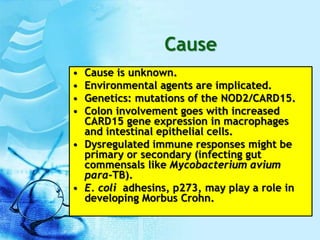
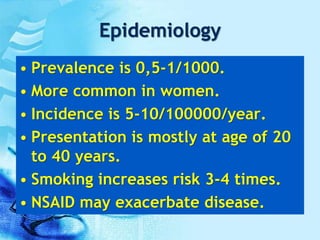
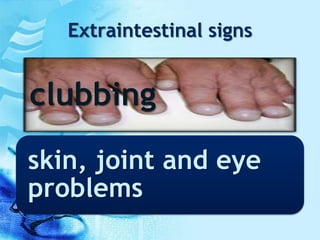
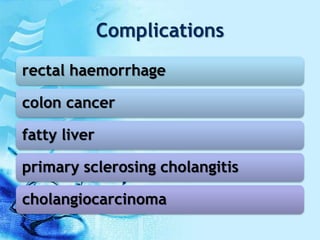
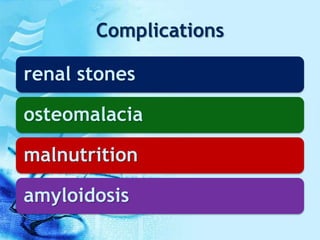
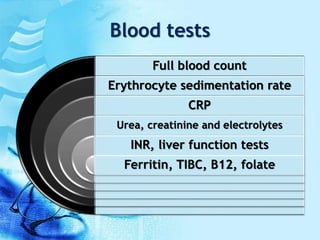
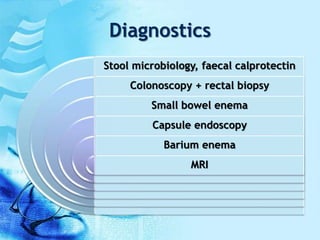
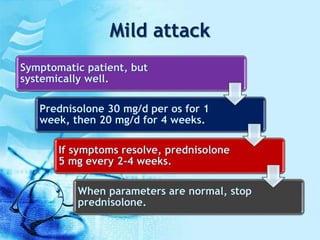
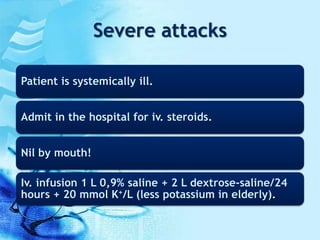
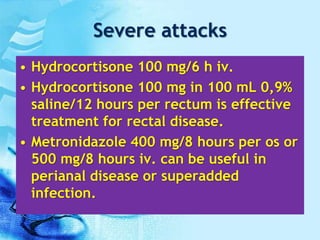
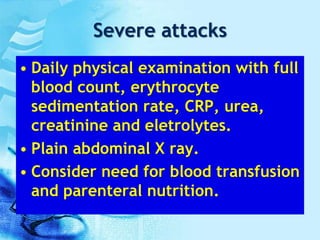
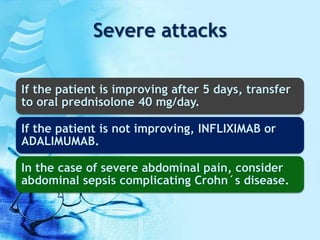
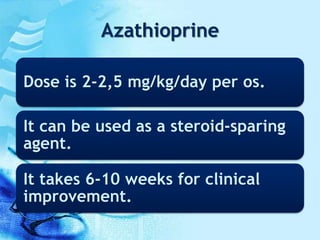
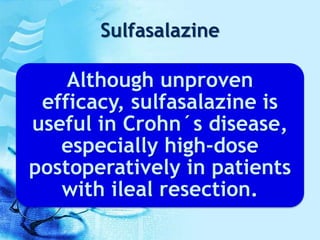
This document provides information on Crohn's disease, including that it is a chronic inflammatory bowel disease characterized by transmural inflammation that can affect any part of the digestive tract. The cause is unknown but likely involves genetic and environmental factors. Symptoms include diarrhea, abdominal pain, weight loss and fever. Complications can include bowel obstruction, abscesses, and fistulas. Diagnosis involves blood tests, stool samples, endoscopy, and imaging. Treatment depends on severity but may include medications like corticosteroids, immunosuppressants, TNF-alpha inhibitors, antibiotics, and nutritional support.