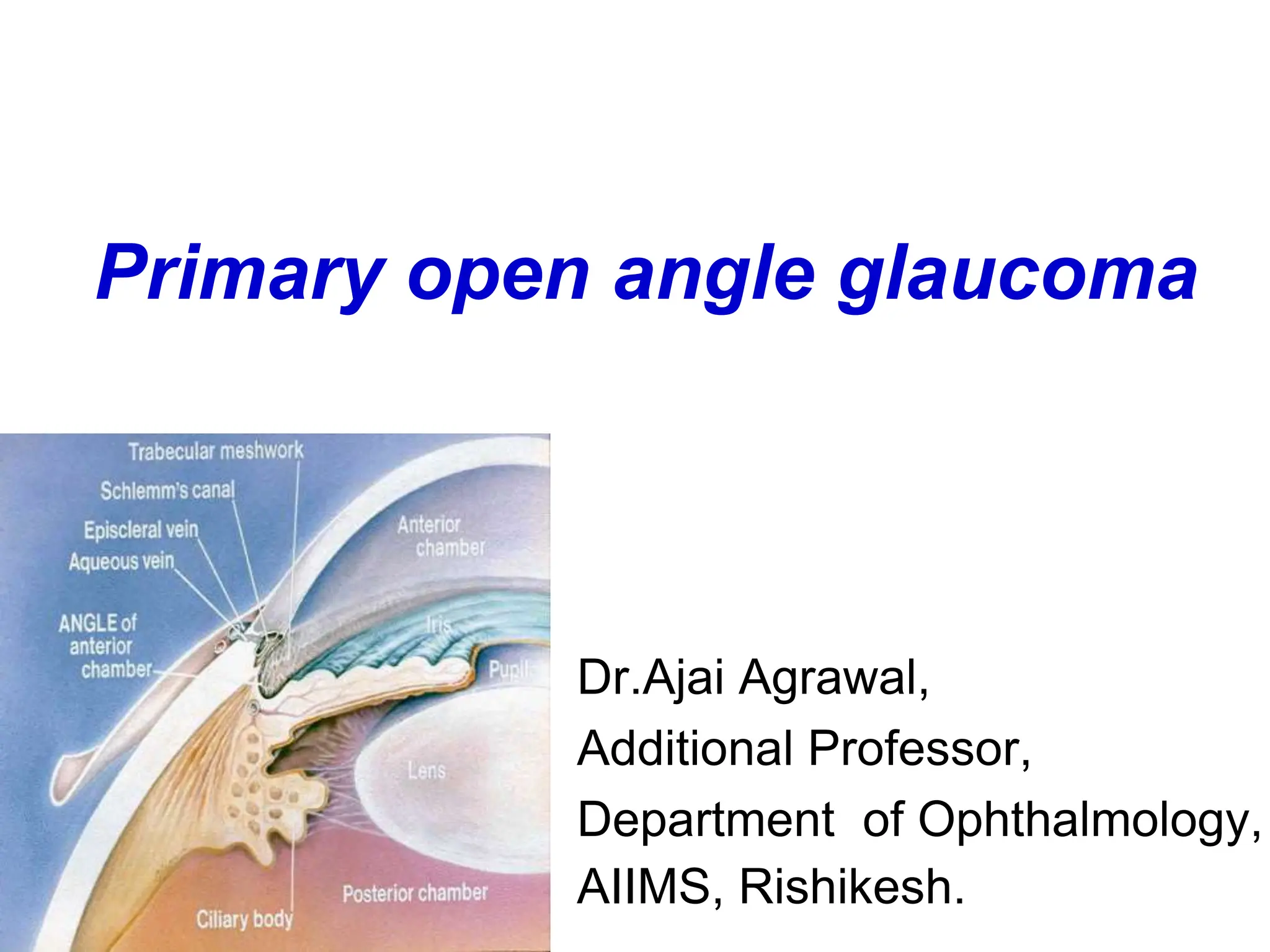
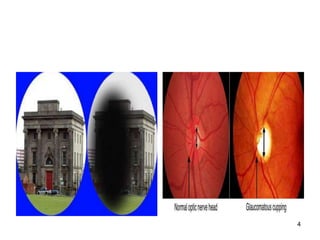
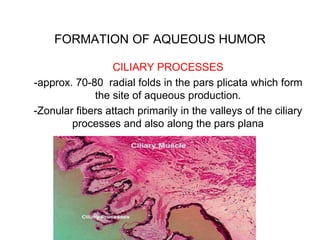
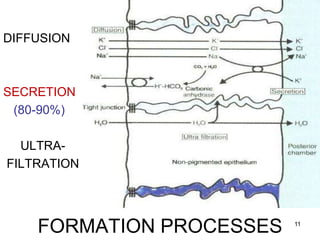
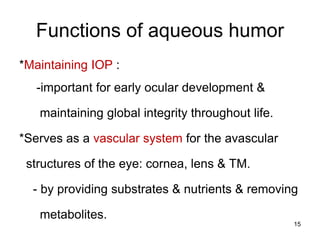
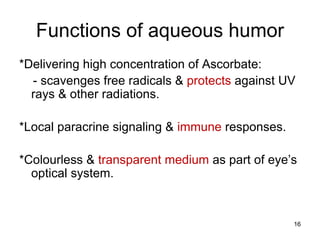
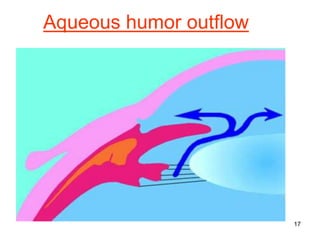
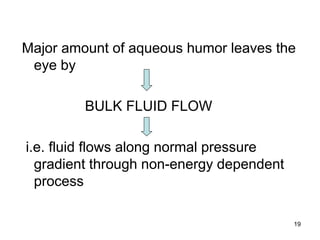
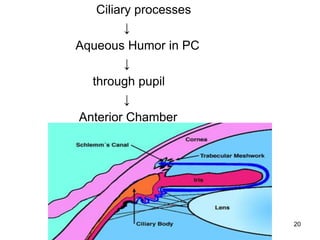
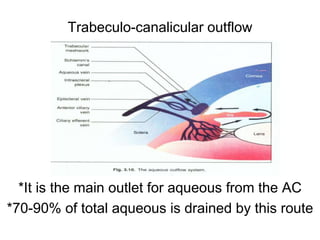
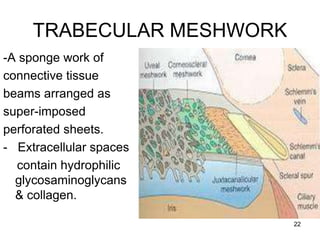
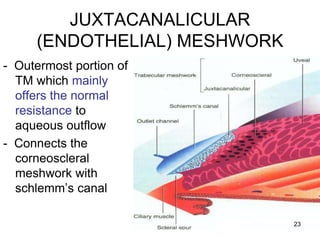
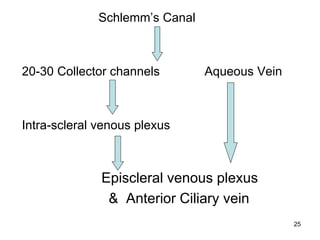
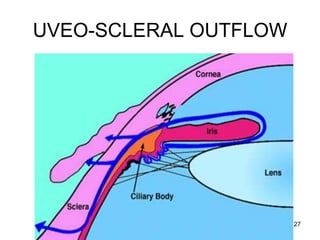
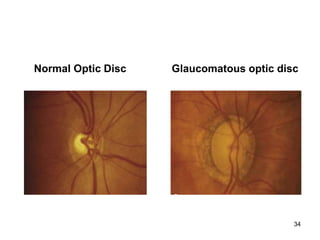
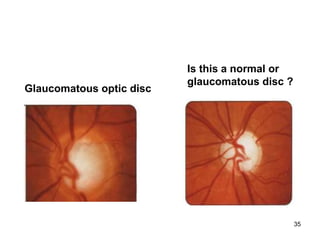
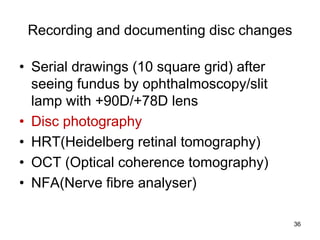
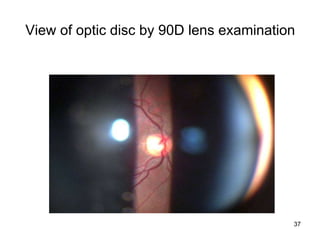
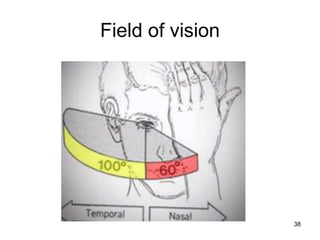
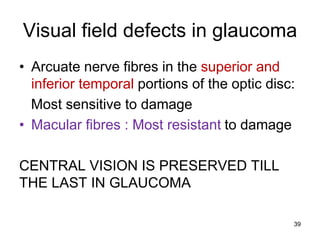
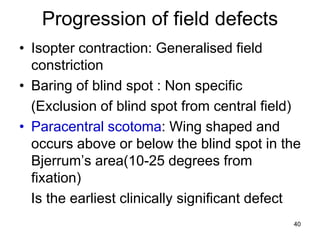
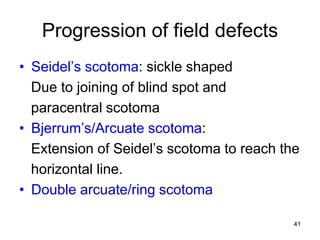
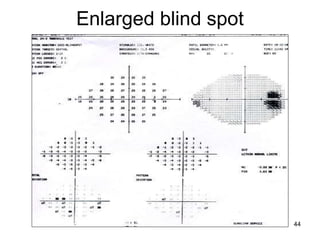
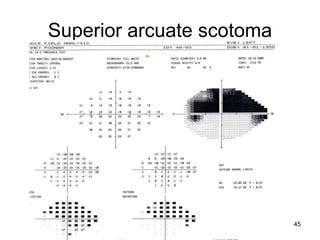
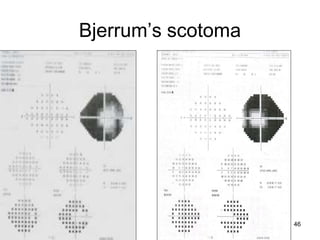
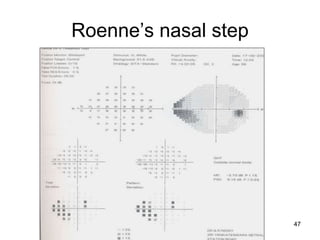
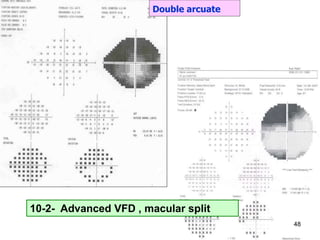
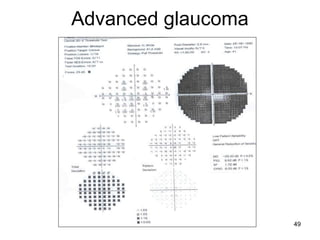
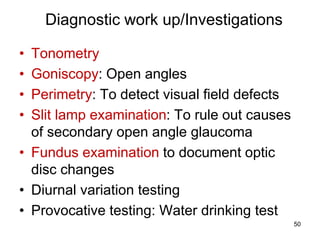
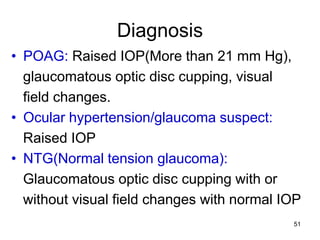
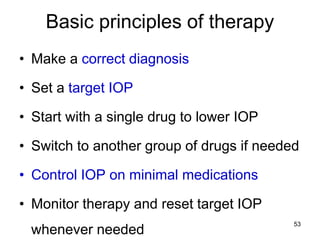
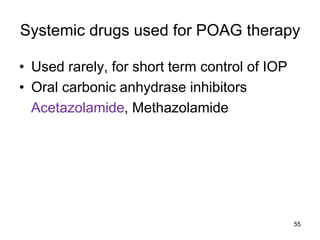
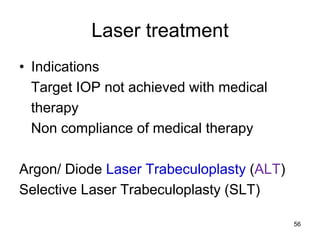
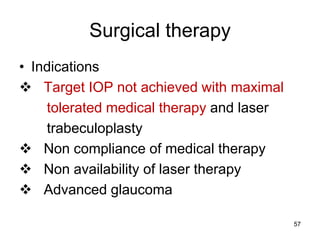
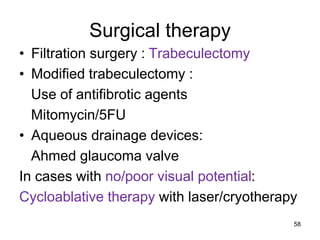
This document provides information on primary open angle glaucoma (POAG). It defines POAG as a chronic, progressive optic neuropathy characterized by morphological changes in the optic disc and retinal nerve fiber layer leading to visual field changes in the absence of other ocular diseases. Risk factors for POAG include elevated intraocular pressure, increasing age, family history, diabetes, and thin central corneas. The pathophysiology involves decreased aqueous outflow leading to increased resistance and intraocular pressure, causing distortion and ischemia of the optic nerve. Signs include elevated intraocular pressure, optic disc cupping, and visual field defects. Treatment aims to lower intraocular pressure through medications, laser trabeculoplasty, or filtration surgery to minimize