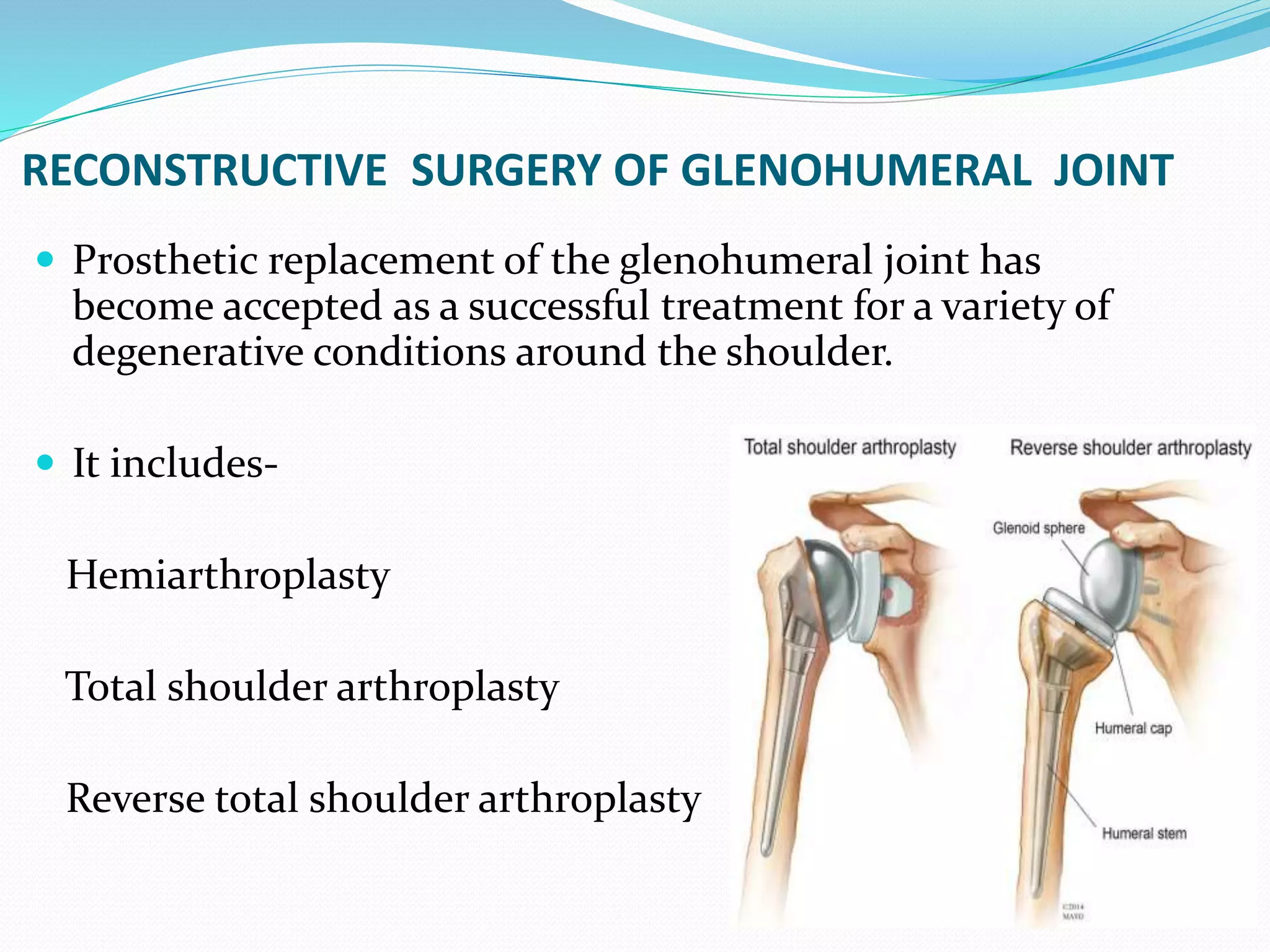
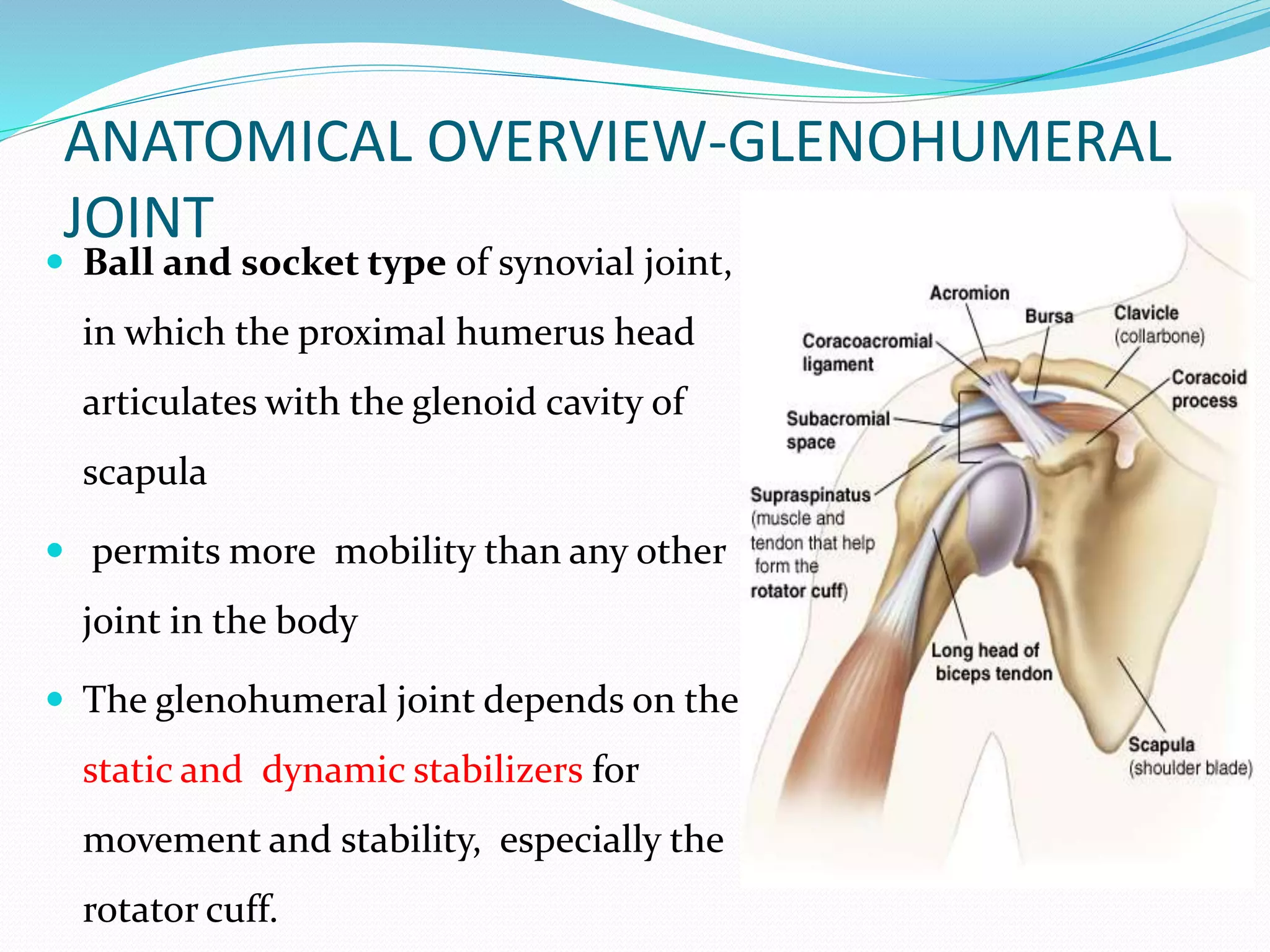
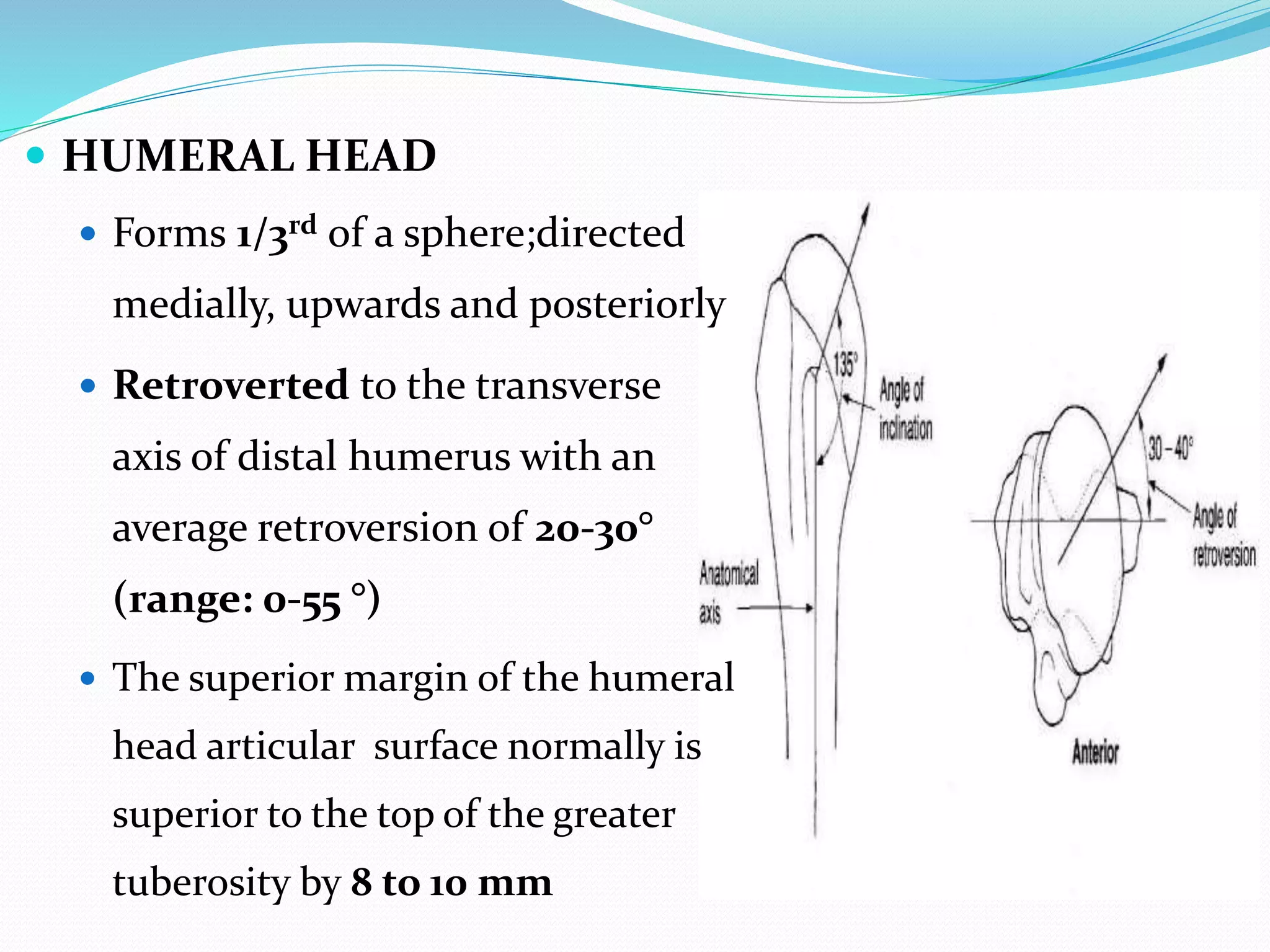
This document discusses reconstructive surgery of the glenohumeral joint, including reverse total shoulder arthroplasty. It provides an anatomical overview of the glenohumeral joint and describes the indications, surgical procedure, components, and complications of reverse total shoulder arthroplasty. Reverse total shoulder arthroplasty involves replacing the normal ball and socket articulation with a convex glenoid component and concave humeral cup to improve function and range of motion, especially for conditions involving rotator cuff dysfunction.