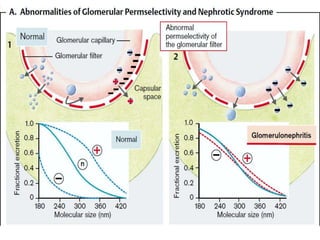
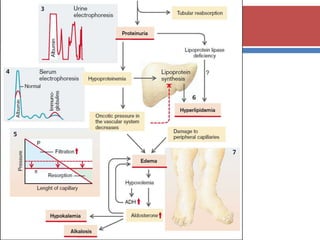
The document provides a comprehensive overview of glomerulonephritis (GN), detailing its structure, types, etiology, clinical features, diagnosis, and treatment options. GN is primarily an inflammatory condition affecting the glomeruli, leading to various symptoms such as hematuria, hypertension, and proteinuria. The text also discusses the complications and preventive measures associated with GN, emphasizing the importance of early diagnosis and appropriate treatment to prevent progression to chronic kidney disease.



































![ After 14-21 days of angina and other infections, young
people could have acute nephritic syndrome and
backache.
Important things:
o Never had renal disease
o Never had changes in the urinalysis
In urinalysis:
o Proteinuria 1-3 gr/l [in heavy case: 3-20gr/l]
o Detected erythrocytes, few leucocytes/lymphocytes/ and
cylinders
o Specific gravity is normal [during excess proteinuria SG ↑]](https://image.slidesharecdn.com/1-glomerulonephritis1-121210062940-phpapp01/85/Glomerulonephritis-HSUM-41-320.jpg)








![ Rapidly progressive glomerulonephritis (RPGN) is a
syndrome associated with severe glomerular injury and
does not denote a specific etiologic form of
glomerulonephritis. It is characterized clinically by rapid
and progressive loss of renal function associated with
severe oliguria and signs of nephritic syndrome; if
untreated, death from renal failure occurs within weeks
to months.[7]
The U.S – 7:1,000,000
The U.K – 2:100,000
Male : Female – 1:1
2-92 age](https://image.slidesharecdn.com/1-glomerulonephritis1-121210062940-phpapp01/85/Glomerulonephritis-HSUM-51-320.jpg)




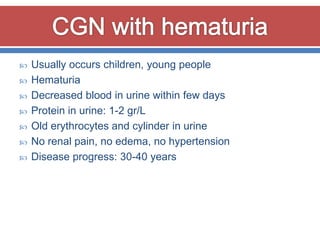
![ Nearly all forms of acute glomerulonephritis have a
tendency to progress to chronic glomerulonephritis. The
condition is characterized by irreversible and progressive
glomerular and tubulo-interstitial fibrosis, ultimately
leading to a reduction in the glomerular filtration rate
(GFR) and retention of uremic toxins. If disease
progression is not halted with therapy, the net results
are chronic kidney disease(CKD), end-stage renal
disease (ESRD), and cardiovascular disease.[10]](https://image.slidesharecdn.com/1-glomerulonephritis1-121210062940-phpapp01/85/Glomerulonephritis-HSUM-56-320.jpg)