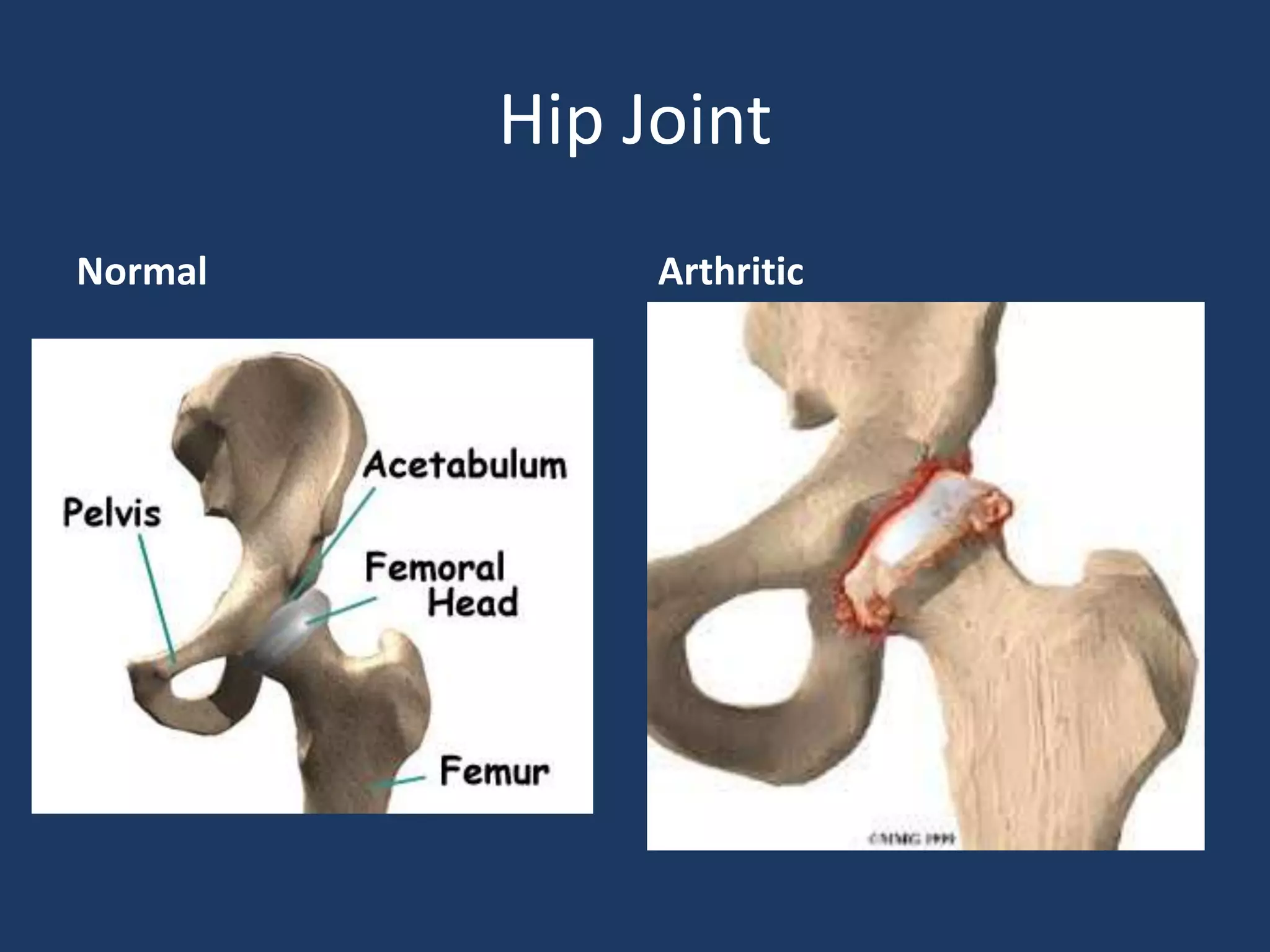
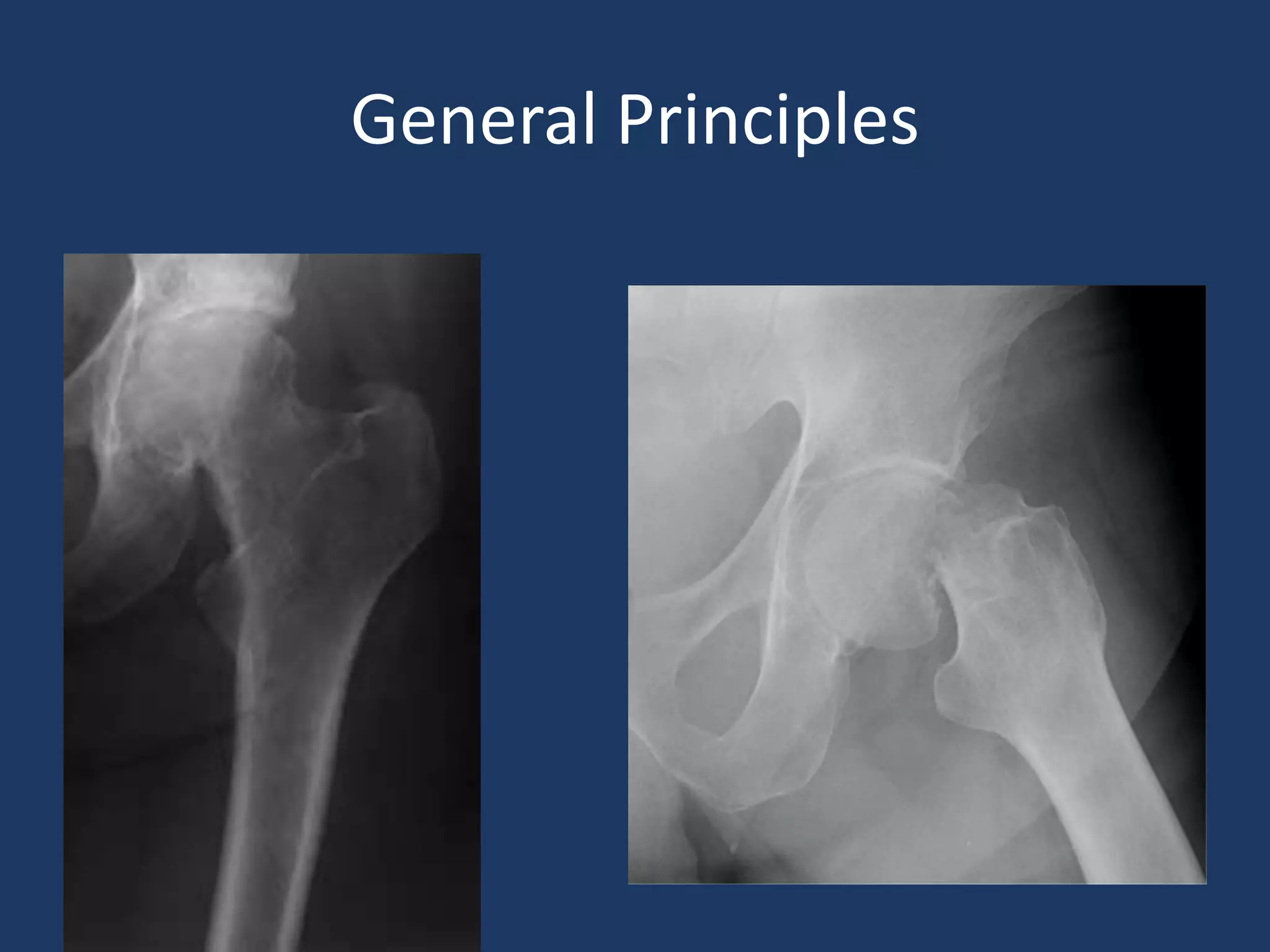
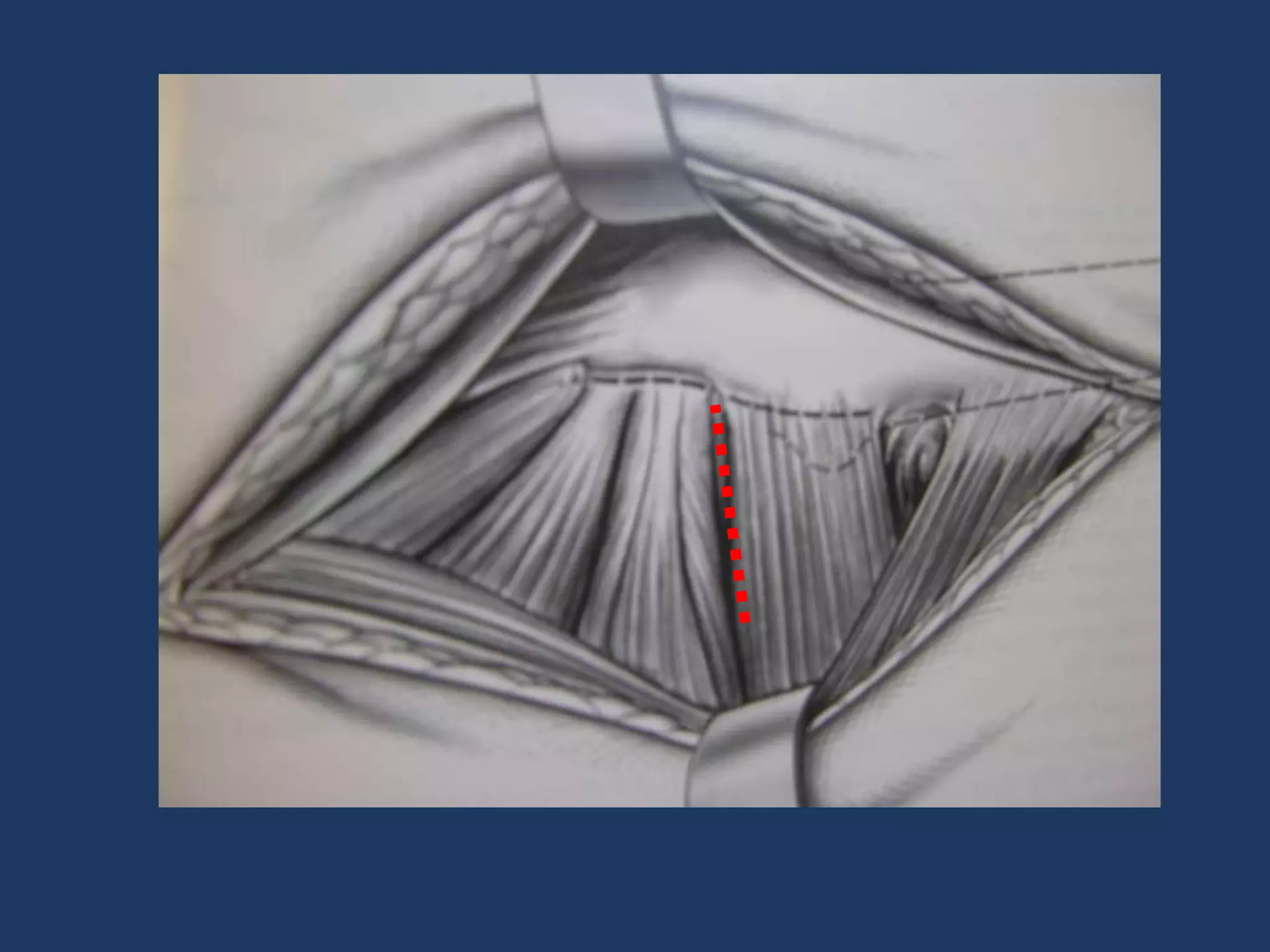
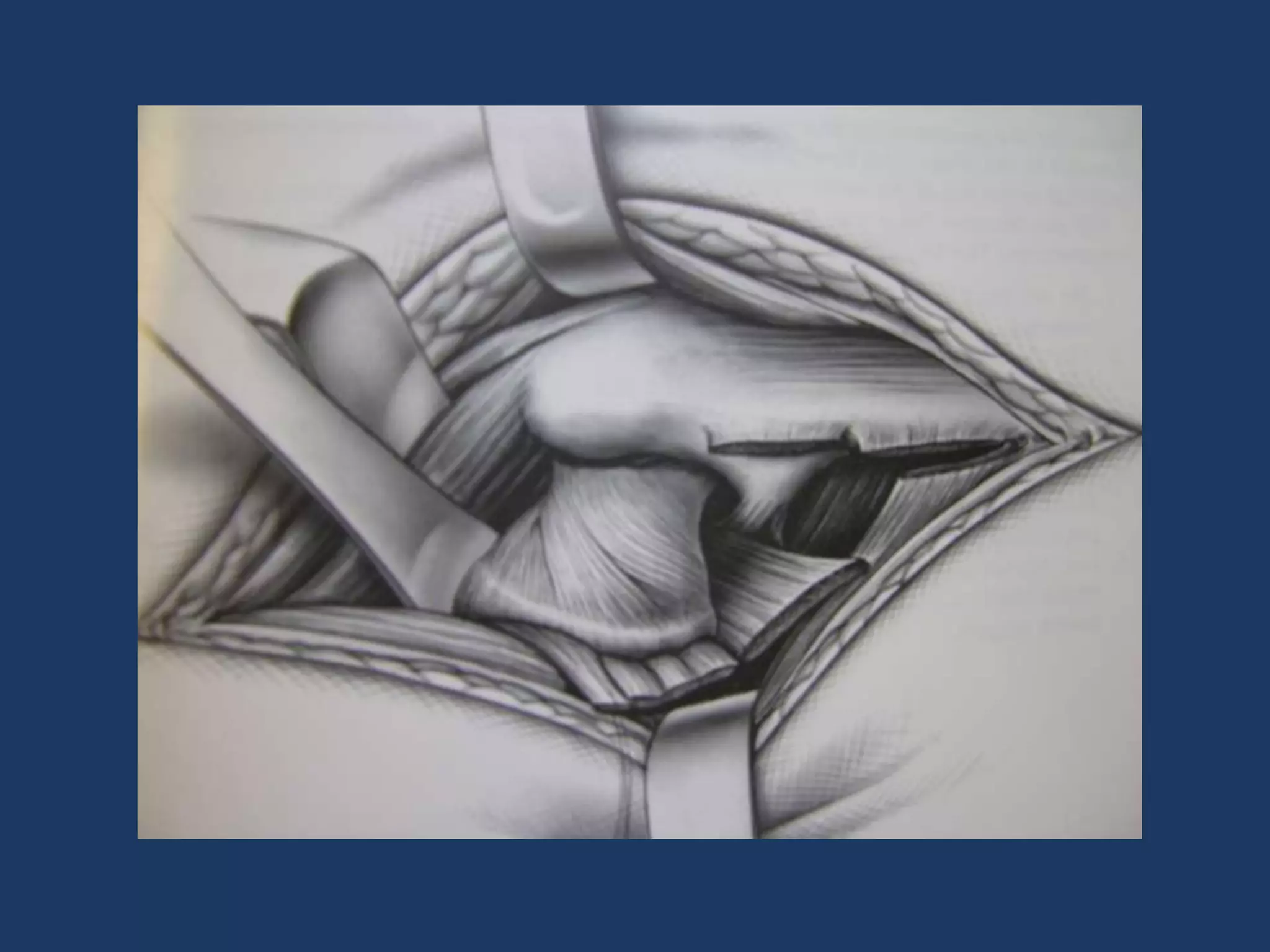
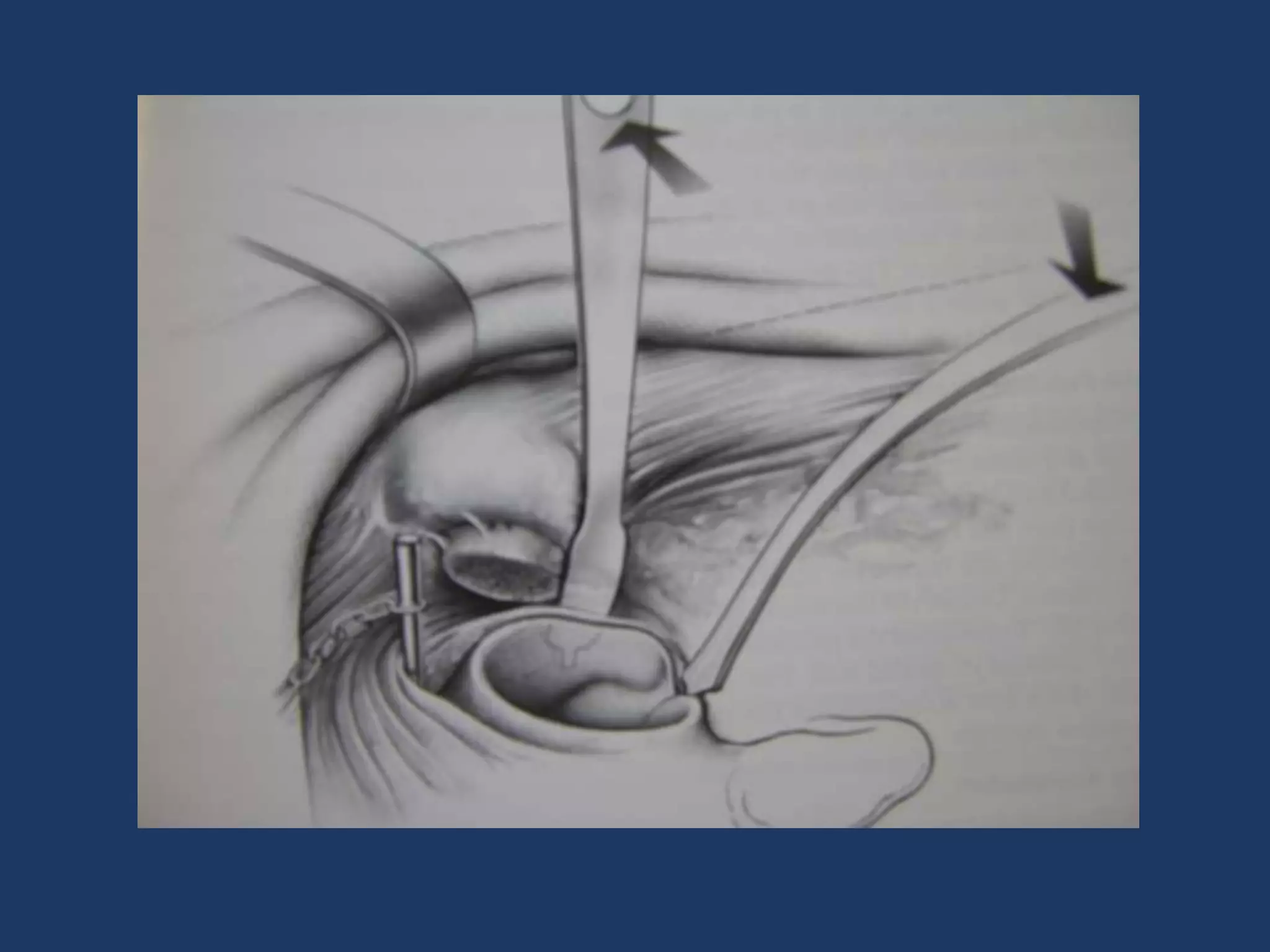
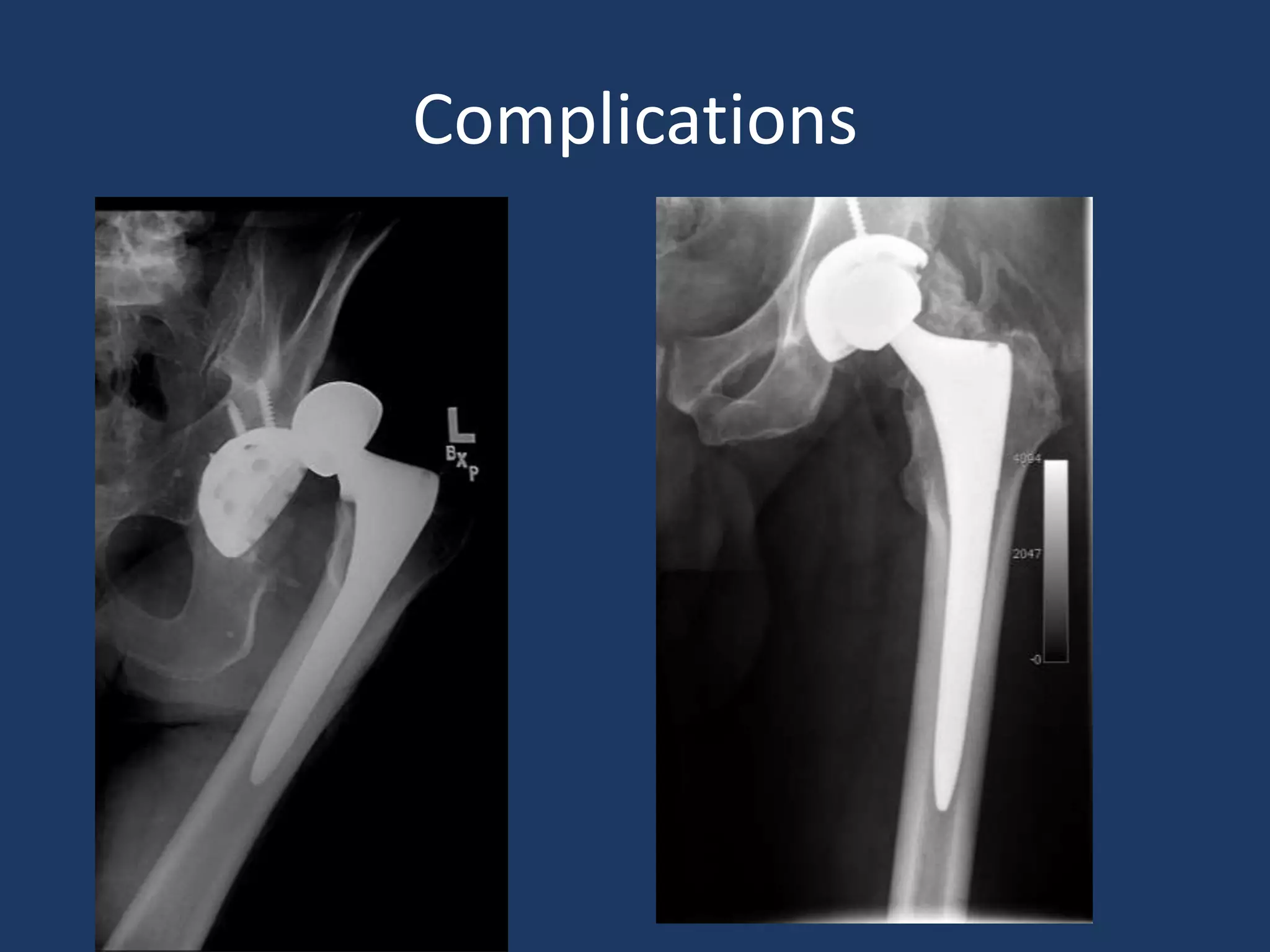
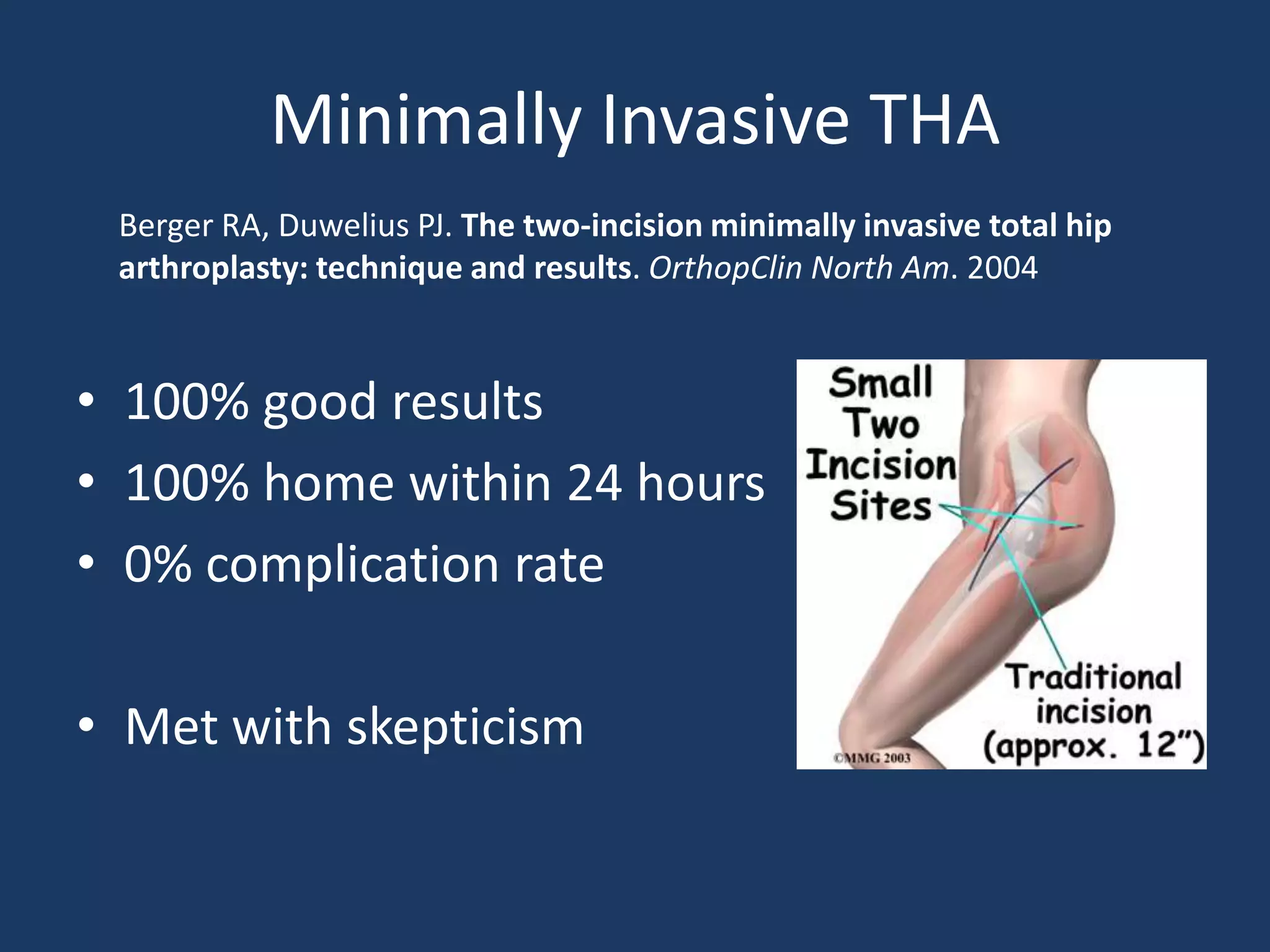
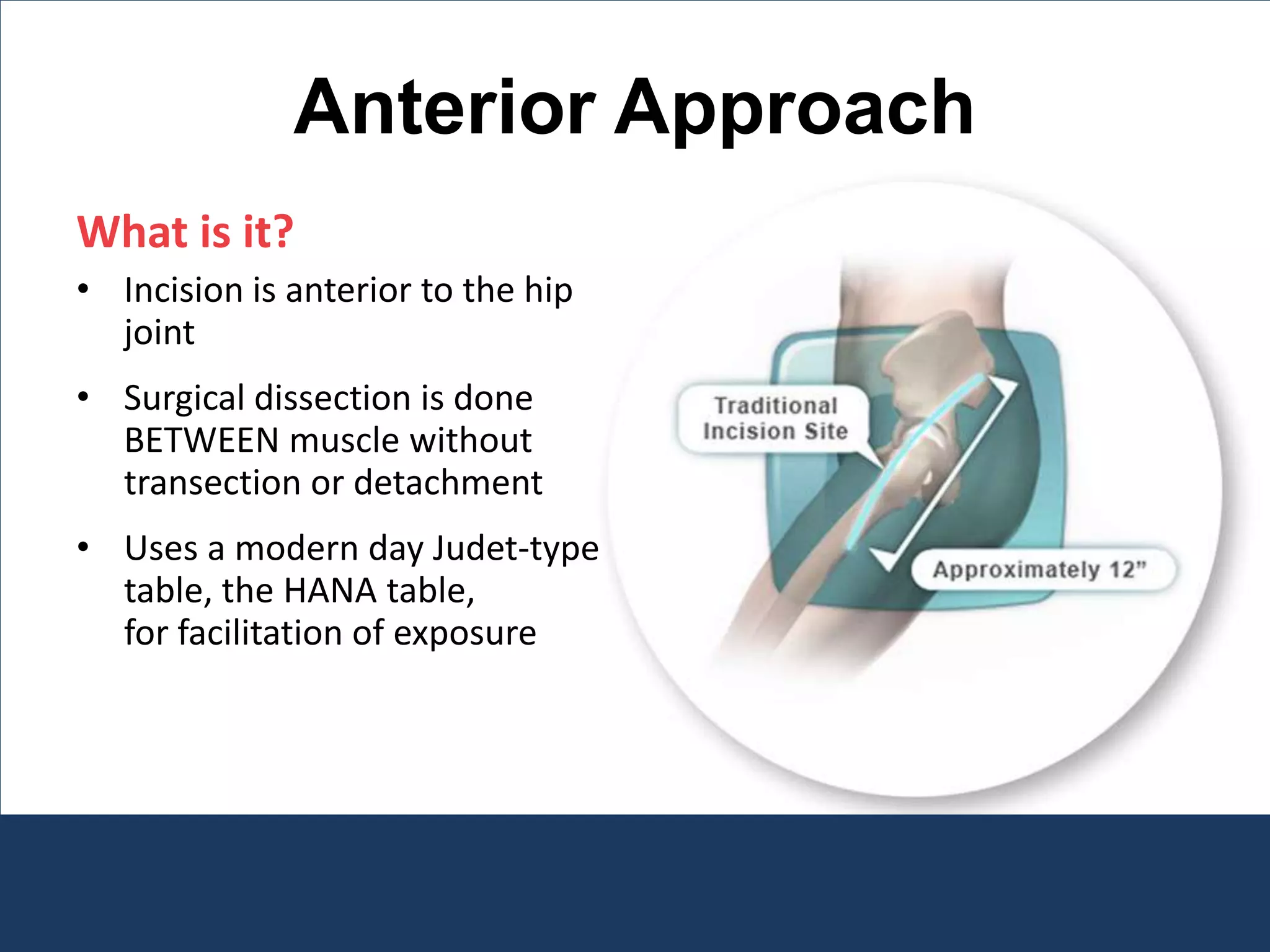
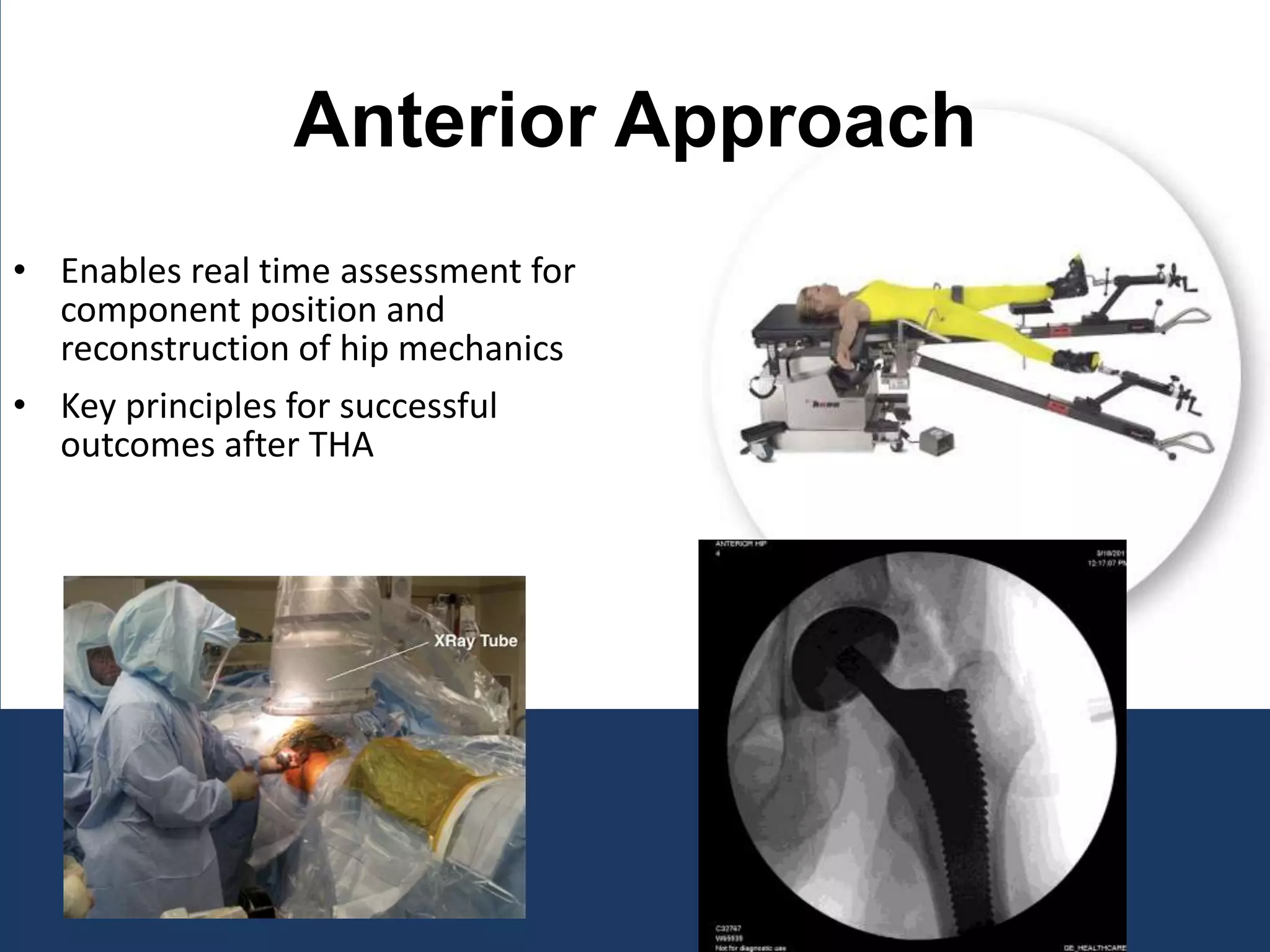
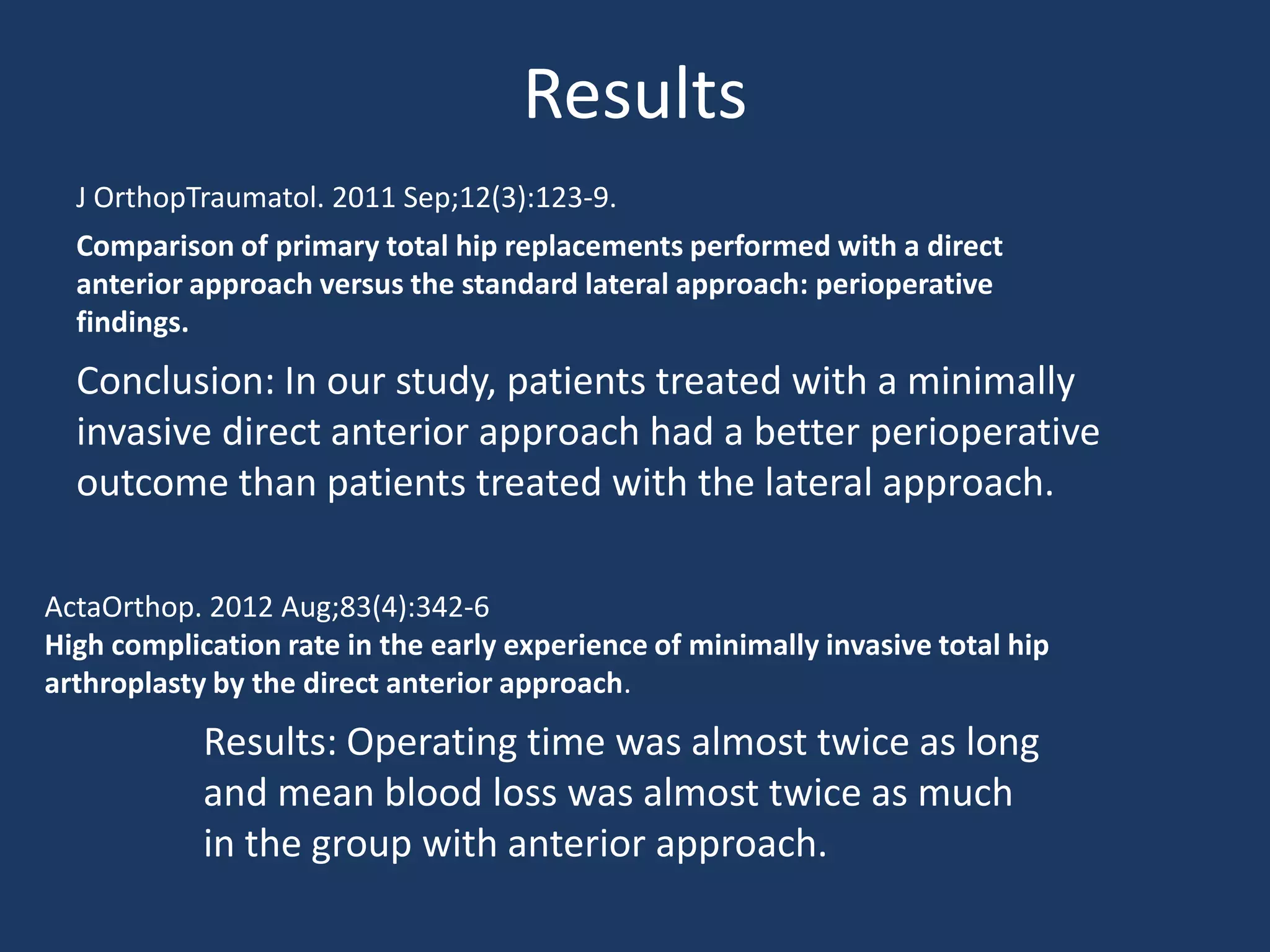
Minimally invasive total hip replacement aims to reduce recovery time. The direct anterior approach is promising but requires experience. It provides good exposure through a small incision without detaching muscles. Early results show less pain and faster recovery compared to traditional approaches, though blood loss and time were initially higher for surgeons adopting the technique. With a multidisciplinary team and careful patient selection, the direct anterior approach shows potential to improve outcomes for total hip replacement.