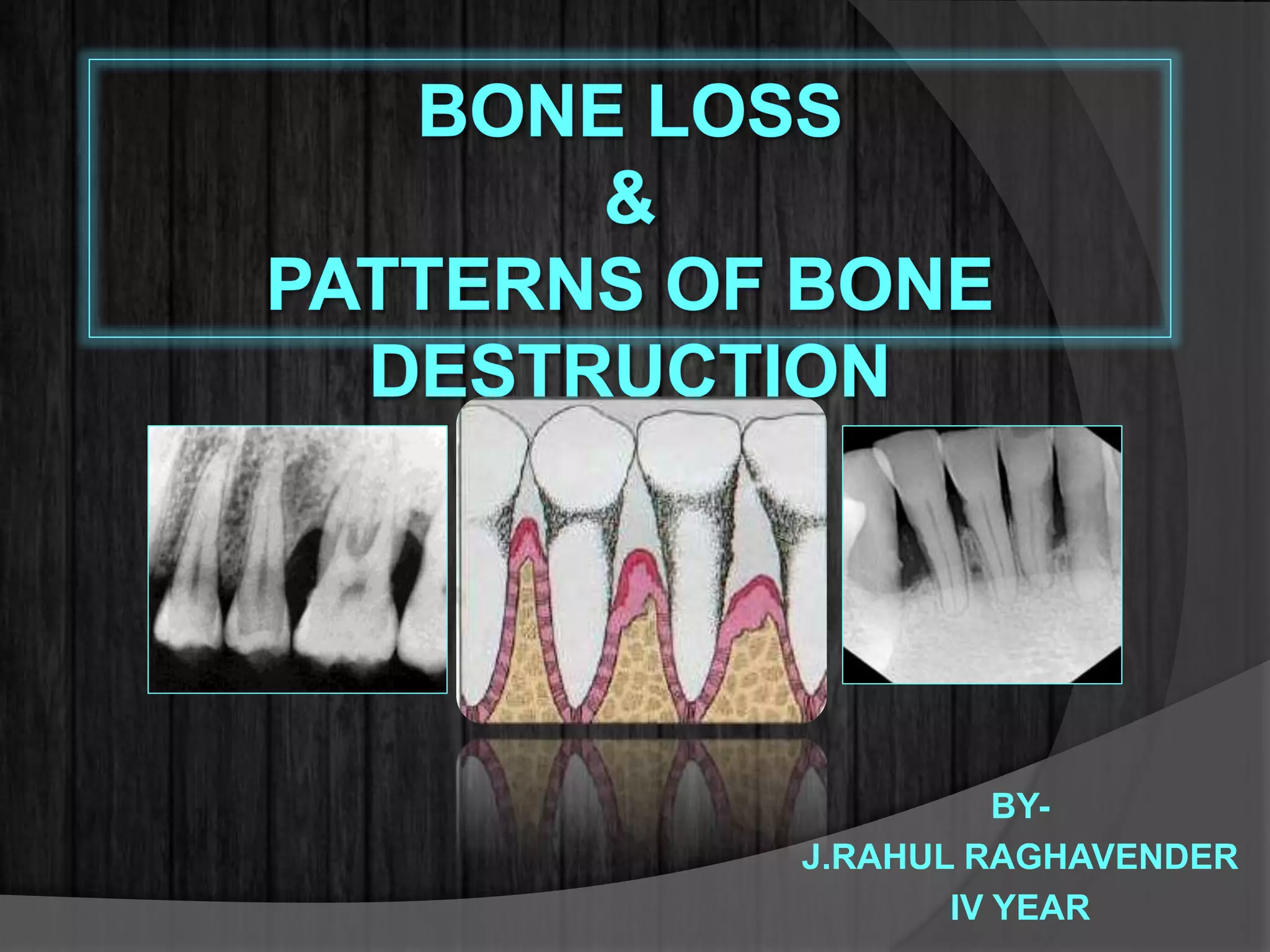
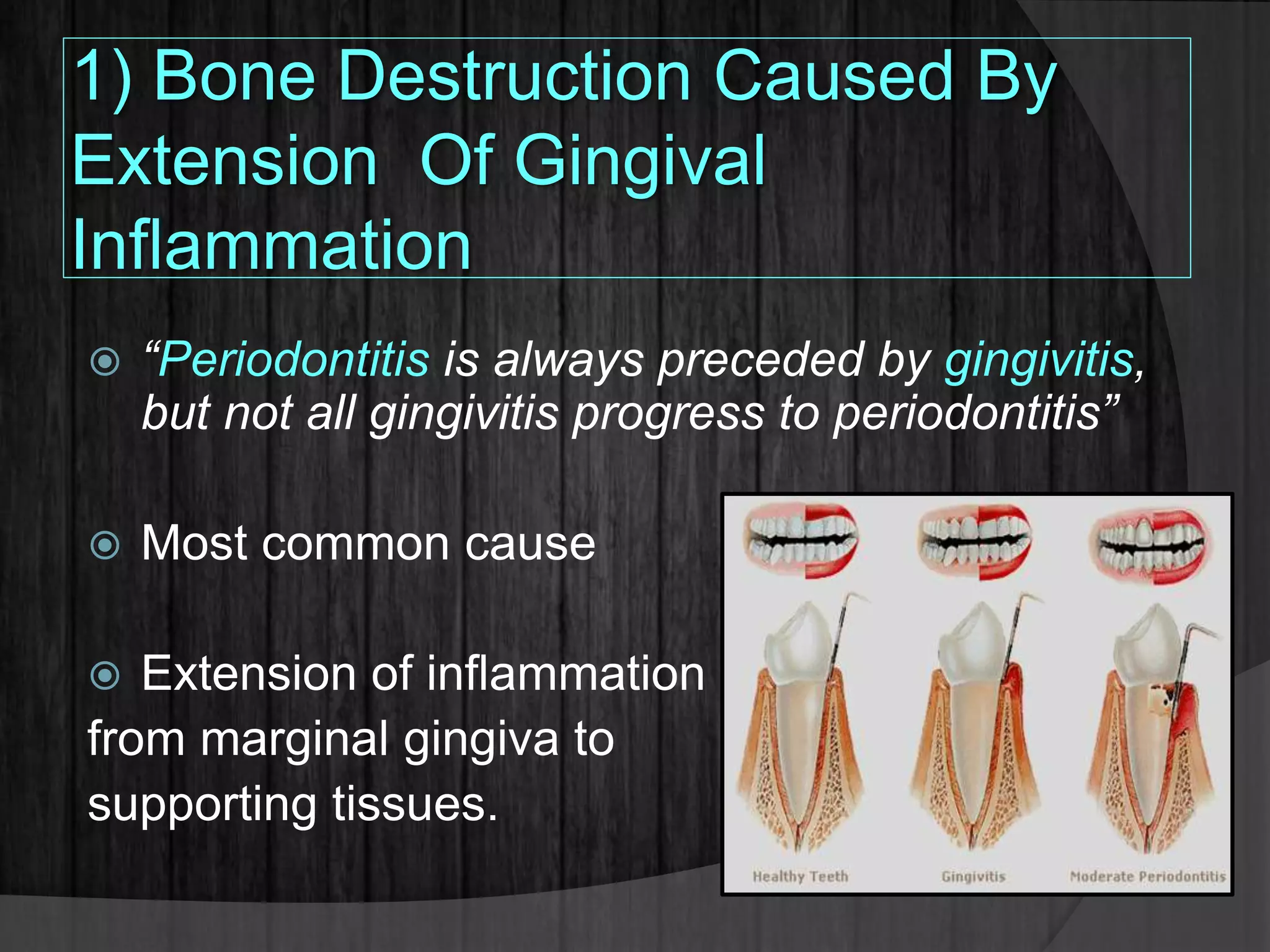
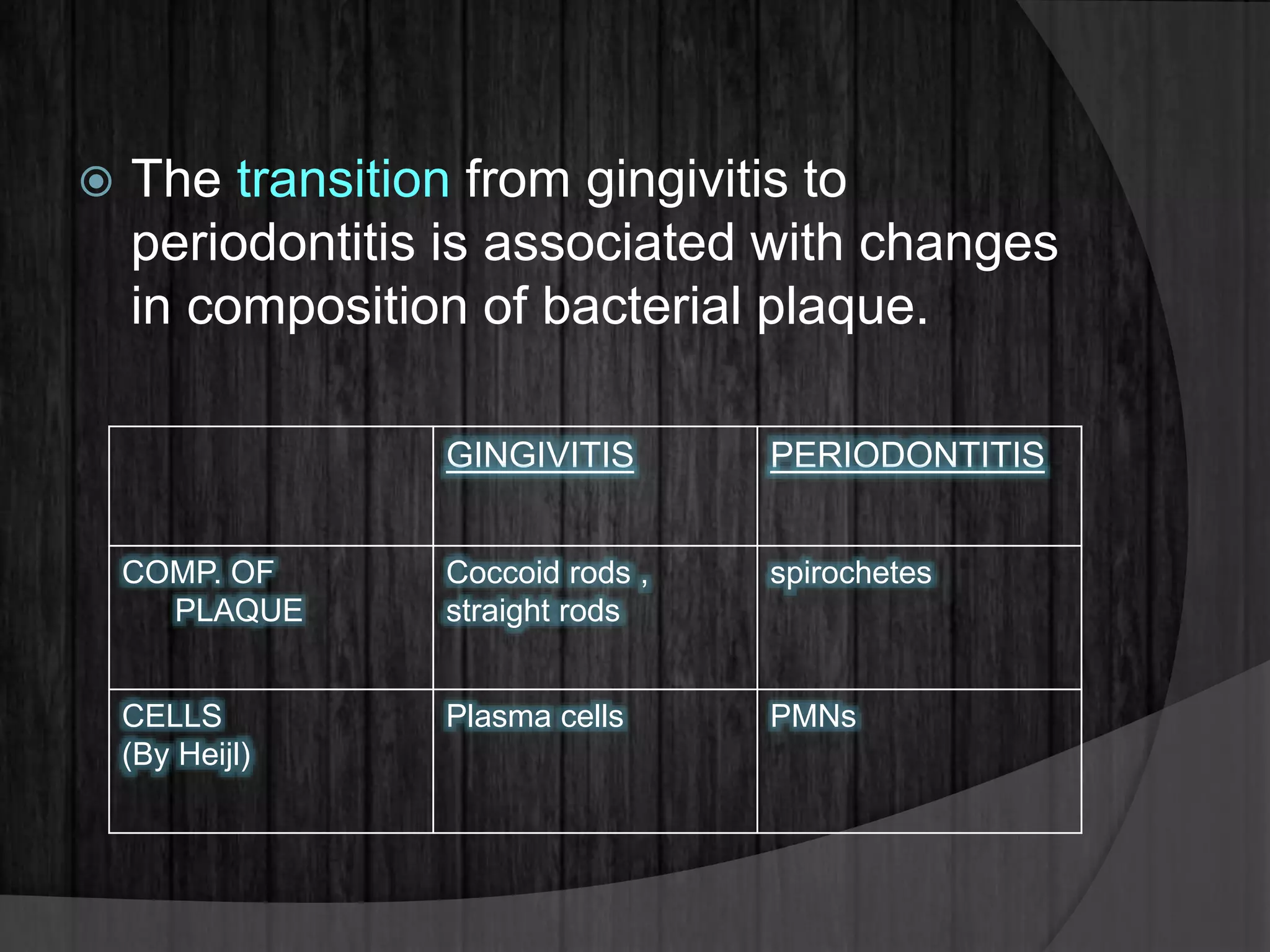
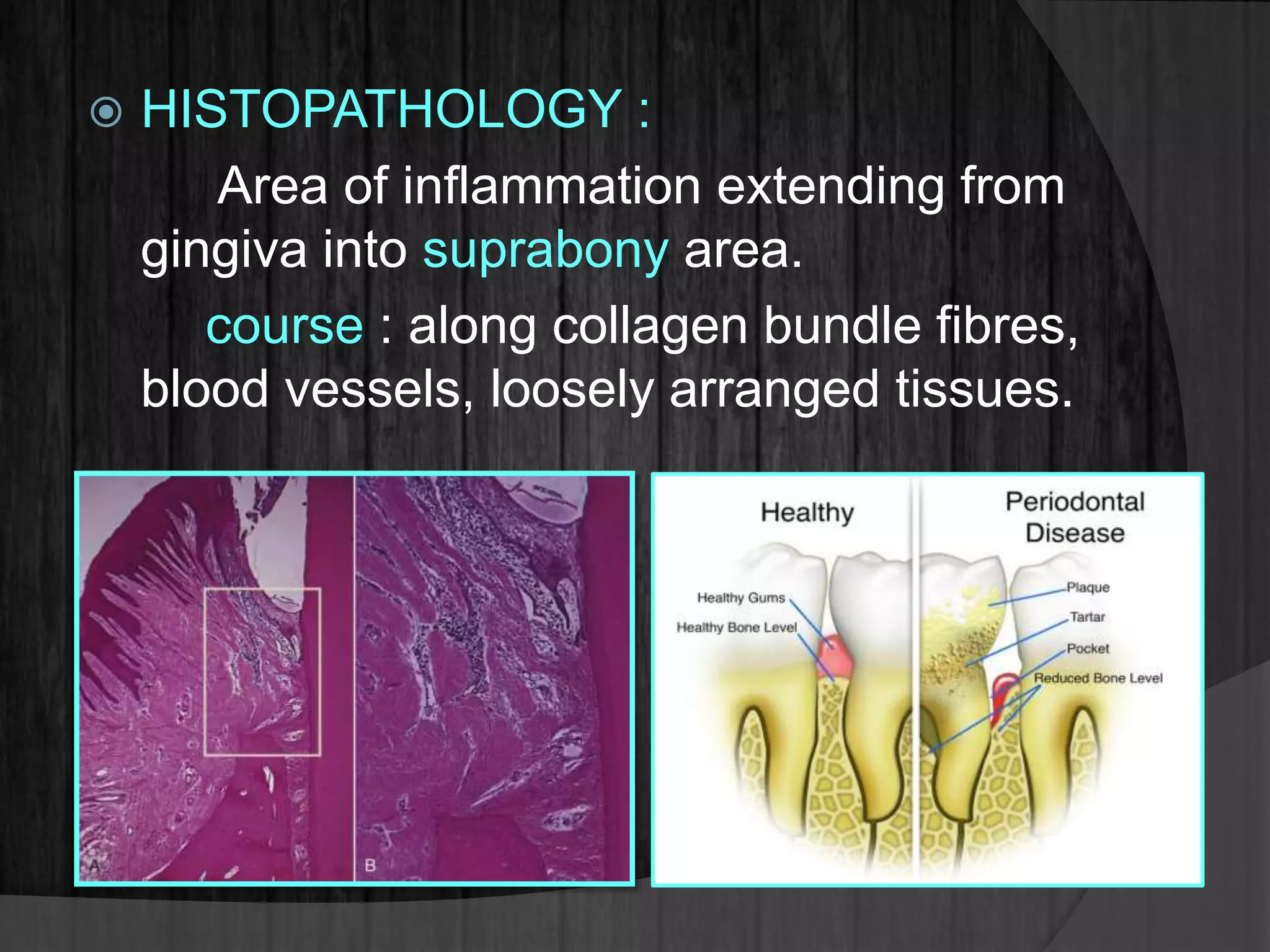
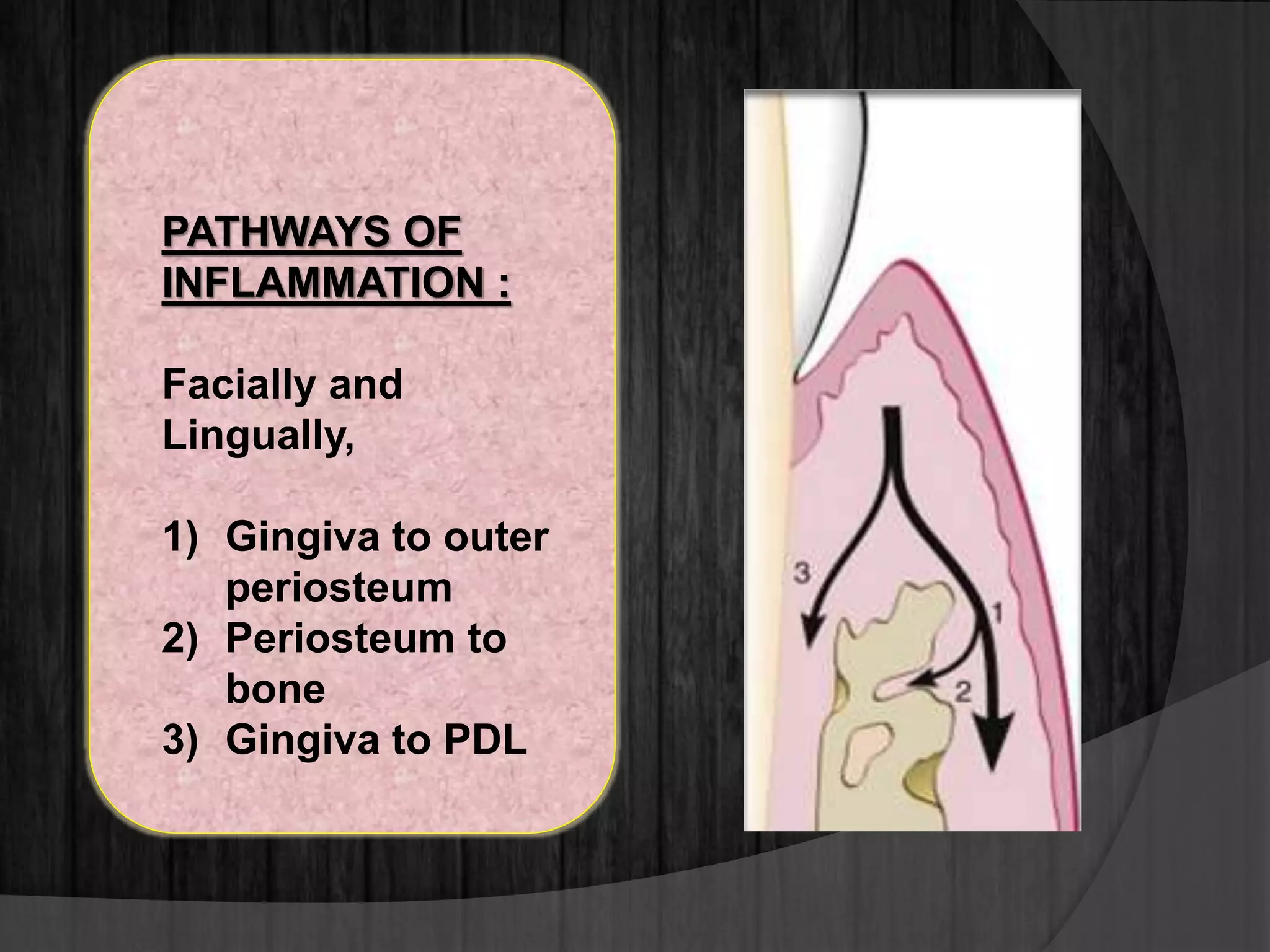
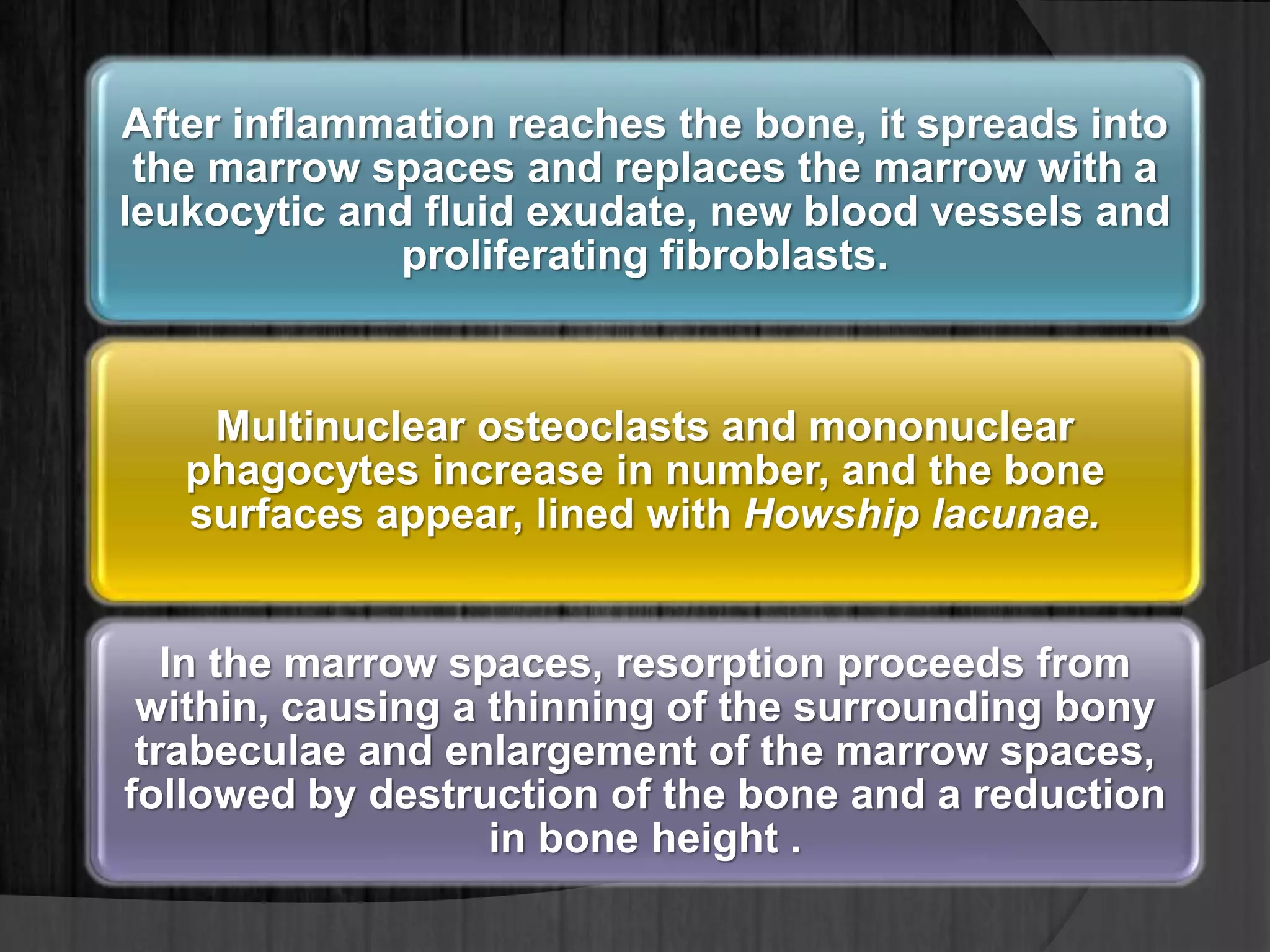
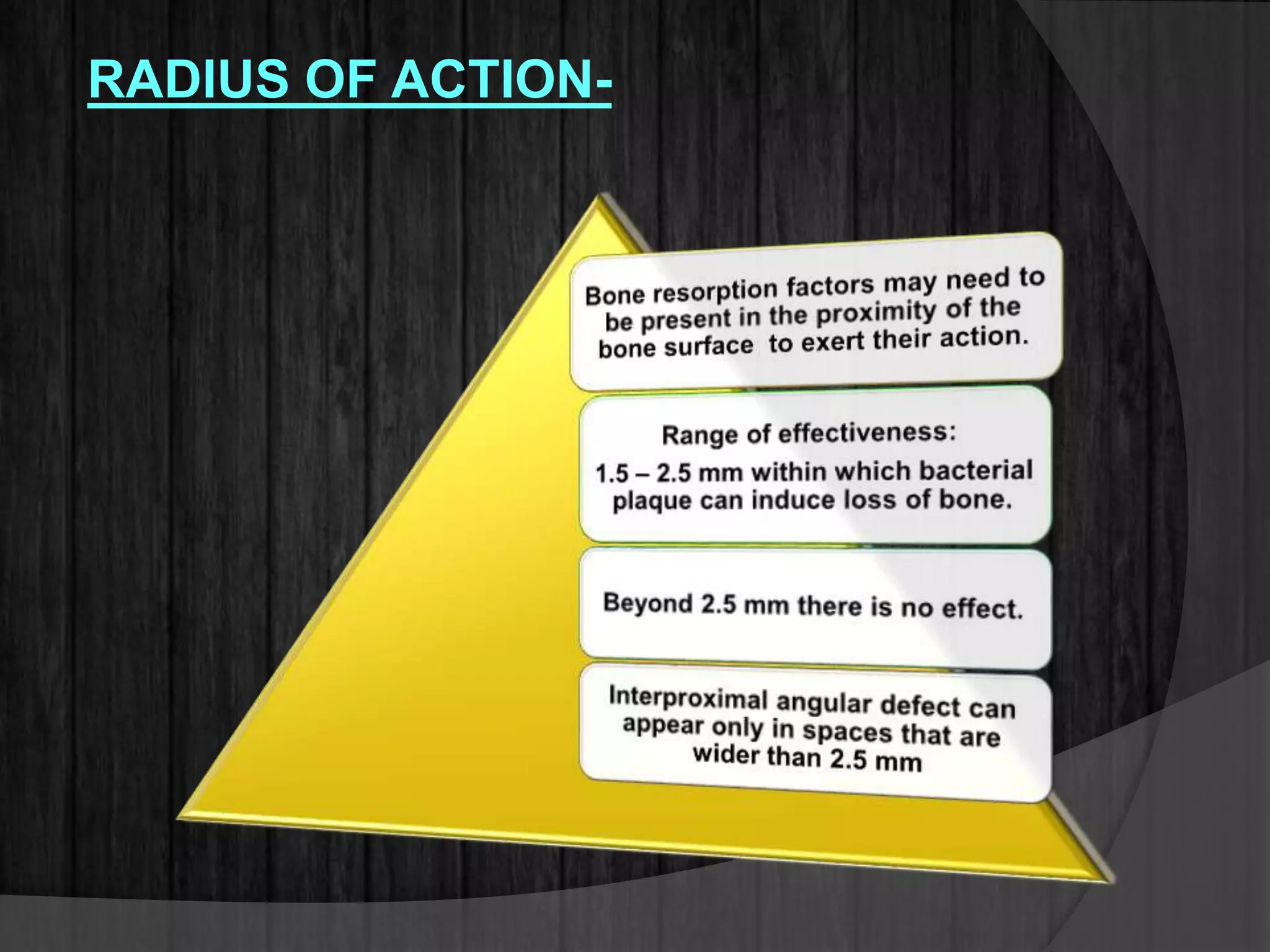
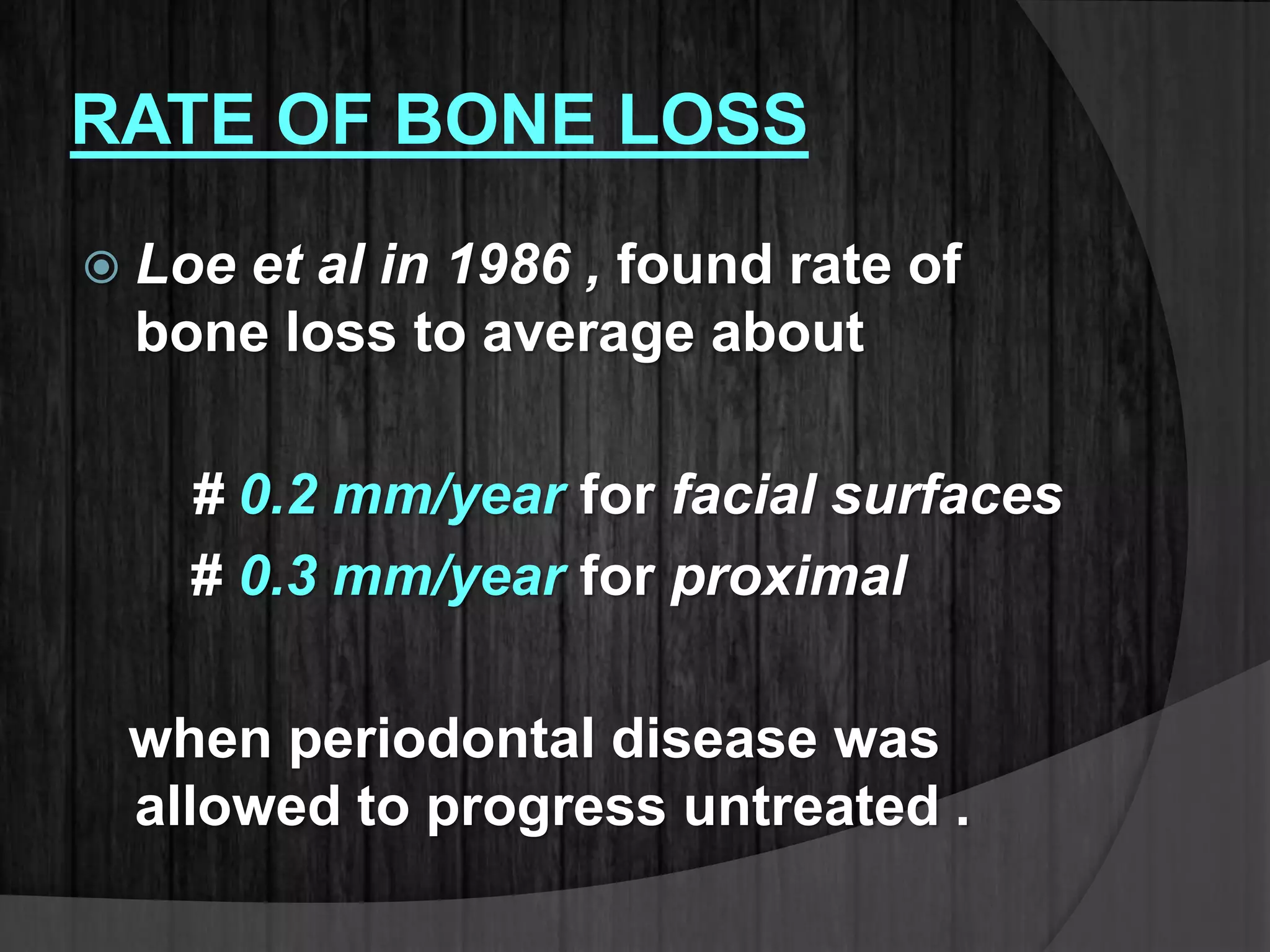
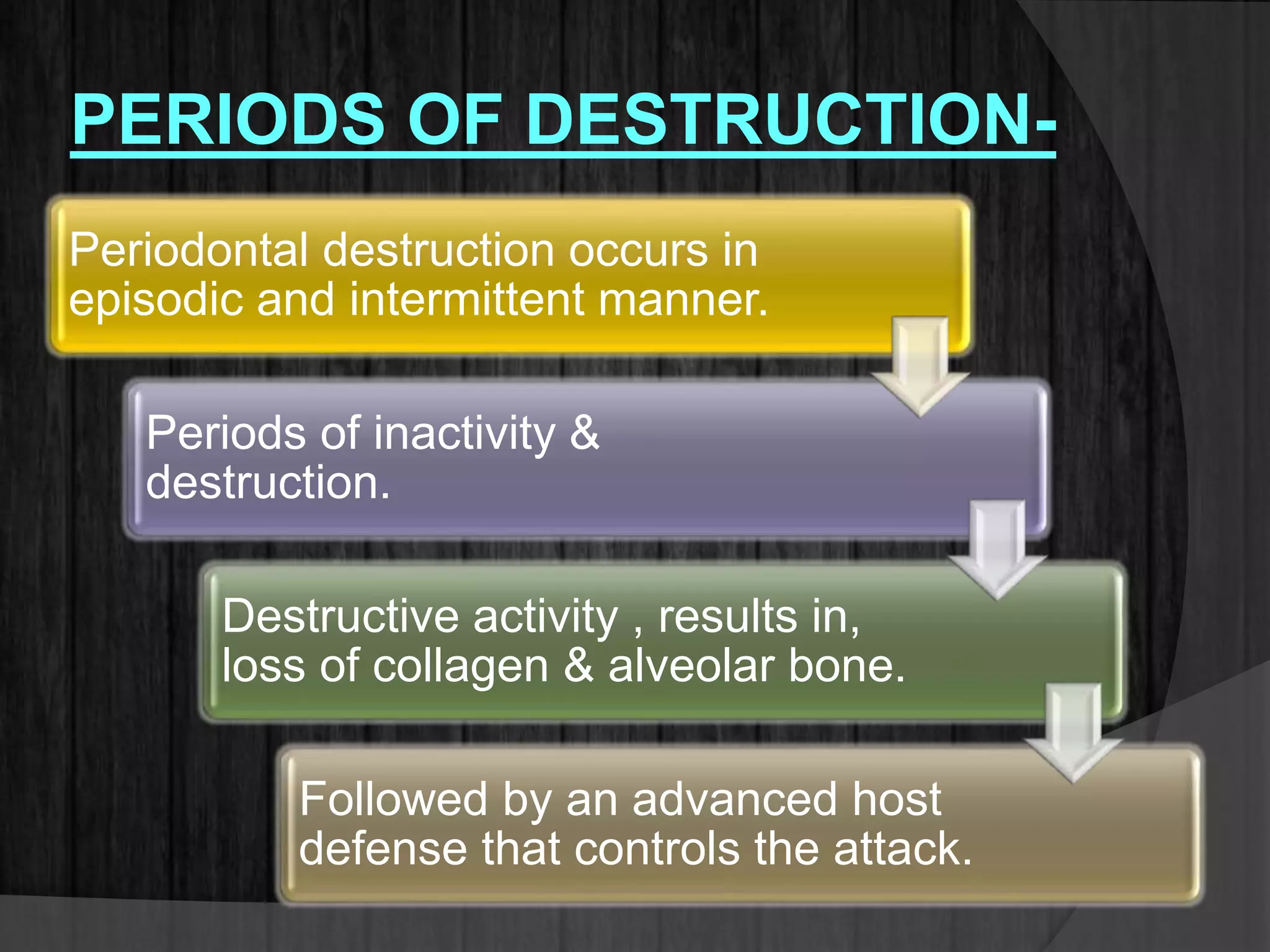
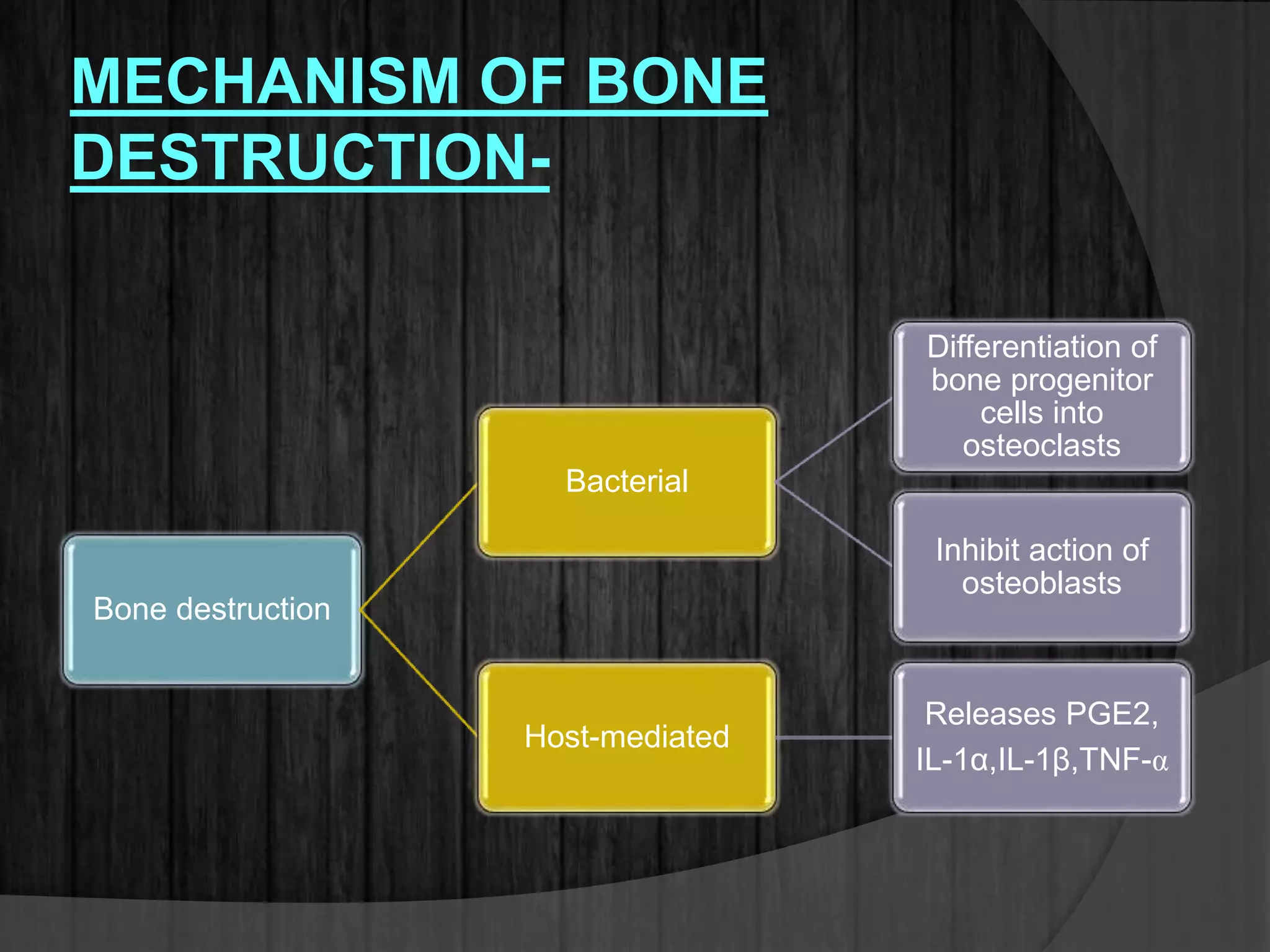
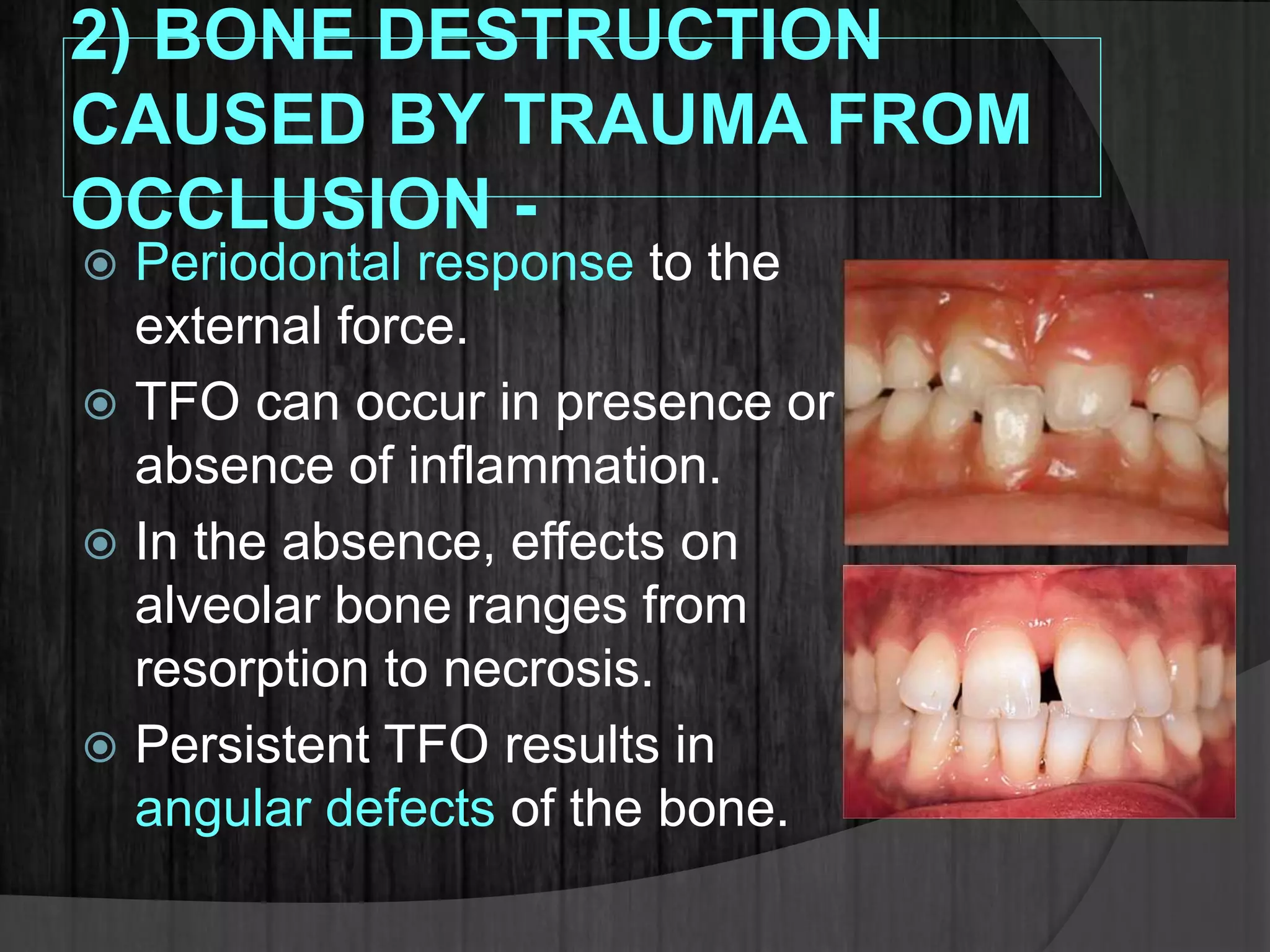
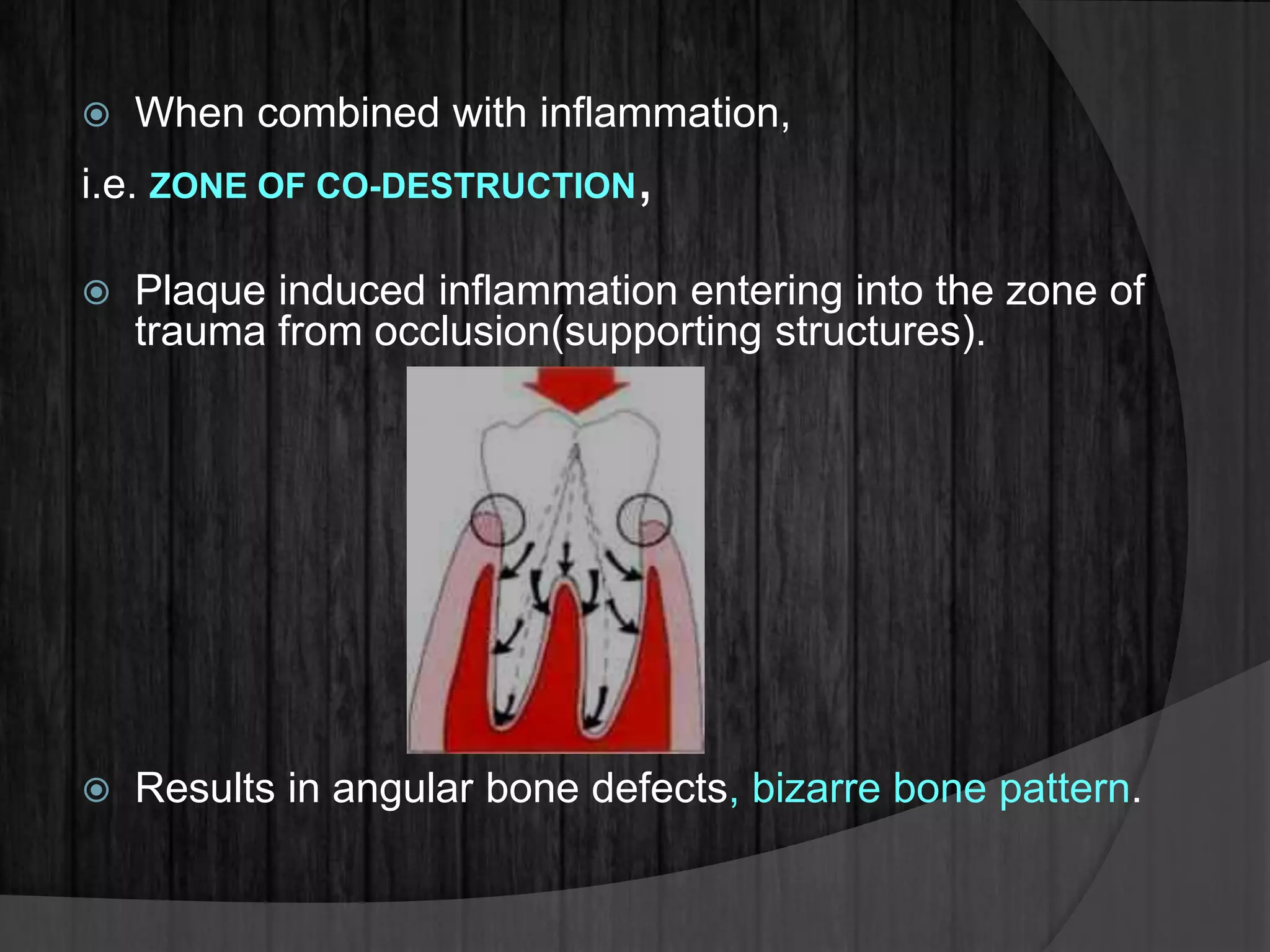
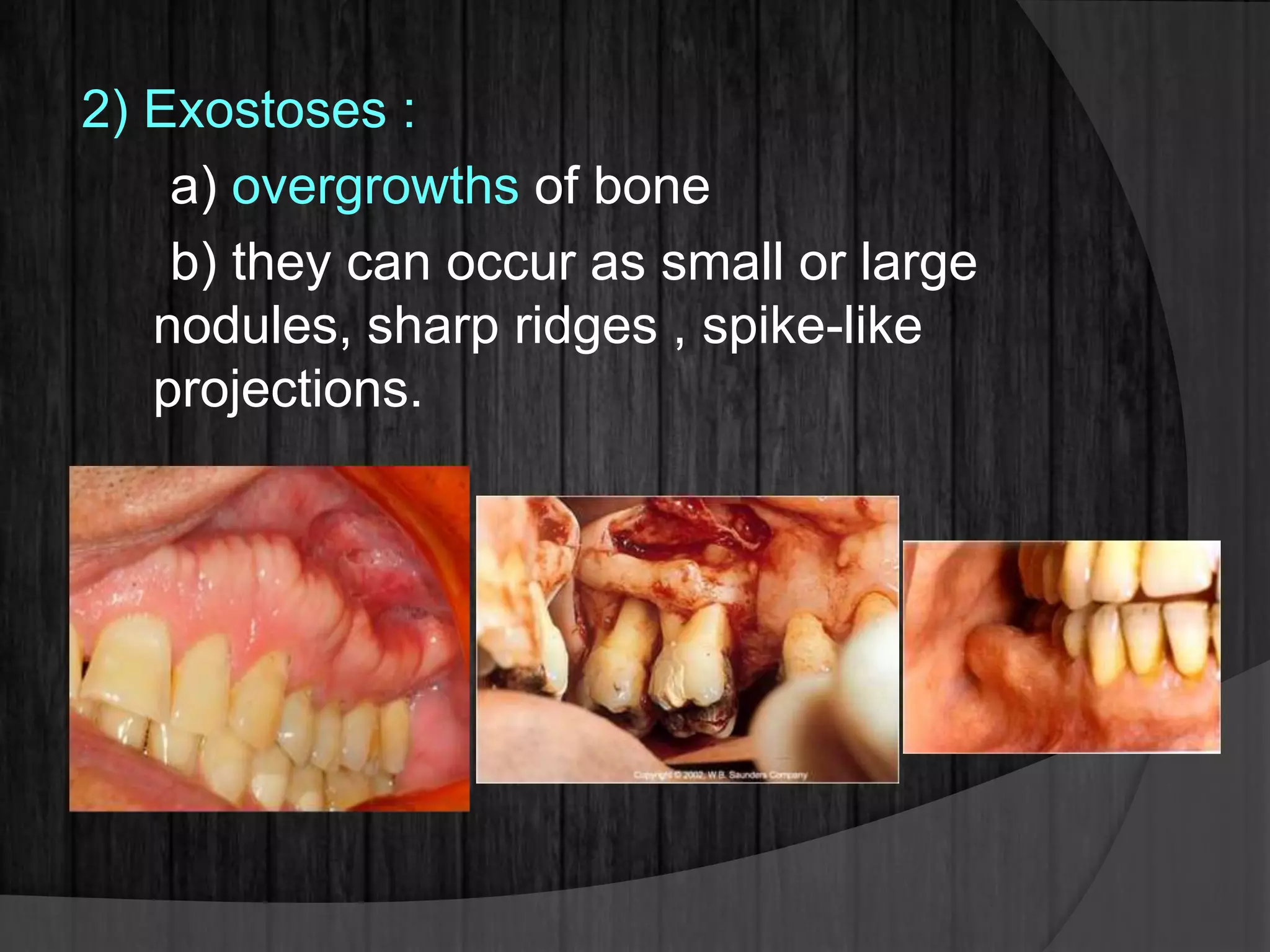
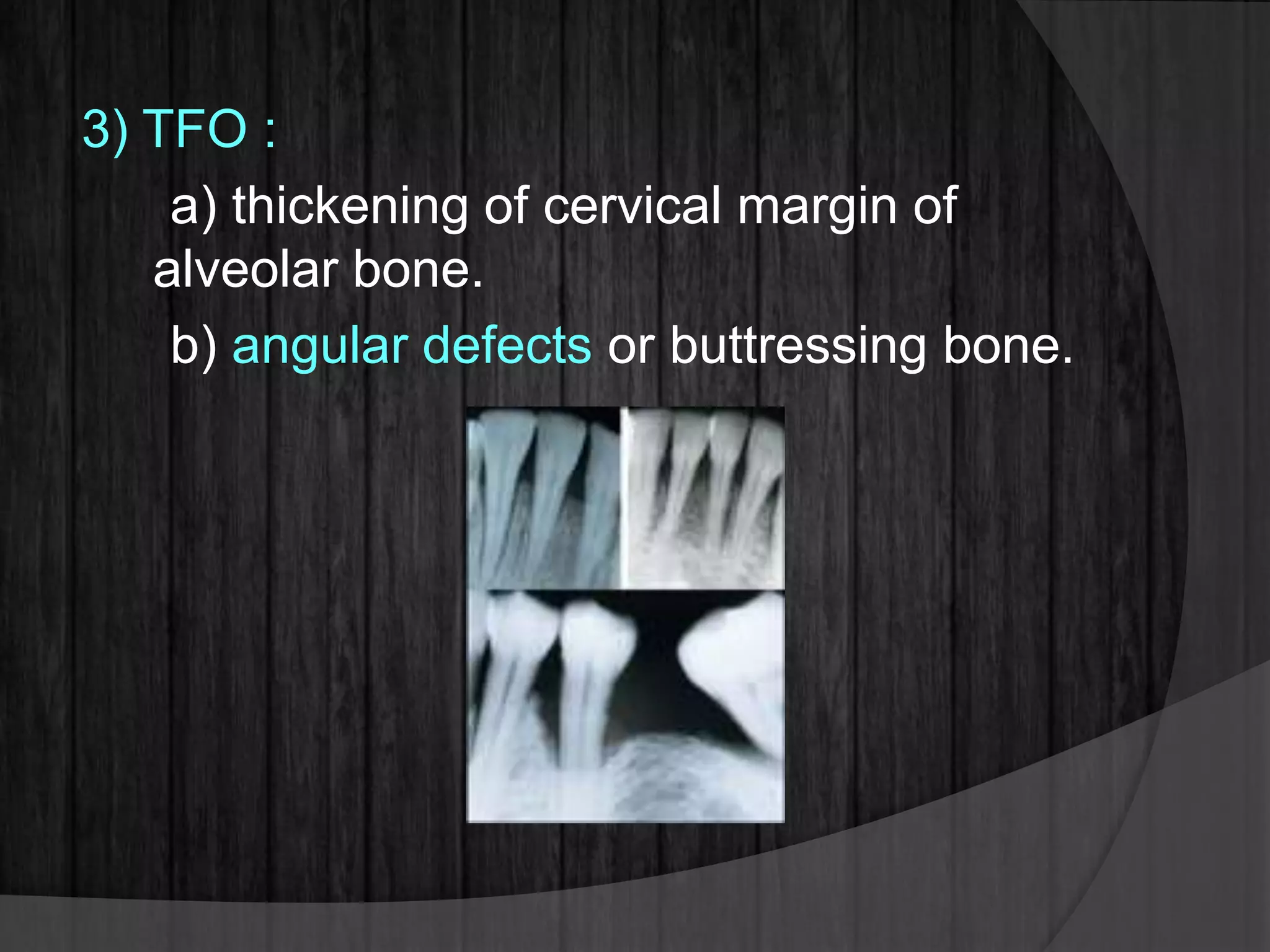
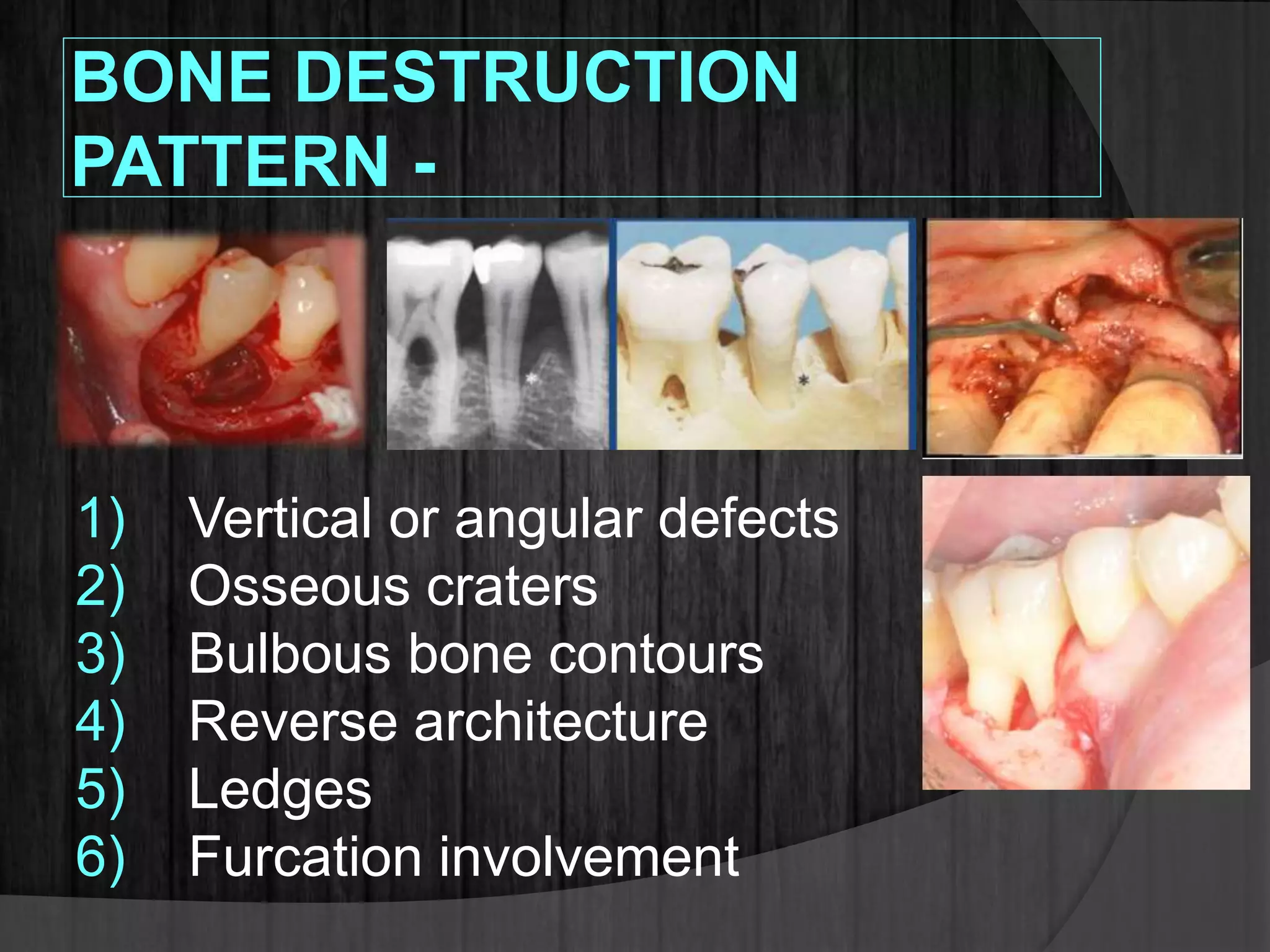
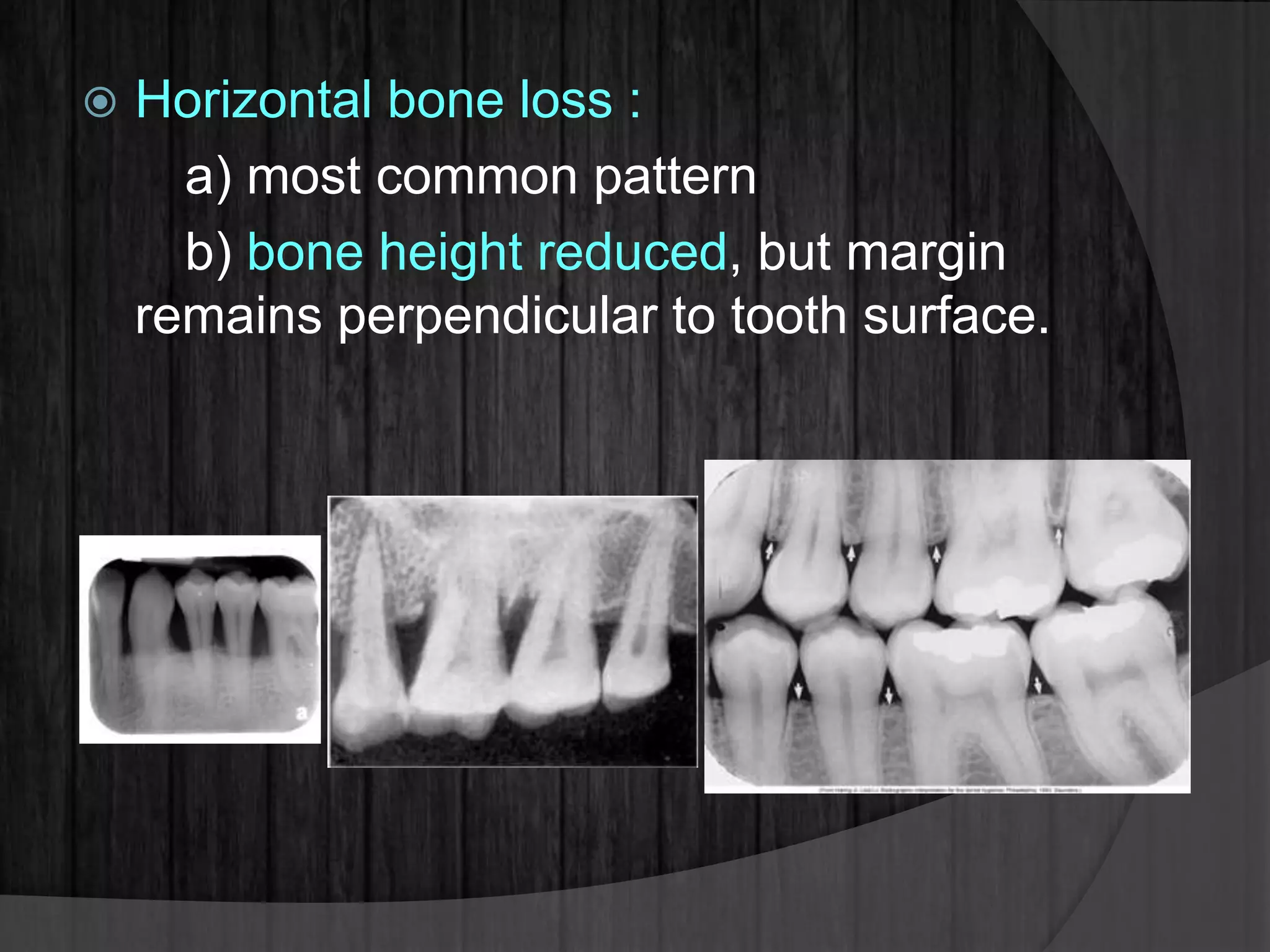
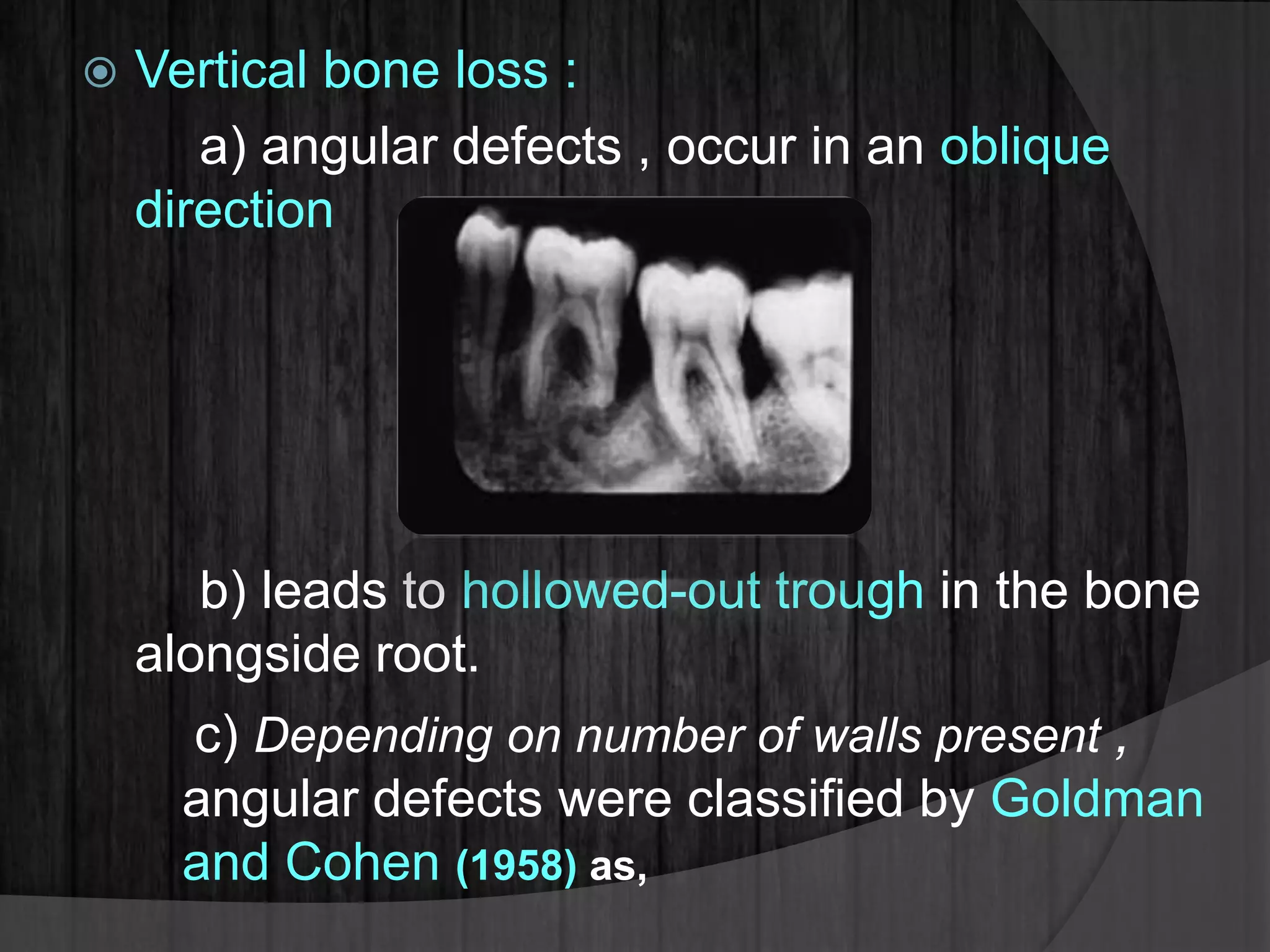
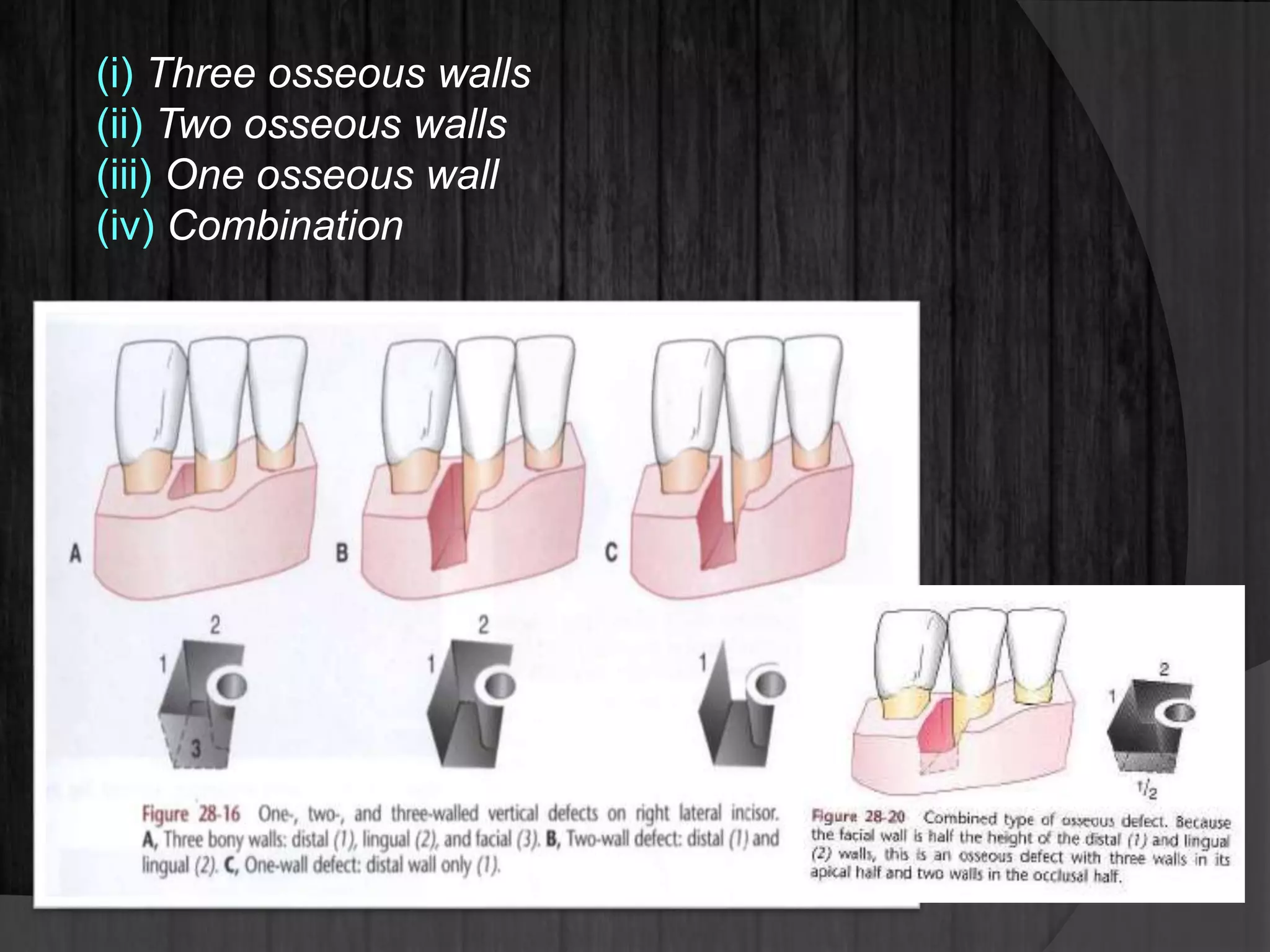
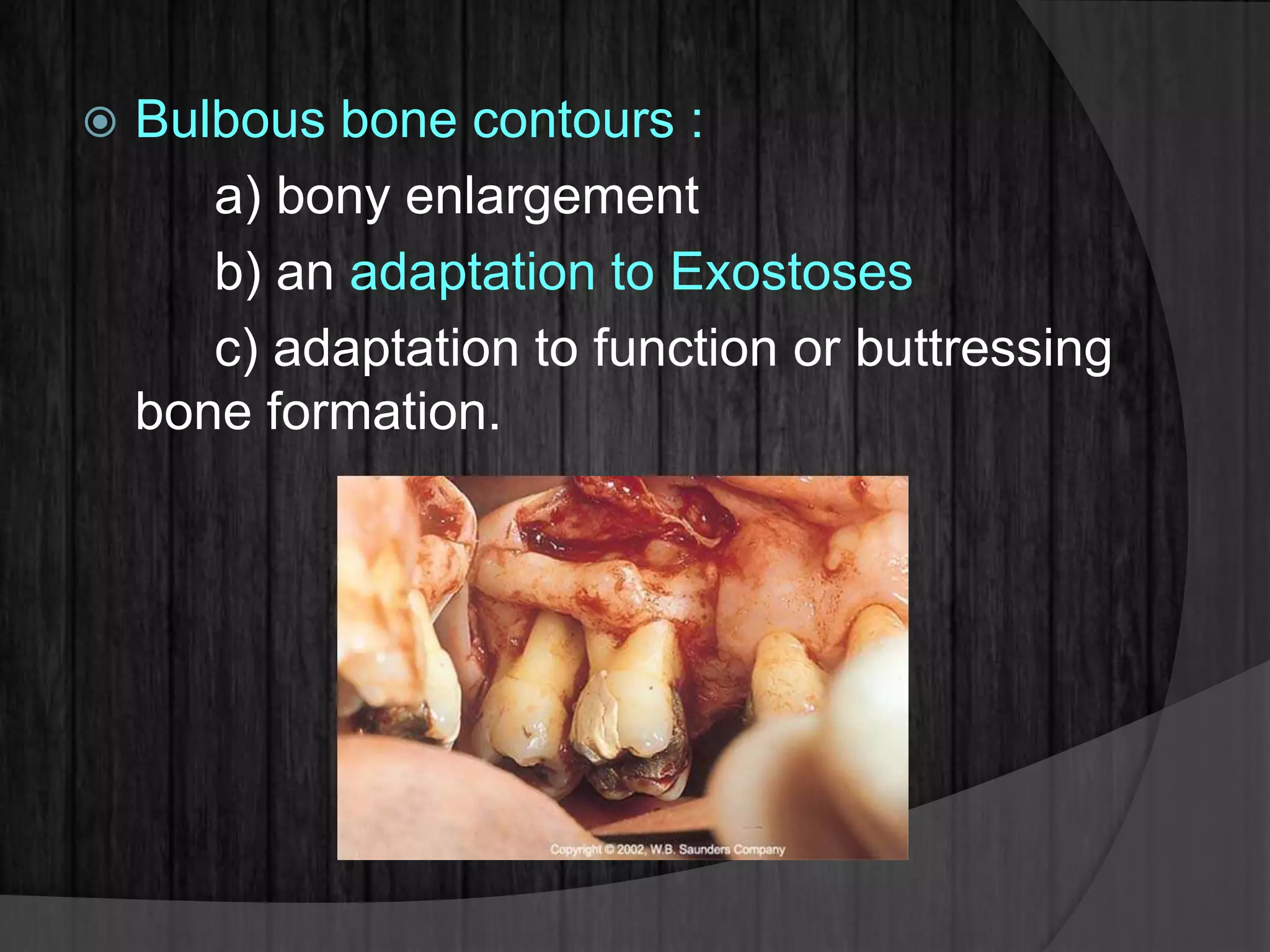
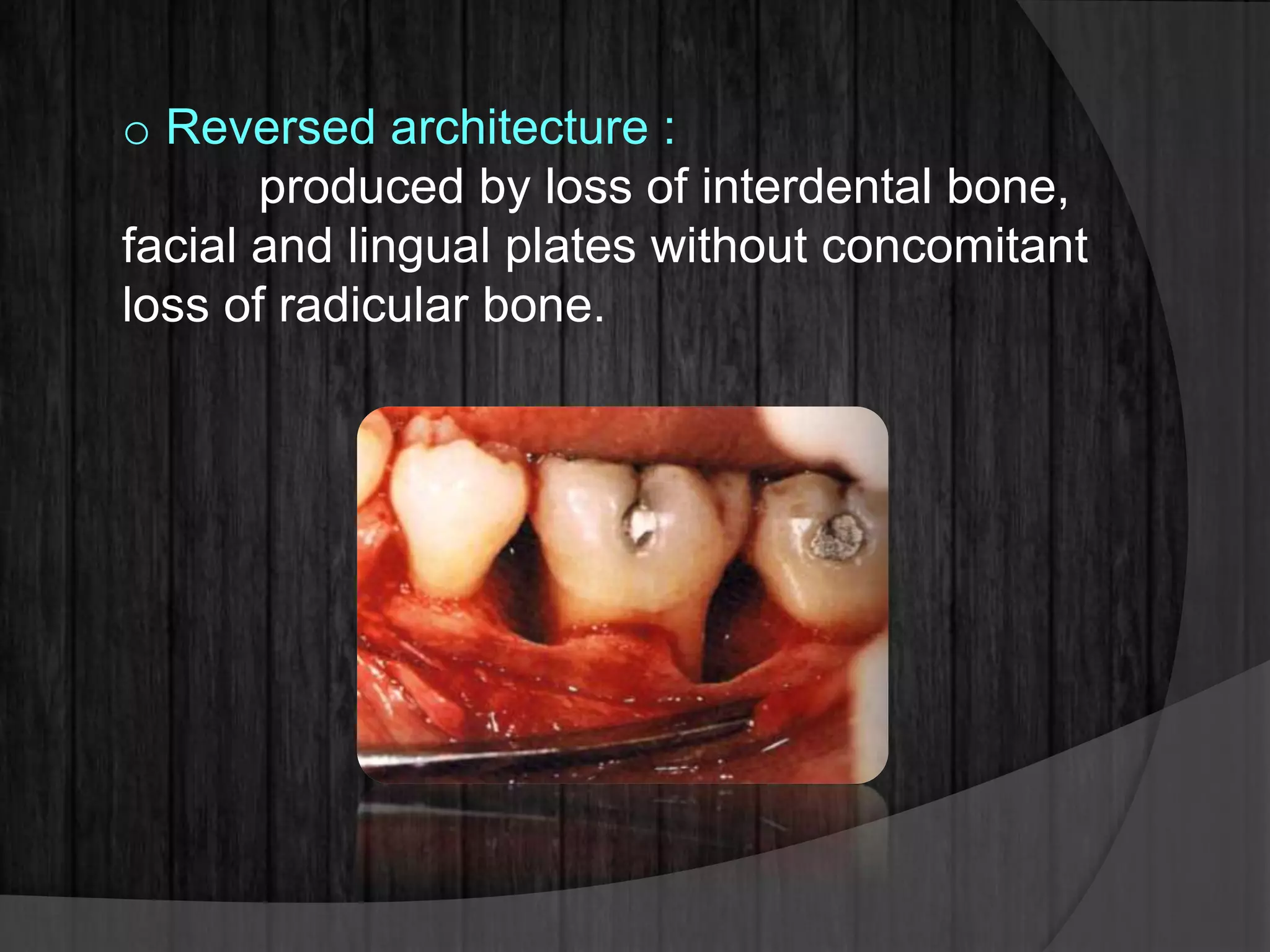
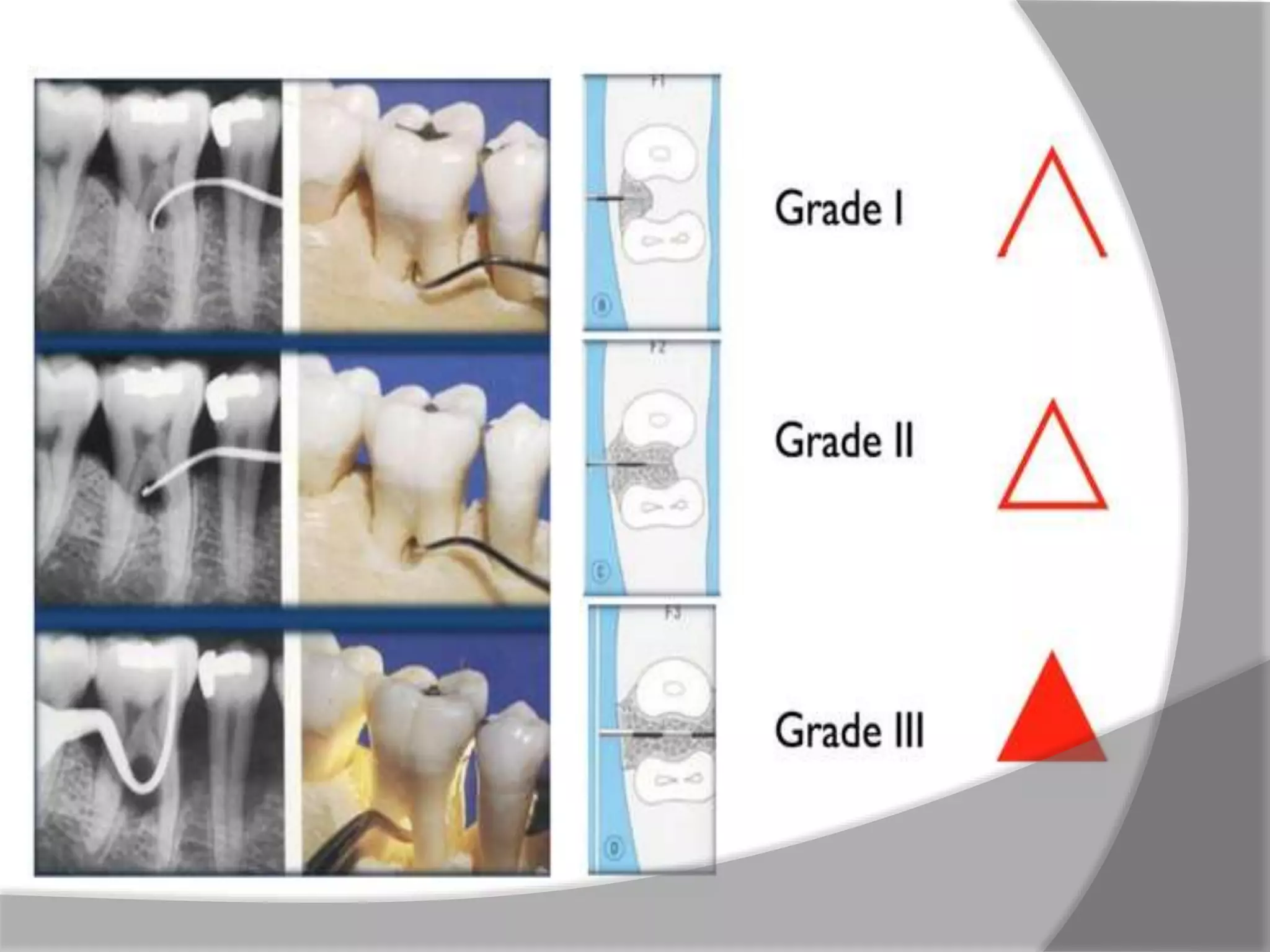
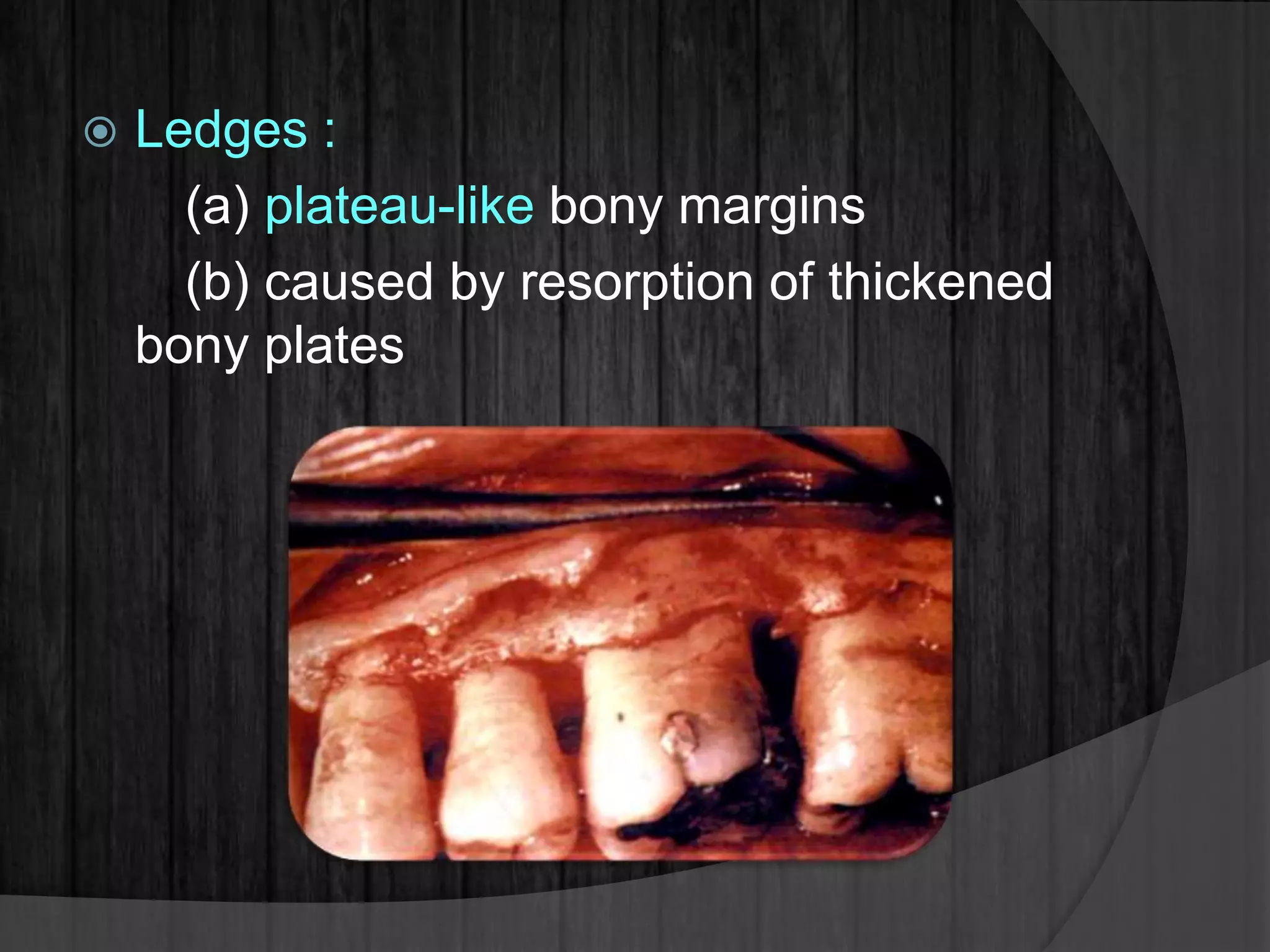
This document discusses bone destruction patterns caused by periodontal disease. It identifies the main causes of bone destruction as the extension of gingival inflammation, trauma from occlusion, and systemic disorders. It describes several patterns of bone loss seen in periodontal disease, including horizontal, vertical, osseous craters, bulbous contours, reversed architecture, ledges, and furcation involvement. The rate and episodic nature of bone destruction in periodontal disease is also covered.