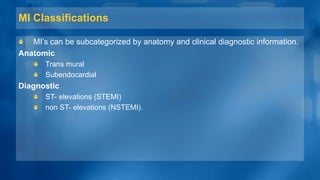
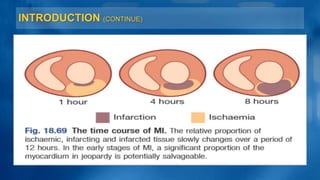
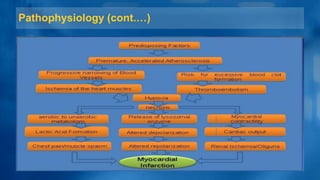
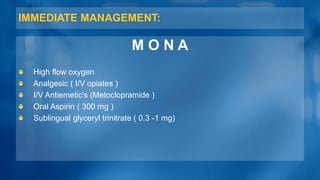
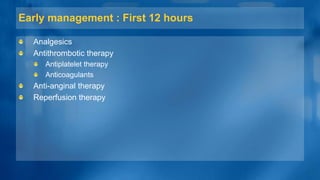
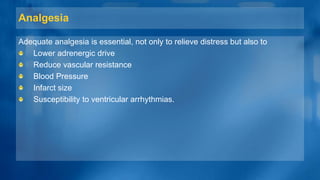
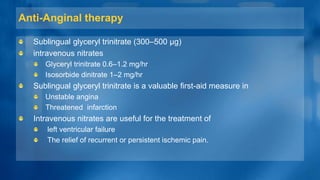
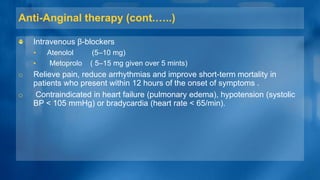
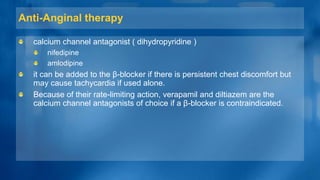
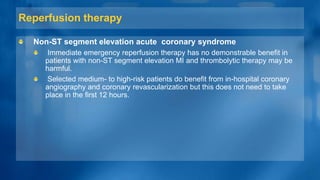
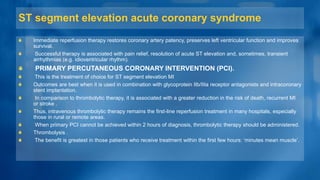
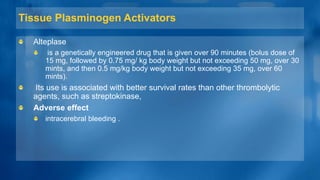
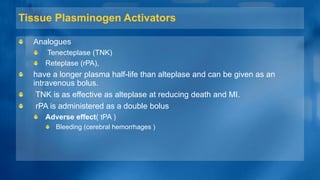
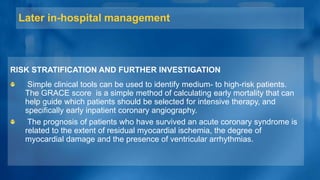
This document presents information on the management of myocardial infarction presented by several students. It discusses immediate management including oxygen, analgesics, antiemetics and aspirin. Early management within the first 12 hours includes analgesics, antithrombotic therapy with antiplatelet drugs like aspirin and clopidogrel as well as anticoagulants. It also discusses anti-anginal therapy and reperfusion therapy.