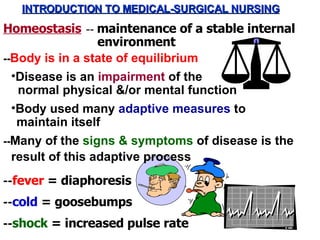
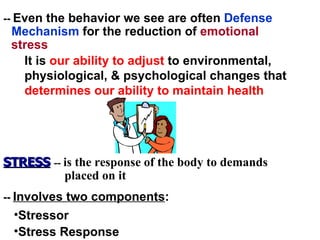
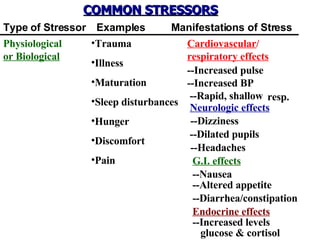
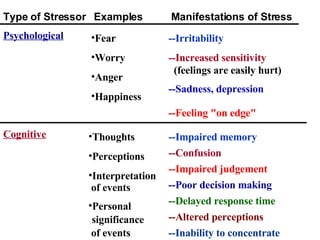
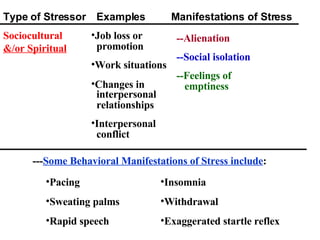
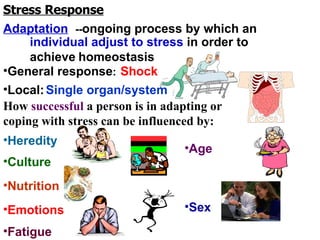
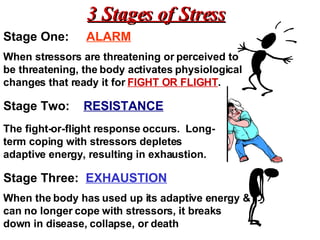
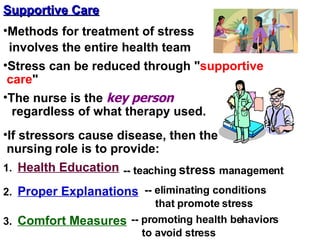
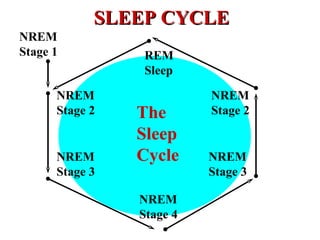
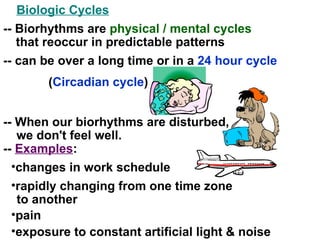
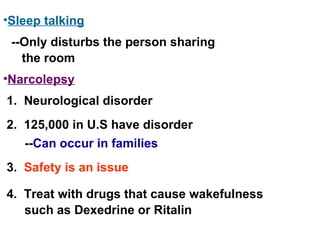
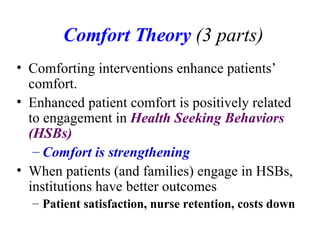
This document provides an introduction to medical-surgical nursing concepts. It discusses homeostasis and how the body maintains equilibrium during disease or stress. Stress is defined as having a stressor and a stress response from the body. Common stressors can be physiological, psychological, sociocultural, or environmental in nature. The body's stress response occurs in three stages: alarm, resistance, and exhaustion. Nurses aim to support patients' normal adaptive processes through supportive care methods like health education, explanations, and comfort measures. Rest, sleep, and biological cycles are also discussed in relation to stress and homeostasis.