The document discusses several concepts related to nursing ethics including:
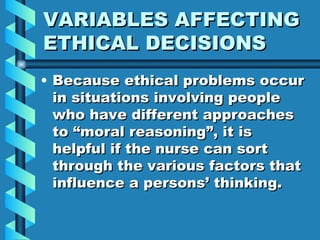
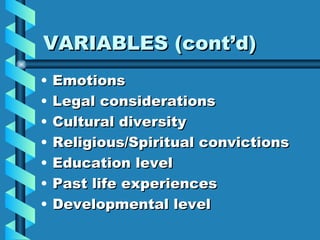
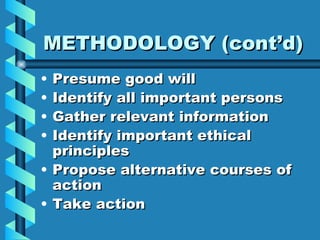
1) Ethics is concerned with determining norms and standards to establish good conduct beyond personal preferences. Within nursing, specific ethical values and requirements are necessary to maintain integrity.
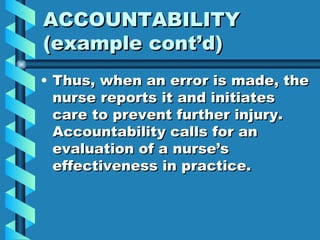
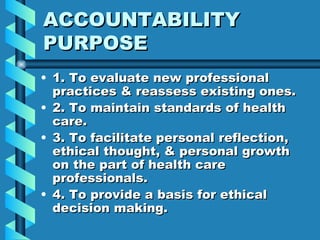
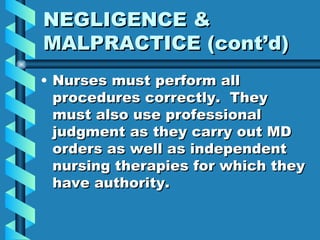
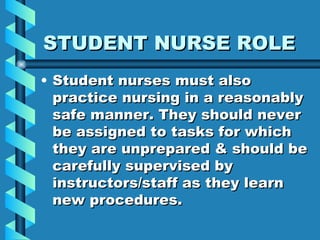
2) Nurses must continue developing their moral identity and knowledge of ethics to participate effectively in the ethical dimensions of their practice. They are responsible and accountable for the nursing care provided.
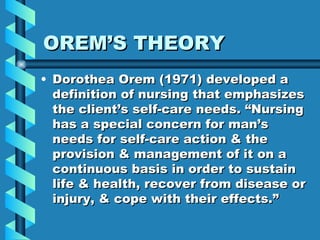
3) Orem's theory of nursing focuses on helping clients meet self-care requisites and regain independence when unable to due to illness or injury. The goal is to increase client's ability to independently meet biological, psychological and social needs.