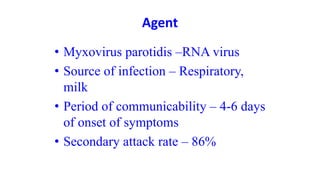
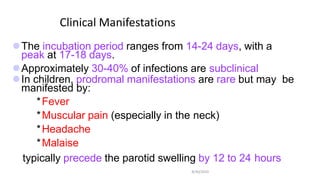
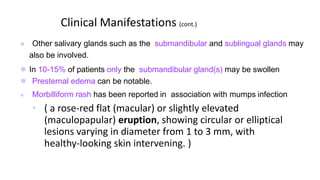
Mumps is a viral infection that causes swelling of the salivary glands. It is caused by the mumps virus and primarily affects children aged 5-15 years old. Common symptoms include fever and swelling of the parotid glands near the ears. Complications can include meningitis, deafness, orchitis, and oophoritis. Treatment focuses on relieving symptoms and prevention is achieved through the MMR vaccine.