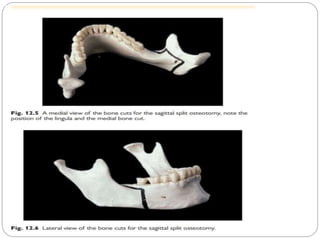
Orthognathic surgery is used to correct skeletal discrepancies of the jaw bones that cannot be addressed by orthodontics alone. It involves both pre-surgical orthodontics to position the teeth and surgical procedures on the mandible and/or maxilla. Common mandibular procedures include sagittal split osteotomy to move the mandible forwards or backwards and vertical subsigmoid osteotomy to push the mandible back. The main maxillary procedure is a Le Fort I osteotomy where the maxilla is freed and can be repositioned using a buccal incision approach. Both procedures aim to correct functional and aesthetic issues of the jaws and require postoperative orthodontics for detailed occlusion.