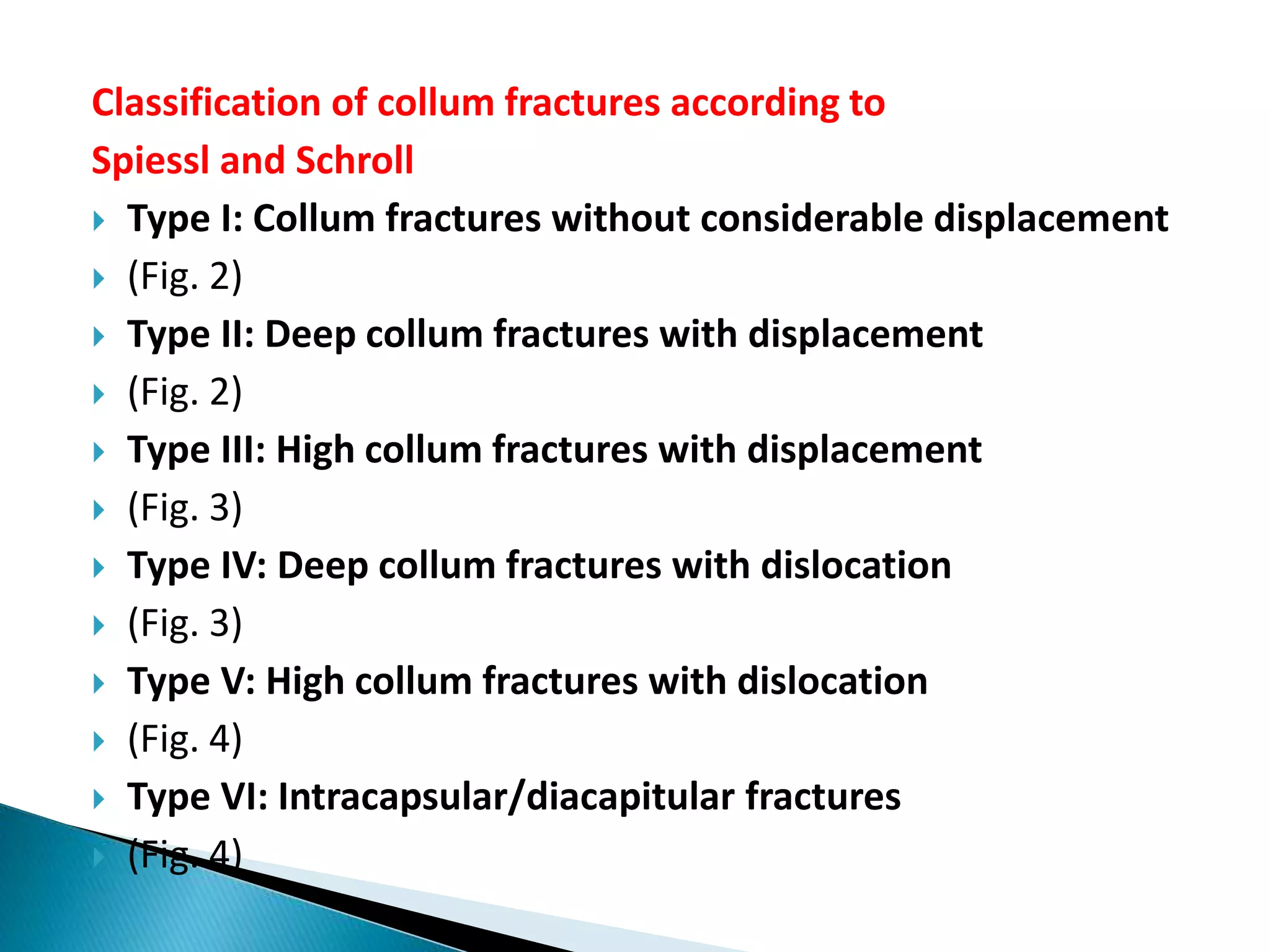
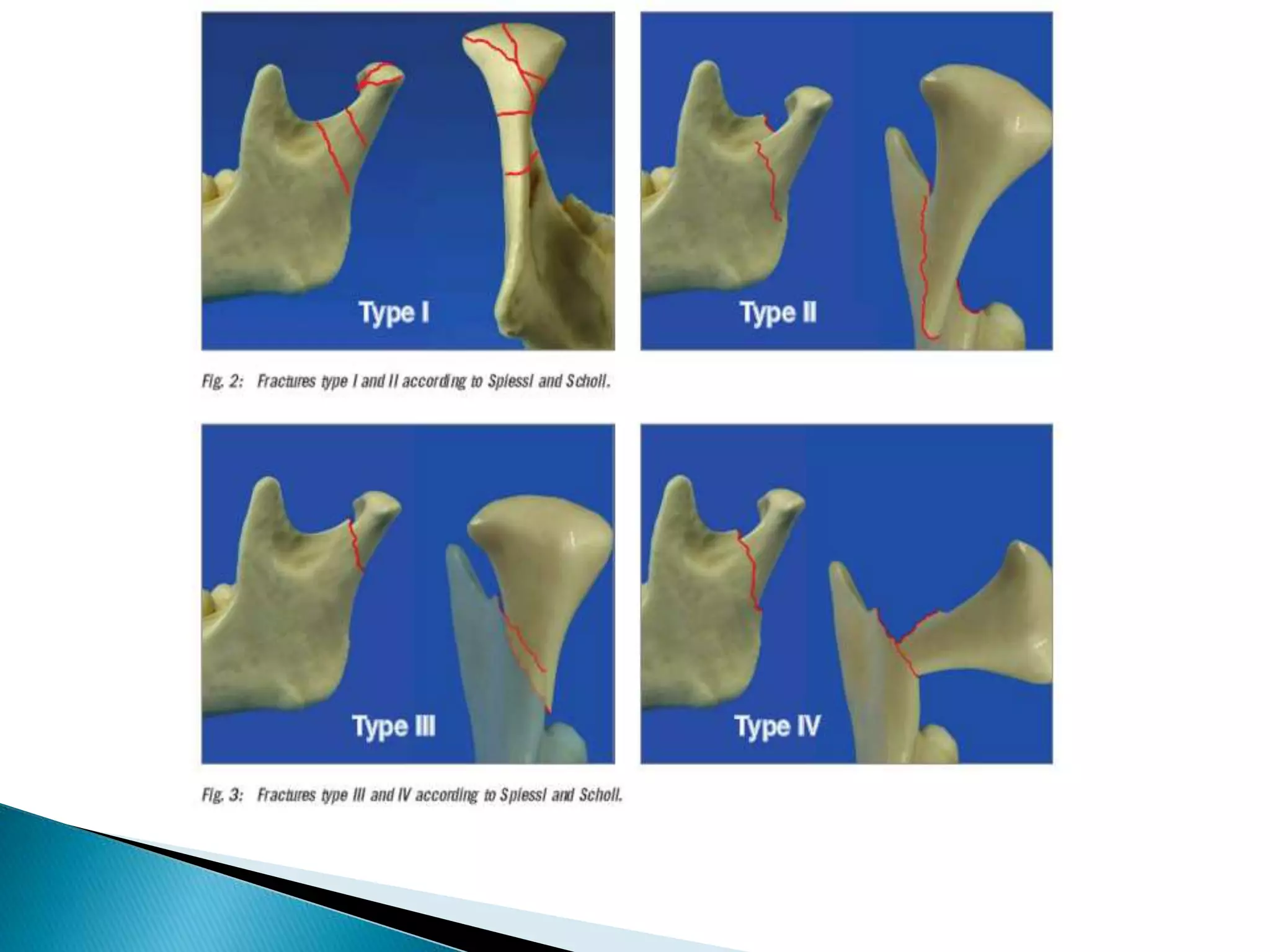
This document discusses condylar fractures of the mandible. It begins with an introduction and overview of condylar fracture classification systems. It then covers the etiology, clinical examination, principles of treatment, and treatment options for condylar fractures, including closed and open reduction techniques. Complications of treatment are also outlined. The document emphasizes that the treatment approach depends on factors like the patient's age, fracture characteristics, and whether other injuries are present. The goal of treatment is to achieve a stable occlusion and restore function through both surgical and non-surgical means.