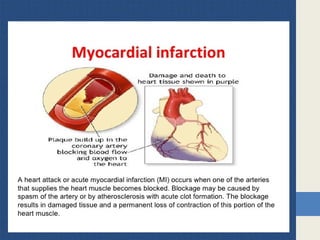
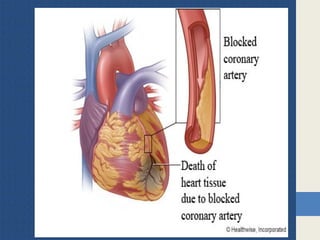
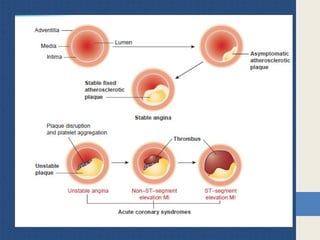
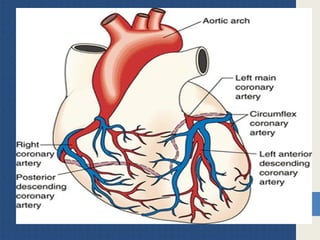
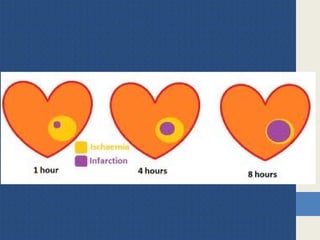
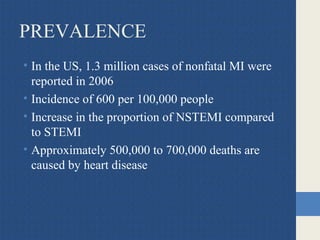
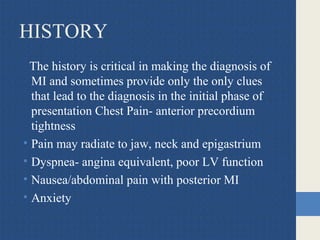
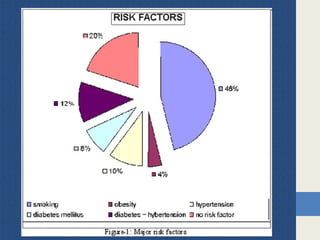
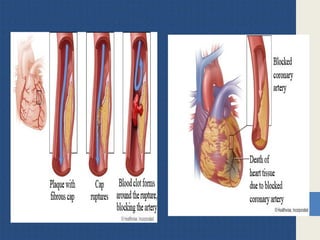
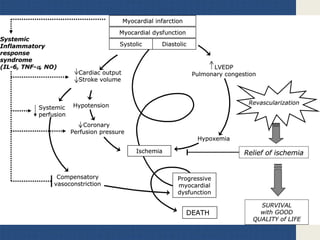
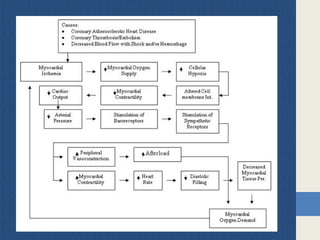
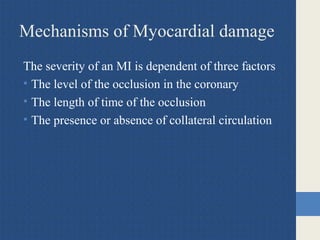
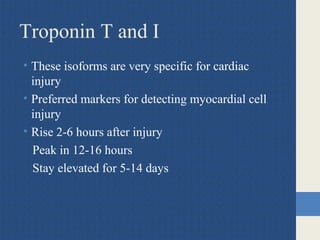
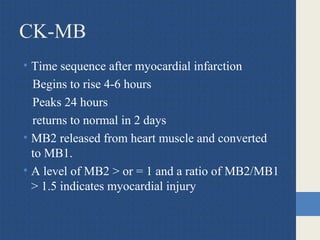
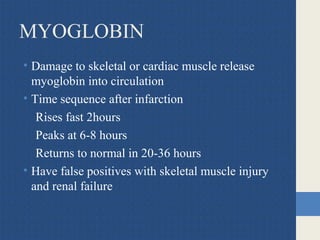
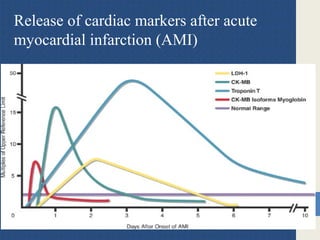
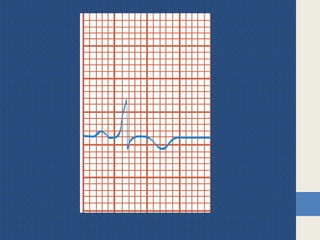
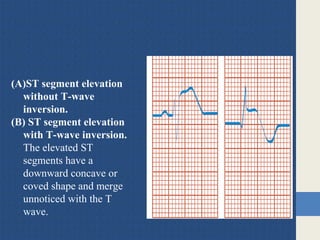
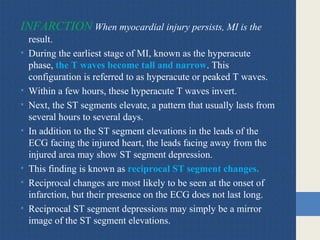
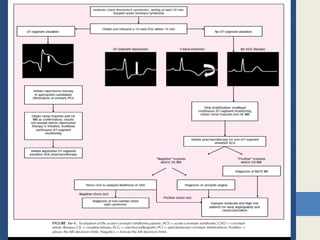
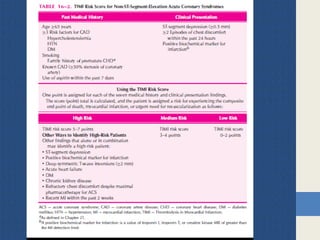
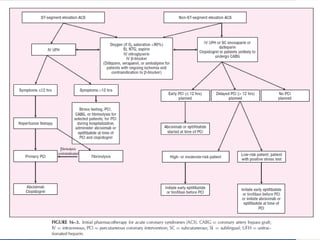
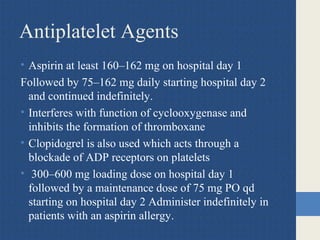
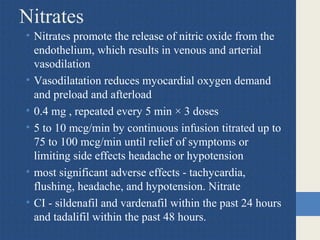
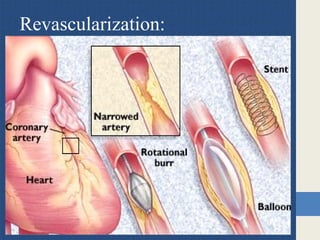
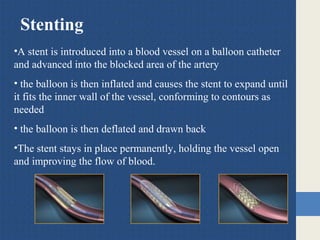
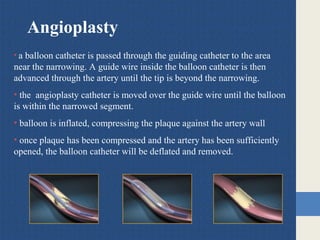
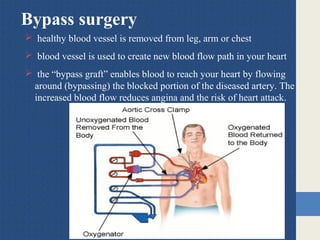
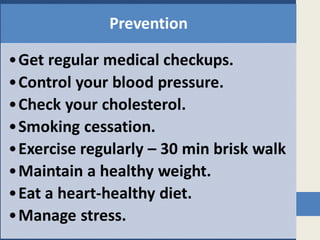
Myocardial infarction, or heart attack, occurs when blood flow to the heart is blocked, damaging heart muscle. There are two main types - STEMI caused by a complete blockage, and NSTEMI from a partial blockage. Risk factors include age, smoking, high cholesterol, diabetes, and family history. Diagnosis involves history, cardiac biomarkers like troponin that indicate heart damage, ECG showing elevated ST segments, and imaging tests. Treatment focuses on restoring blood flow through medications, angioplasty, or bypass surgery, along with long term preventative medications like aspirin, statins, and beta blockers.