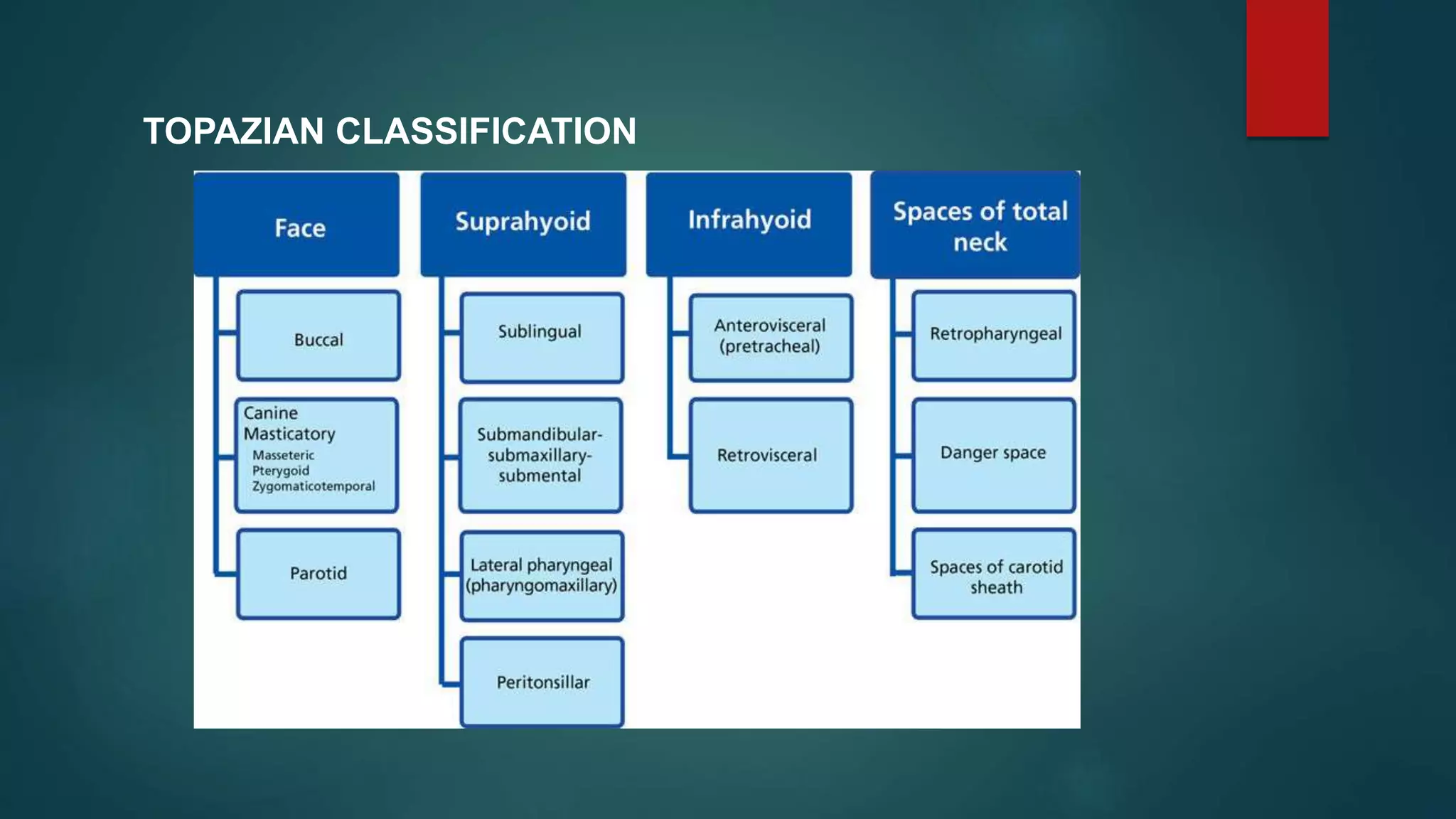
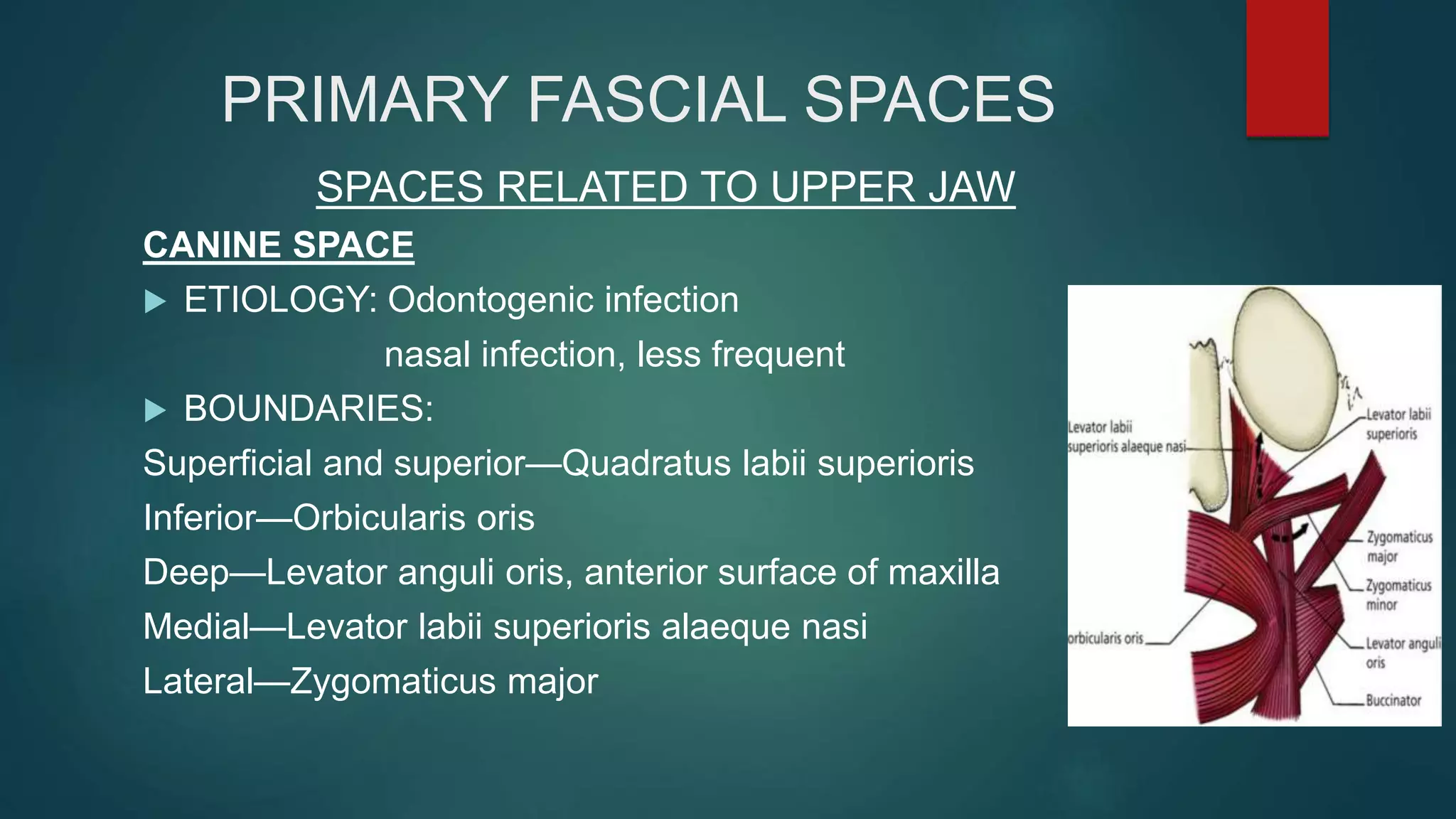
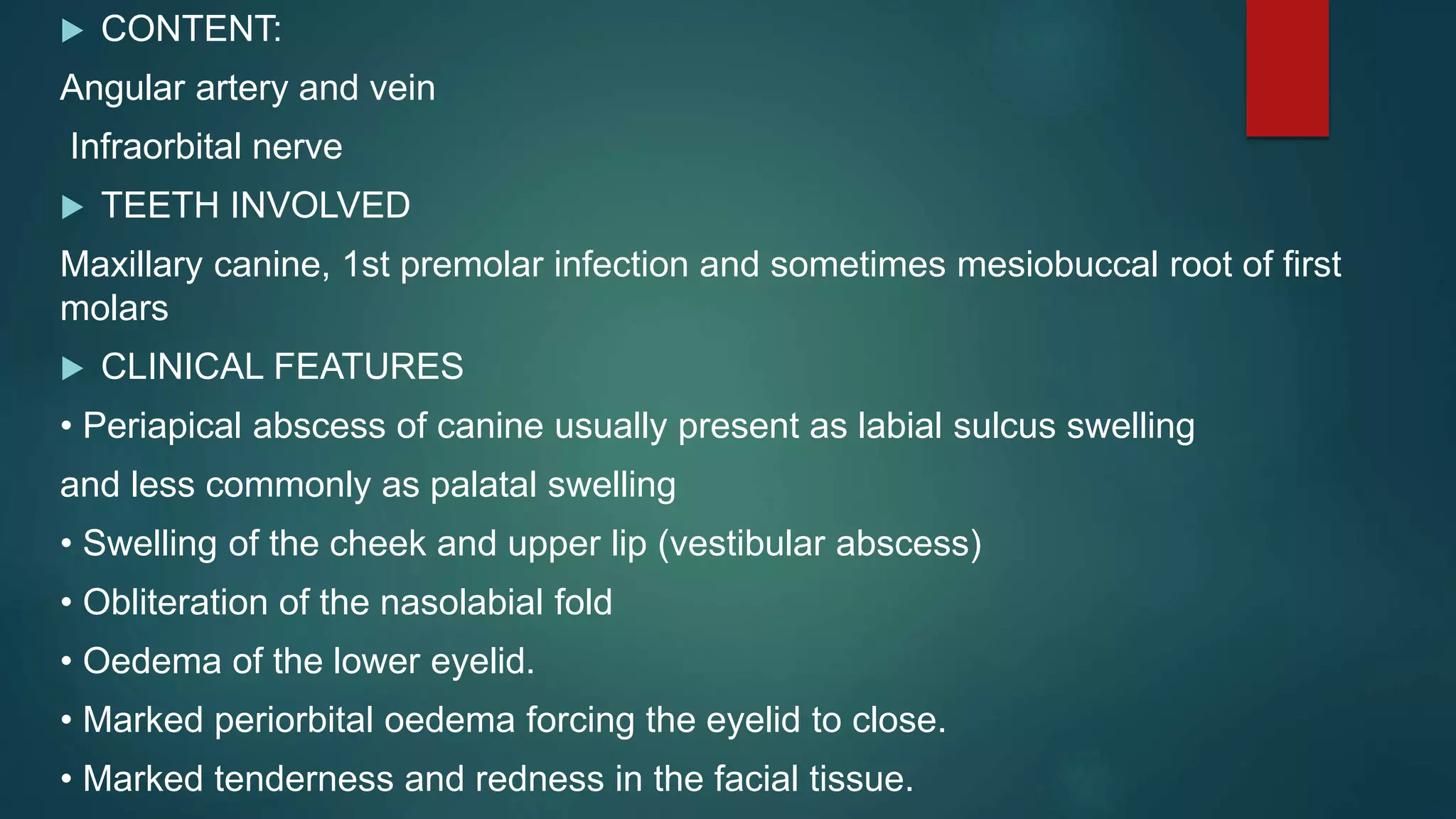
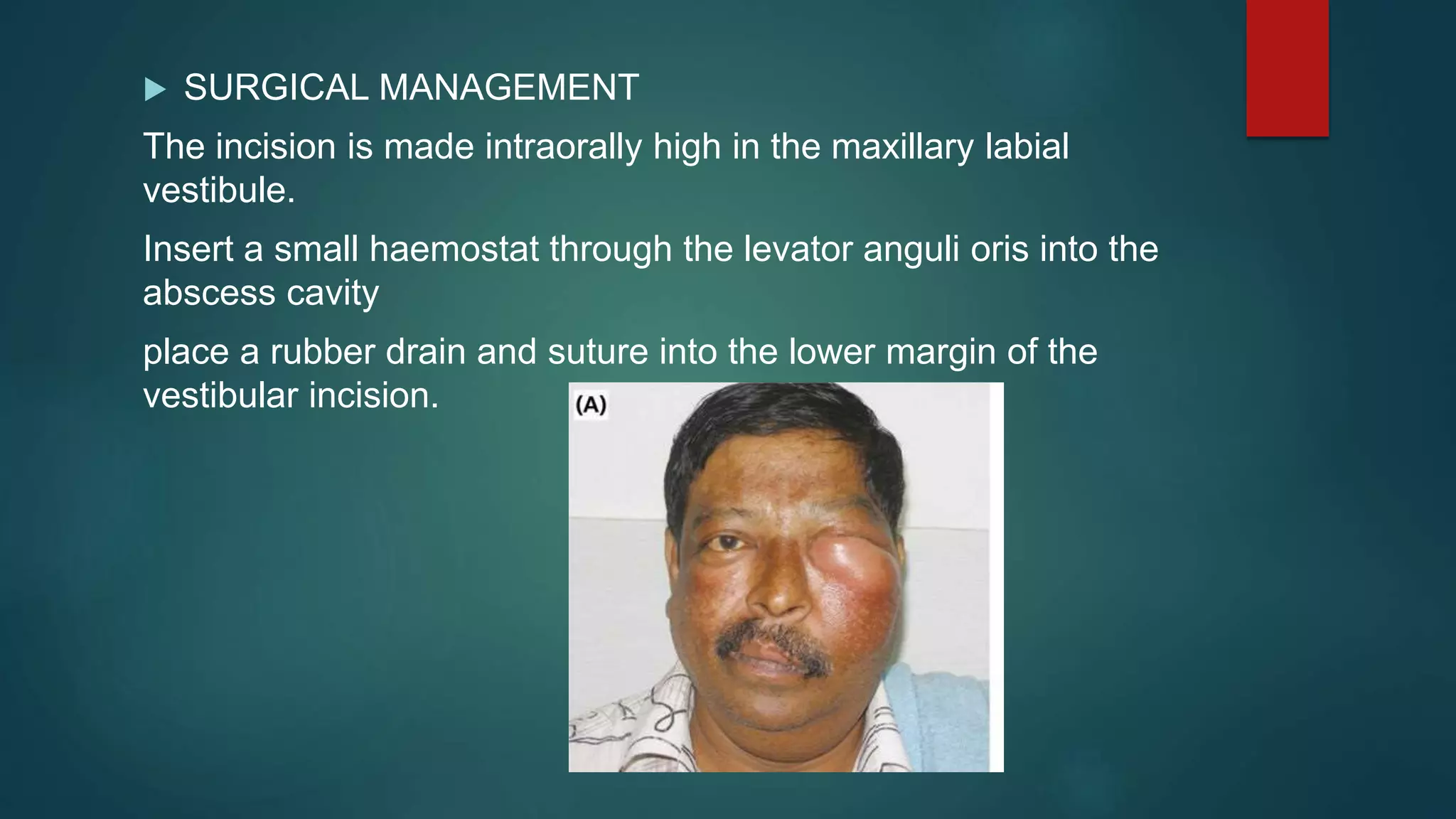
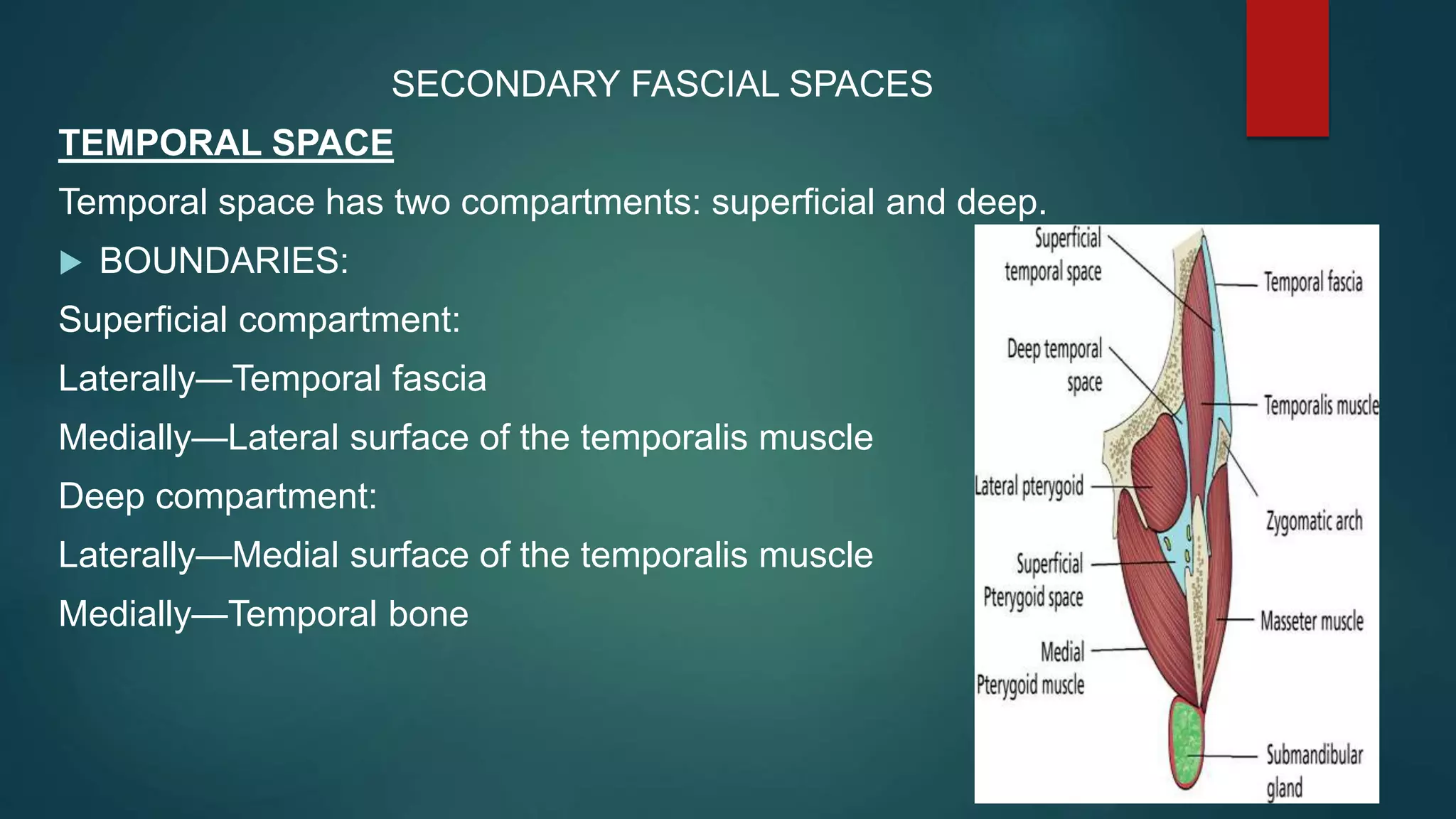
This document discusses various fascial spaces in the head and neck region that can become infected. It describes the boundaries, contents, teeth involved, clinical features, and surgical management for primary spaces like the canine, buccal, infratemporal, submental, submandibular, and sublingual spaces. It also briefly mentions secondary spaces like the masseteric, pterygomandibular, temporal, and others. The document provides detailed anatomical information to help clinicians properly diagnose and treat infections in these potentially dangerous head and neck spaces.