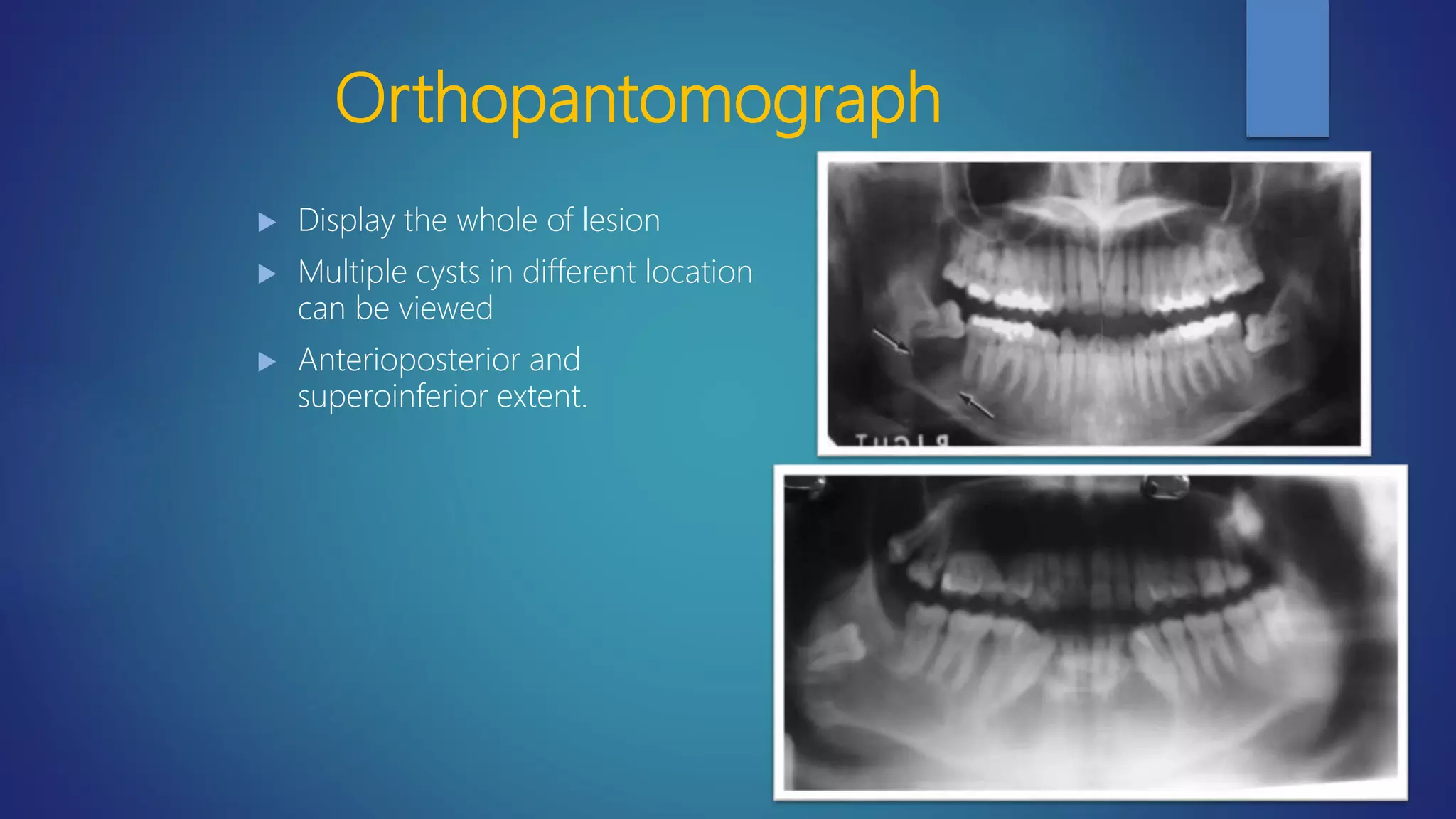
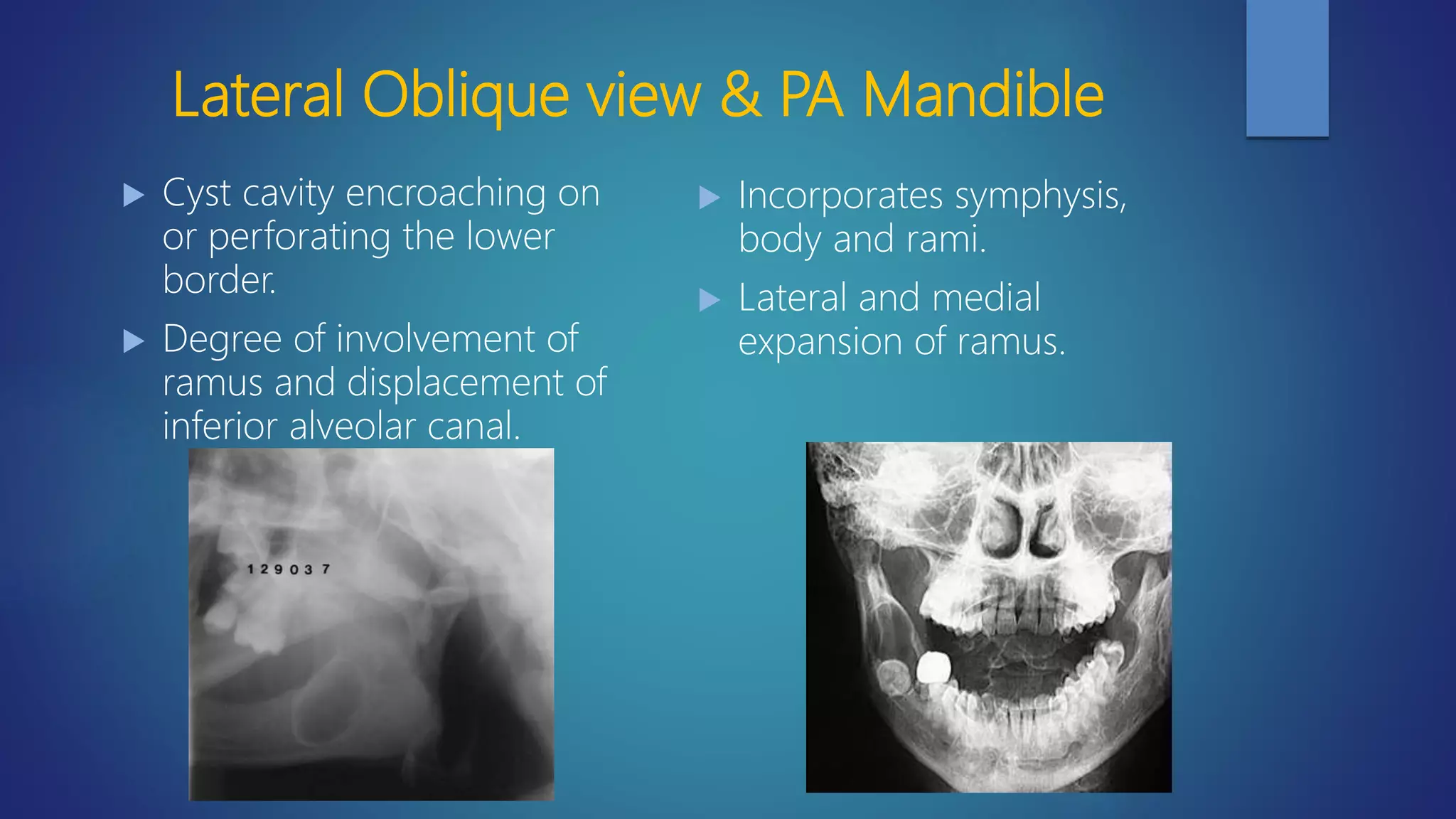
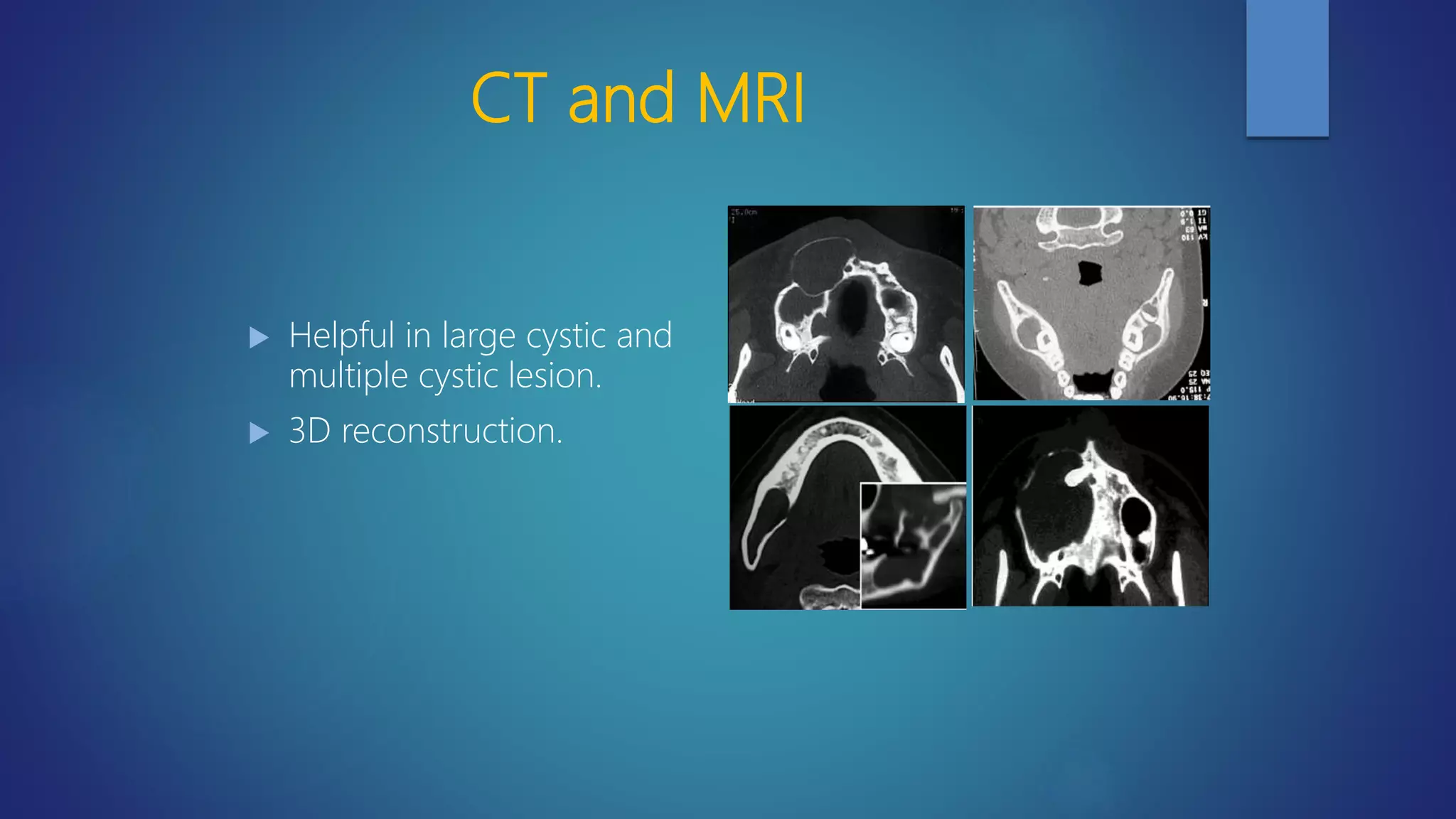
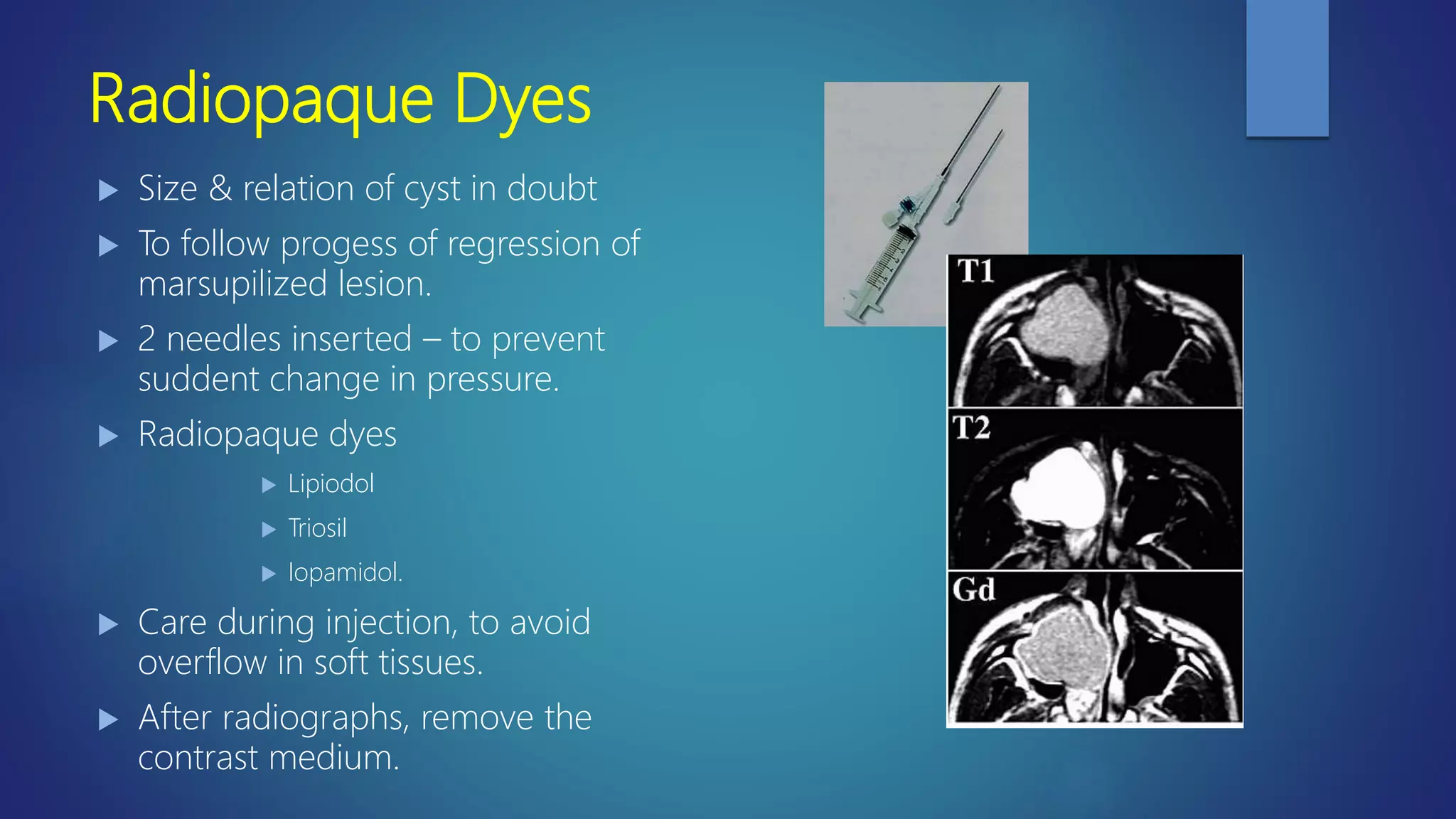
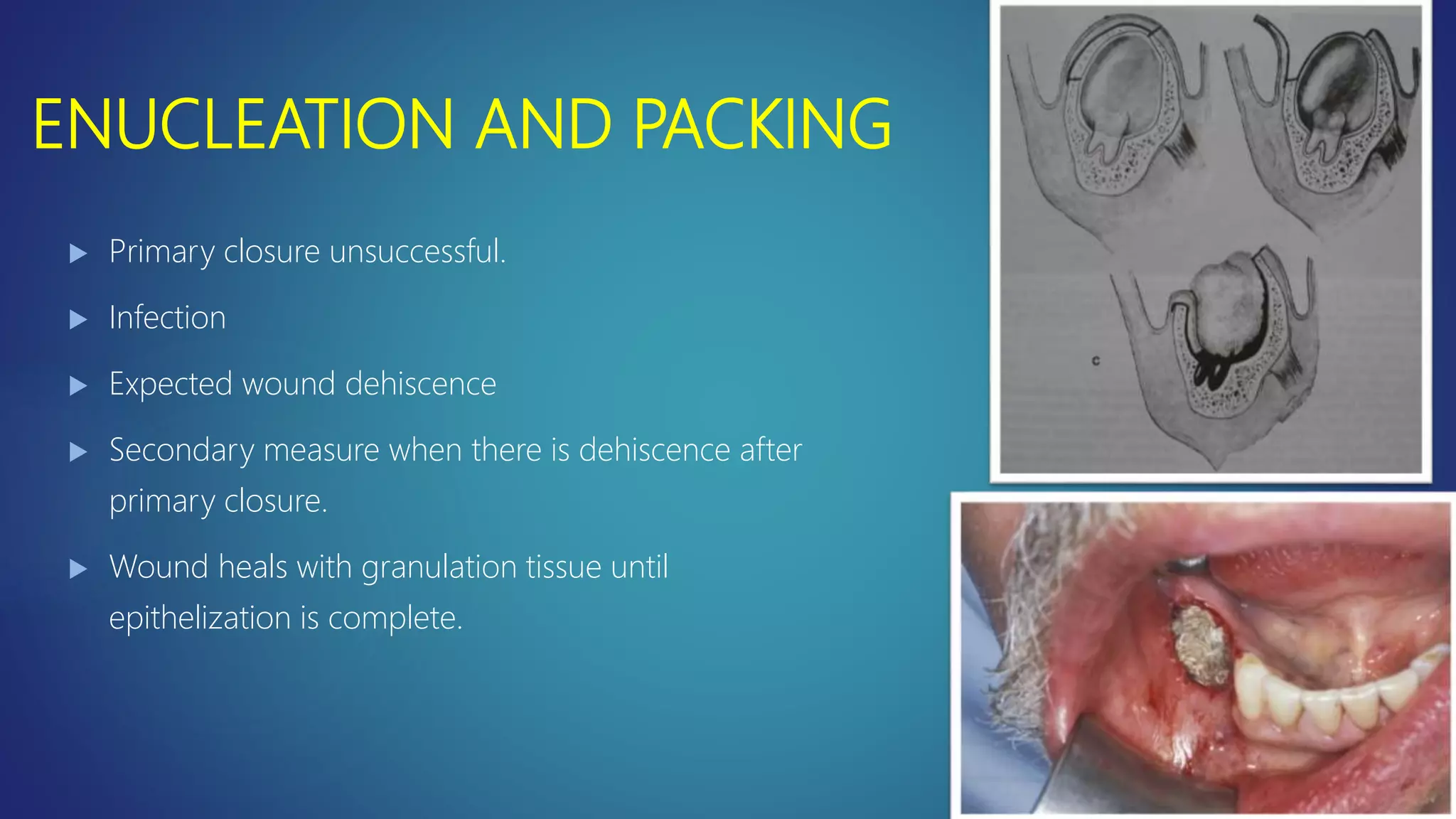
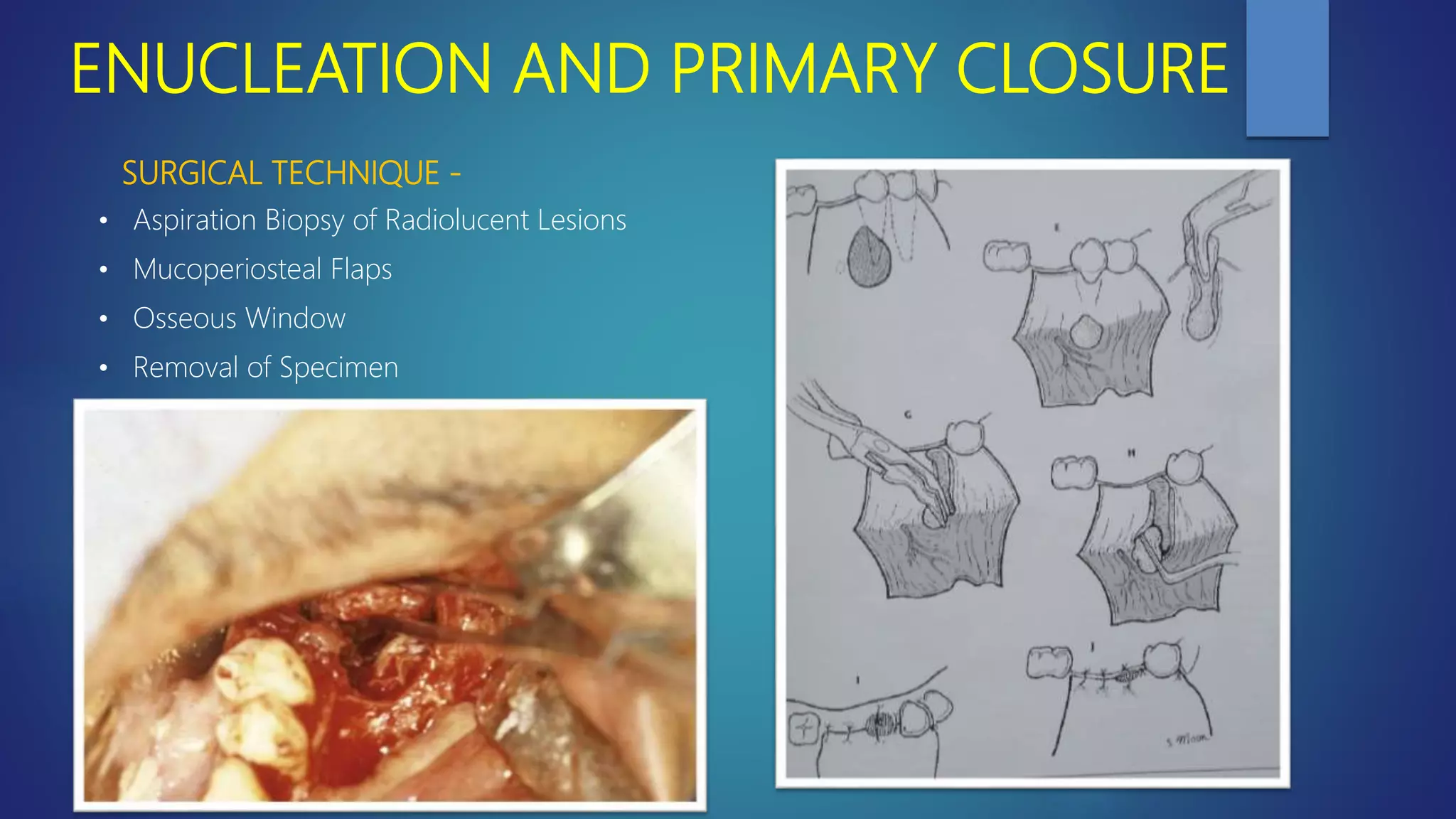
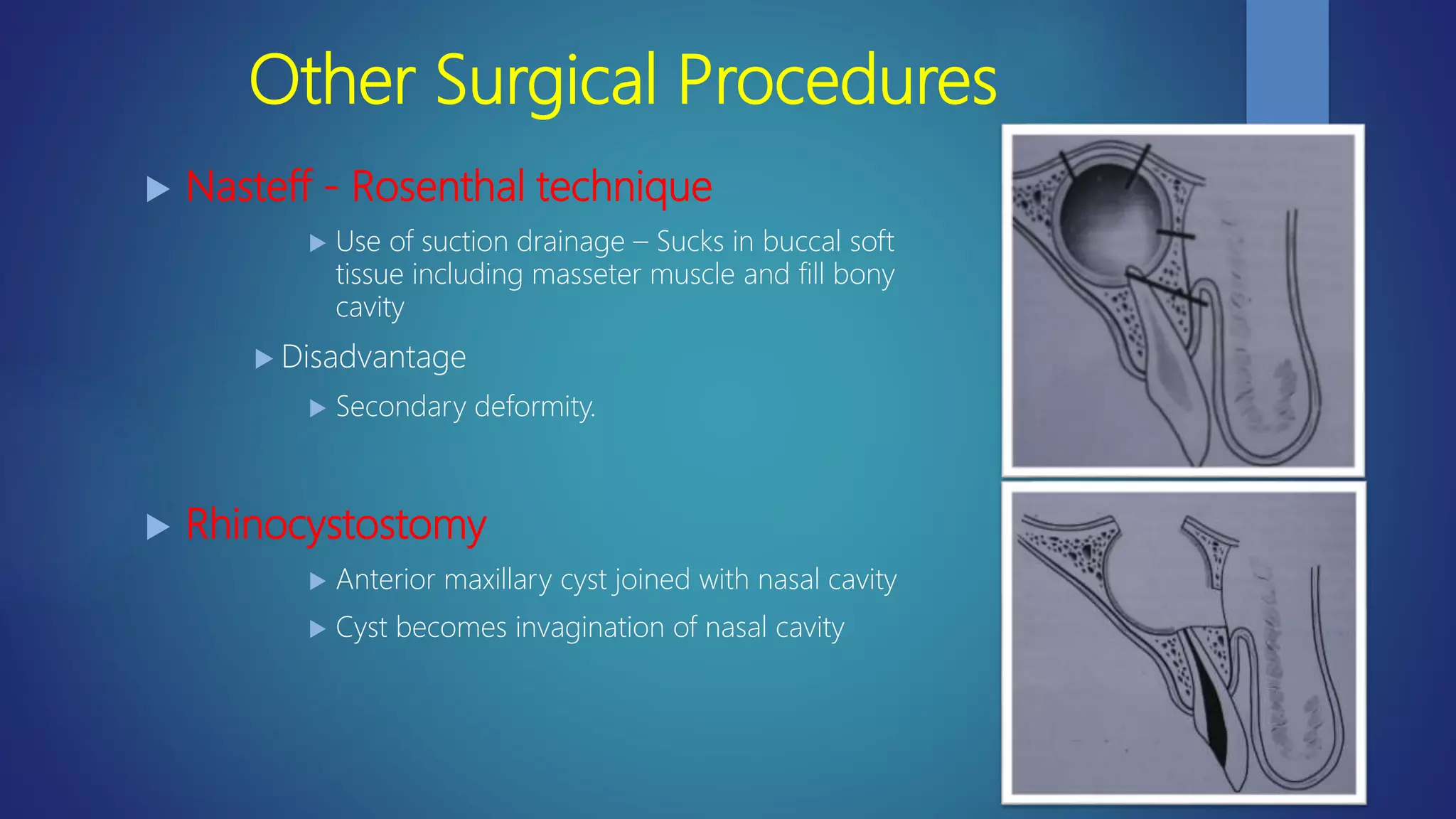
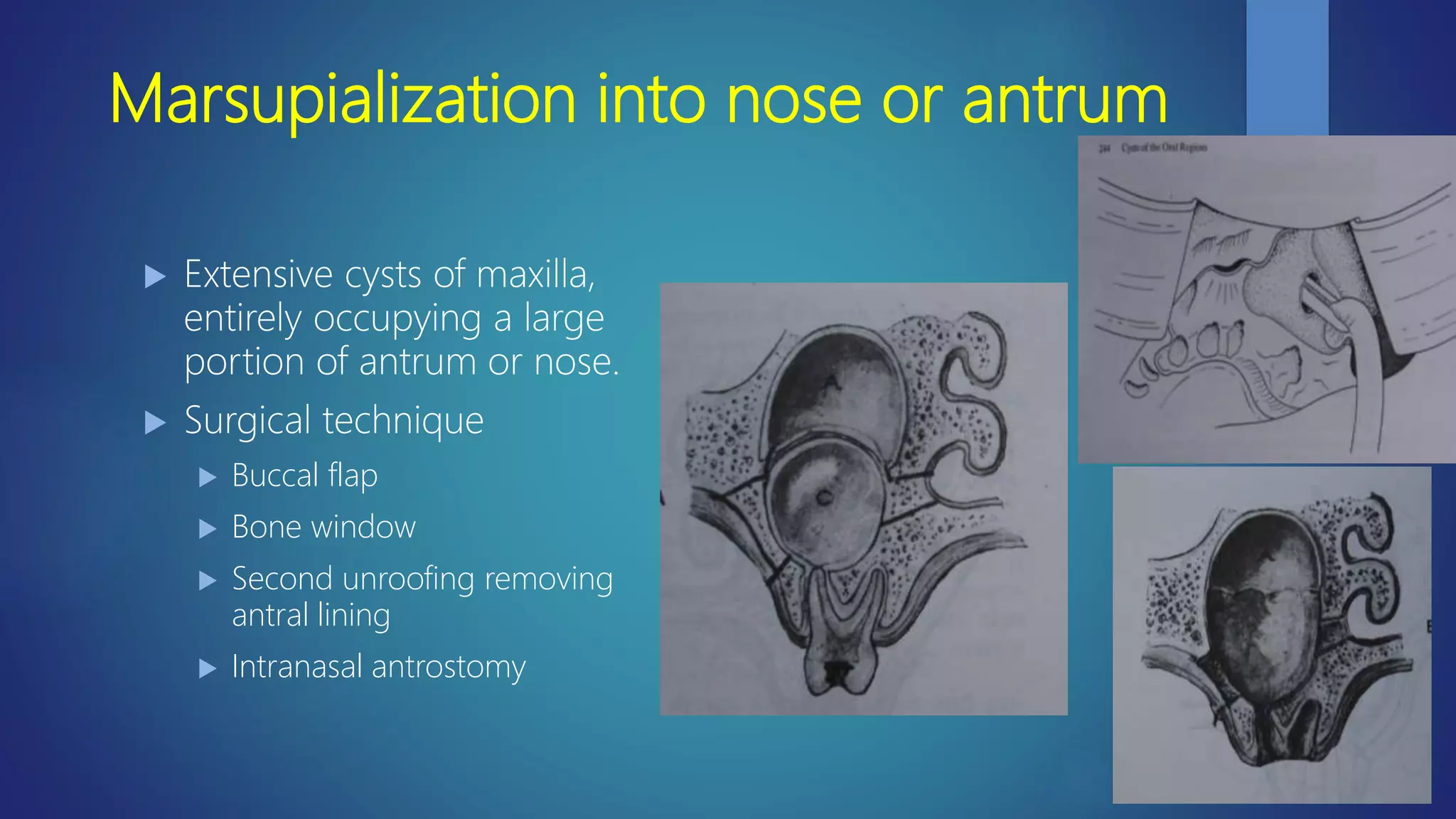
This document discusses the principles of managing odontogenic cysts. It provides an overview of investigations like physical examination, radiographic examination, aspiration and biopsy that are used to diagnose cysts. It then discusses various treatment options like decompression, enucleation, and marsupialization. Enucleation involves completely removing the cyst lining in one piece while marsupialization removes the entire cyst roof to create a window for drainage.