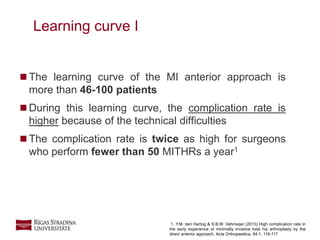
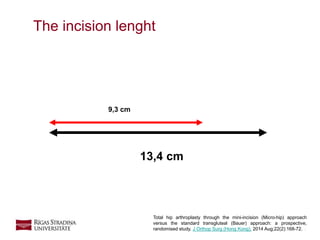
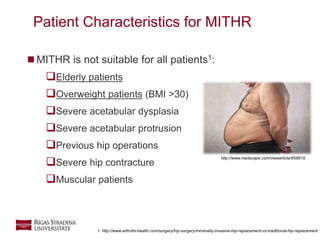
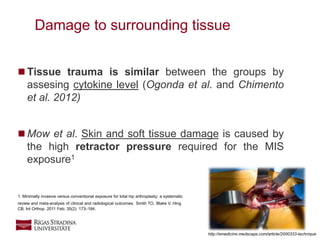
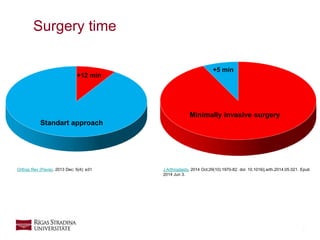
Minimally invasive total hip replacement (MITHR) uses a smaller incision of 6-10 cm compared to the standard incision. While MITHR results in less soft tissue damage and shorter hospital stays, it also has a longer learning curve for surgeons. Early in the learning curve, complication rates are higher for MITHR. With increased experience, surgeons can perform MITHR with outcomes equivalent to conventional THR. However, the evidence does not clearly support making MITHR the standard procedure over the conventional approach. Patient characteristics and surgeon experience should guide the choice of surgical approach.


![16
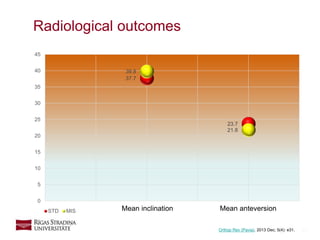
6 weeks – 2 years after surgery
0
1
2
3
4
5
6
7
8
9
10
6 weeks 12 weeks 1 year 2 years
VAS pain at motion 1.5 1 0 0
Harris 7.7 9.1 9.6 9.9
VAS satisfaction 9.6 9.6 10 10
Standart lateral
VAS pain at motion Harris VAS satisfaction
Orthop Rev (Pavia). 2013 Dec; 5(4): e31.
[0-10] [0-10] [0-10]](https://image.slidesharecdn.com/mithr-2-gala-variants-161210204820/85/Minimally-invasive-total-hip-replacement-16-320.jpg)
![17
0
1
2
3
4
5
6
7
8
9
10
6 weeks 12 weeks 1 year 2 years
VAS pain at motion 1 0 0 0
Harris 8.3 9.5 9.9 9.9
VAS satisfaction 10 10 10 10
Minimally invasive
VAS pain at motion Harris VAS satisfaction
6 weeks – 2 years after surgery
Orthop Rev (Pavia). 2013 Dec; 5(4): e31.
[0-10] [0-10] [0-10]](https://image.slidesharecdn.com/mithr-2-gala-variants-161210204820/85/Minimally-invasive-total-hip-replacement-17-320.jpg)