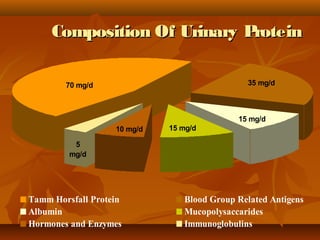
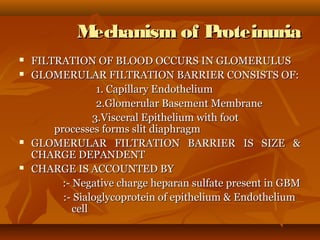
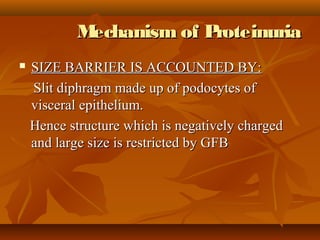
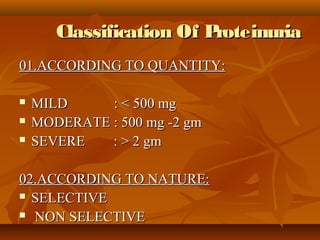
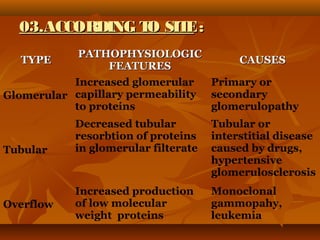
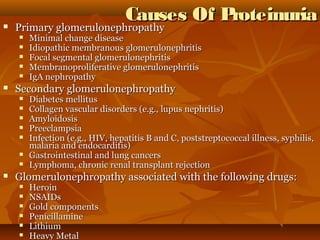
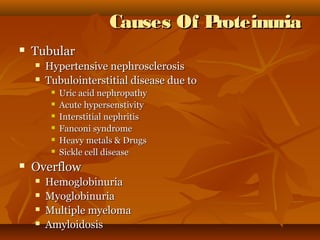
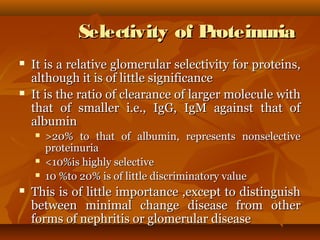
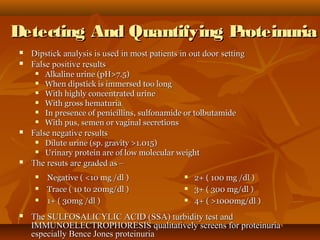
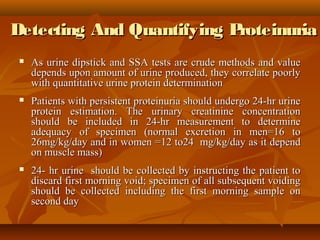
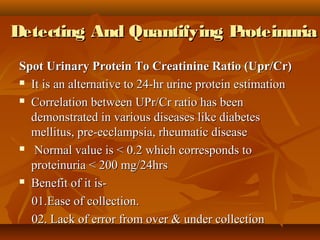
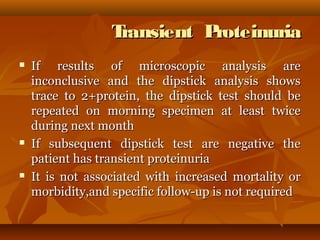
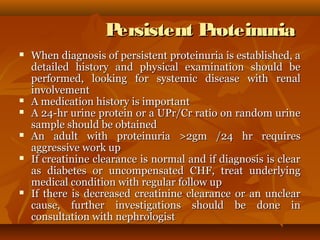
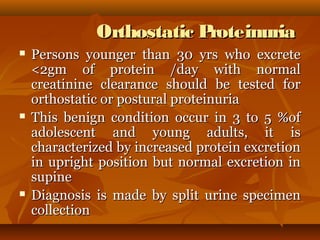
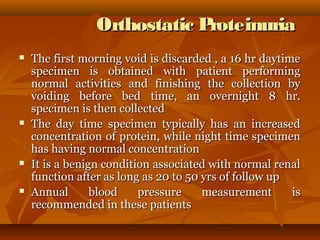
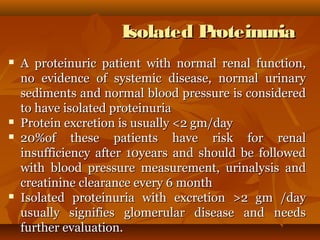
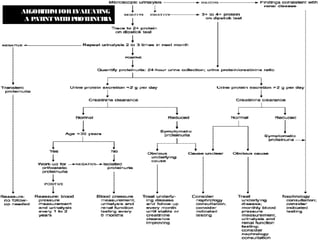
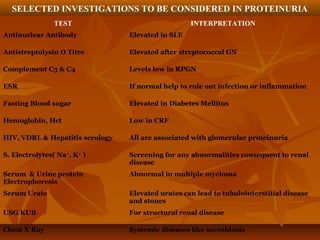
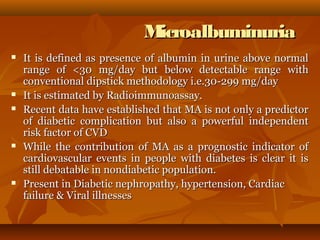
This document discusses proteinuria, its definitions, causes, classification, and diagnostic evaluation in medical practice, emphasizing its prevalence and benign nature in many cases. It outlines mechanisms leading to proteinuria and the importance of differentiating between transient and persistent proteinuria through various tests and patient evaluations. The text also highlights specific conditions linked to proteinuria and the clinical significance of microalbuminuria as a cardiovascular risk indicator.