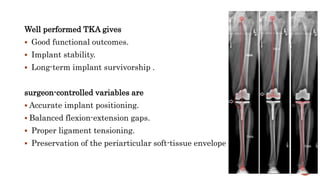
1. Robotic total knee arthroplasty (TKA) uses preoperative imaging and intraoperative robotics to improve the accuracy of implant positioning and soft tissue balancing compared to conventional jig-based TKA.
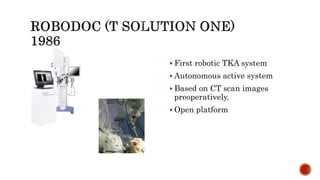
2. Earlier robotic systems were associated with technical complications in up to 30% of cases, but complication rates with newer systems, such as Mako and Navio, appear to be low.
3. Robotic TKA systems can be classified as passive, active, interactive, or teleoperated based on their level of autonomy and interaction with the surgeon. The most widely used interactive systems currently are Mako, Navio, Rosa, and Cori.













![The most well-known is the one proposed by Schneider and Troccaz in
2001.
It places robotic systems in four categories:
I] Passive
II] Active
III] Interactive
IV] Tele-operated](https://image.slidesharecdn.com/roboticsintkr-221120080128-ff7941b2/85/ROBOTICS-IN-TKR-pptx-17-320.jpg)