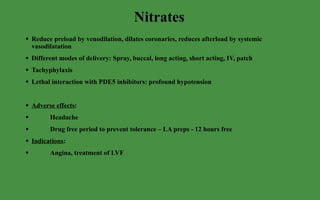
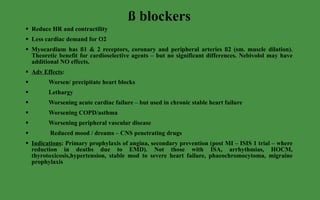
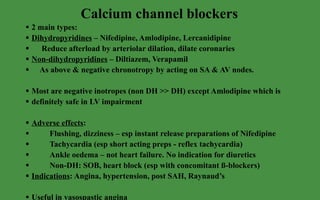
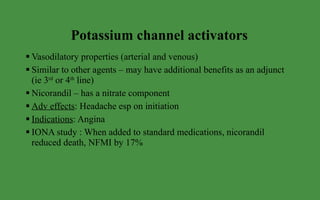
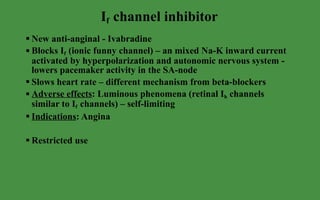
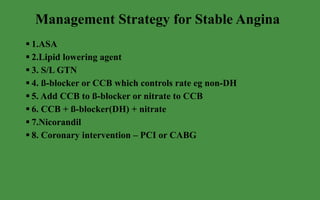
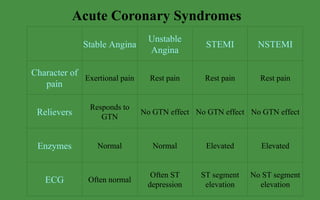
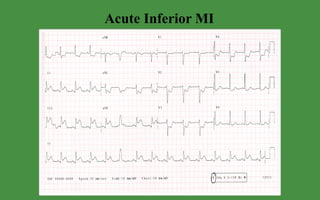
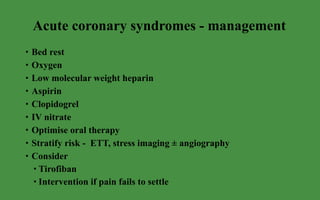
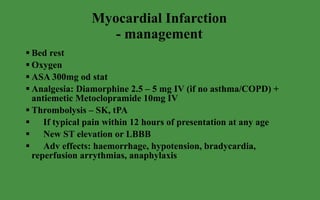
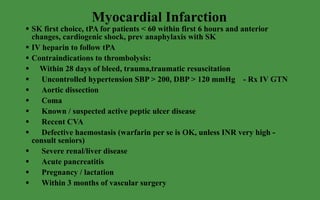
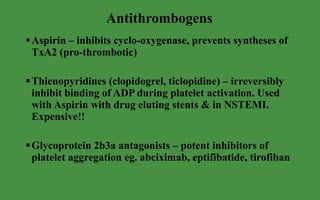
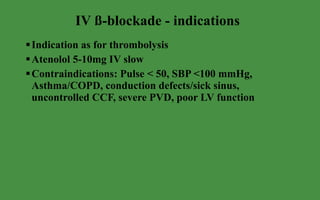
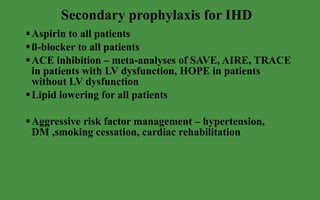
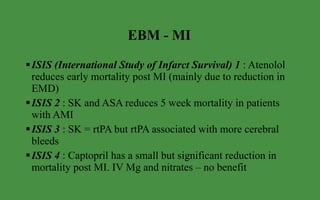
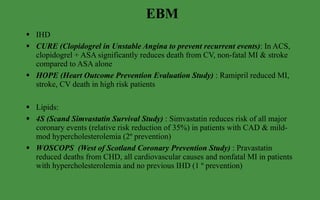
The document discusses ischaemic heart disease and acute coronary syndromes. It describes angina, myocardial infarction, and their management. For stable angina, treatments include nitrates, beta-blockers, calcium channel blockers, and lifestyle modifications. For acute coronary syndromes, management involves oxygen, aspirin, clopidogrel, bed rest, and considering interventions like thrombolysis or angiography. Secondary prevention includes aspirin, beta-blockers, ACE inhibitors, and aggressive risk factor control.