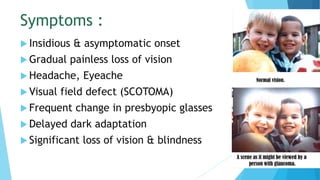
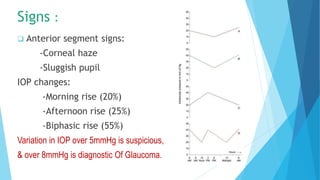
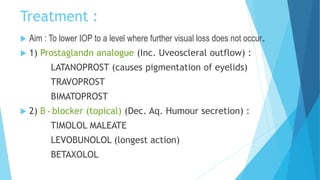
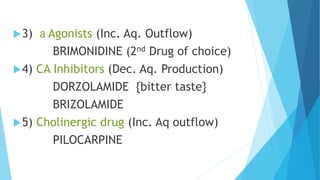
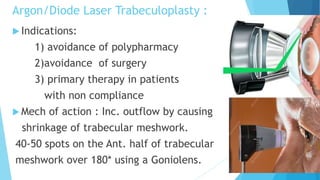
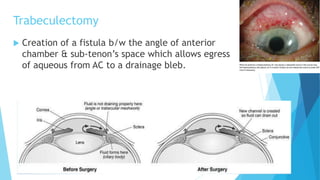
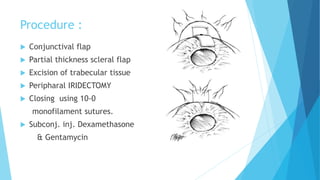
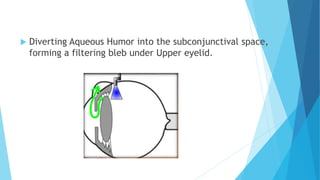
This document provides information on primary open angle glaucoma (POAG), the most common type of glaucoma. It defines POAG as a chronic, progressive optic neuropathy caused by conditions that lead to optic nerve damage and vision loss, with the main risk factor being elevated intraocular pressure (IOP). The document discusses the epidemiology of POAG, symptoms, signs, diagnostic tests, treatment options including medications and surgeries like trabeculectomy, and provides details on mechanisms and risk factors of the disease.