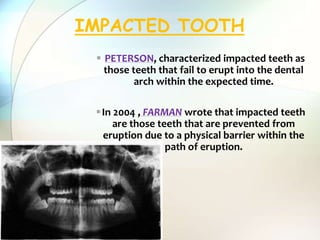
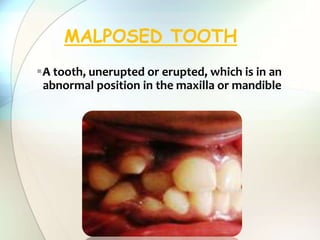
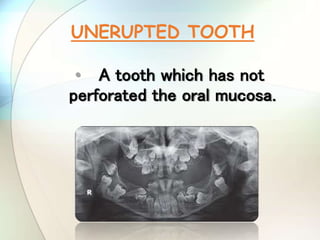
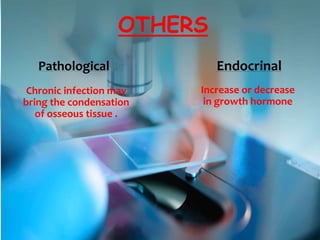
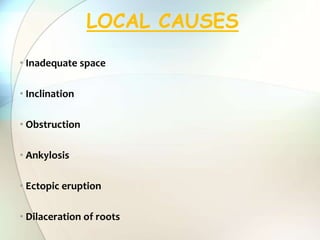
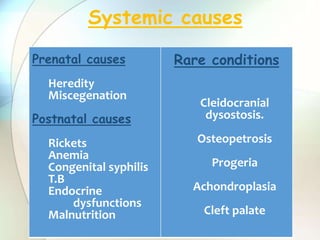
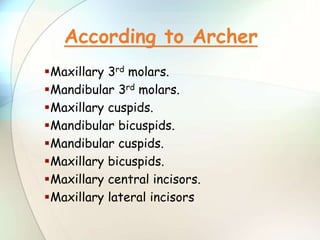
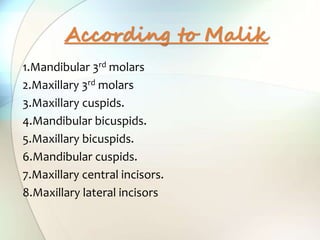
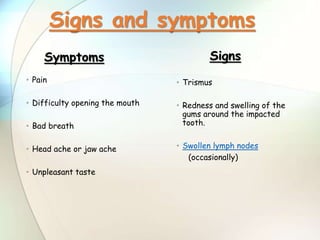
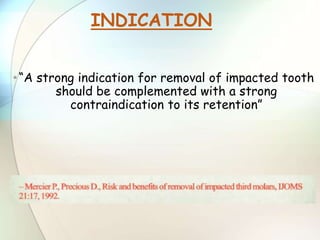
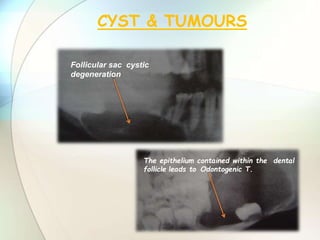
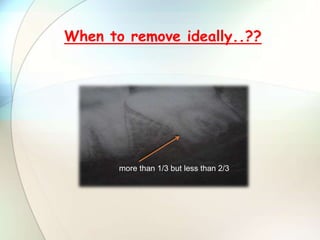
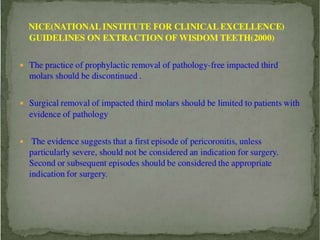
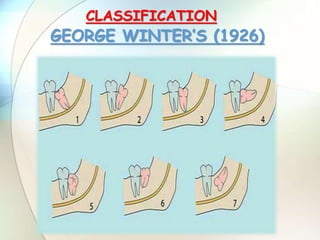
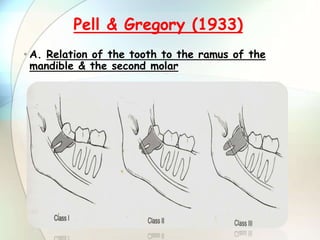
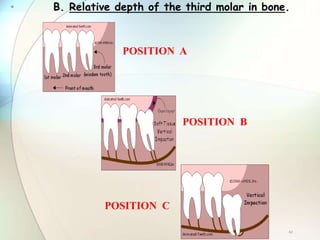
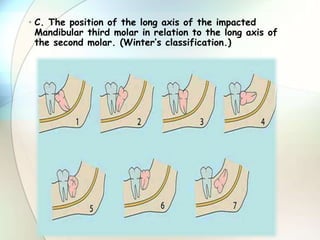
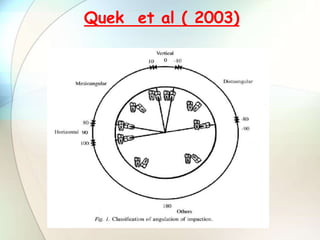
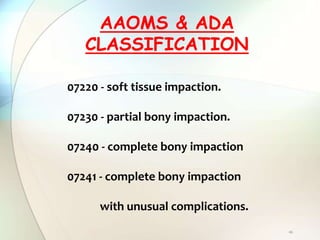
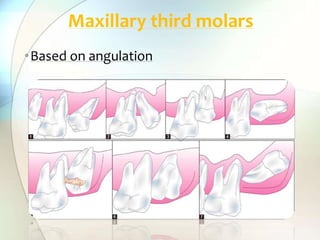
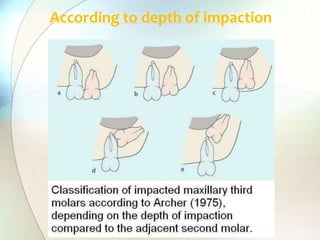
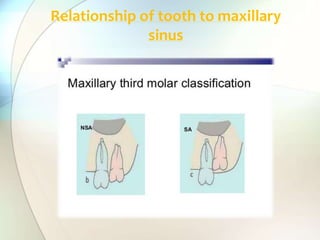
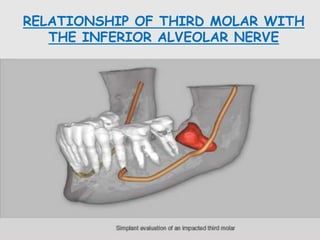
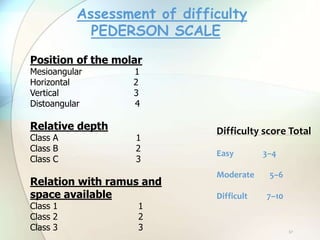
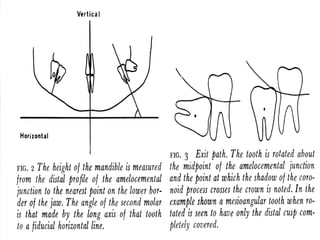
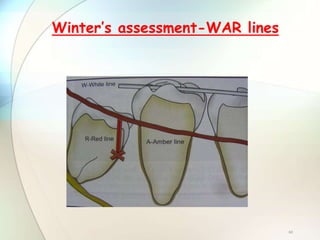
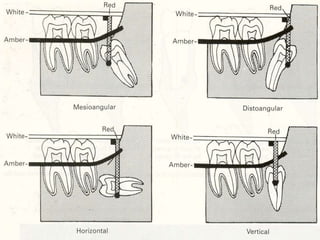
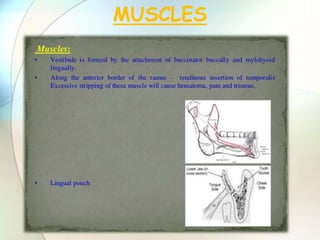
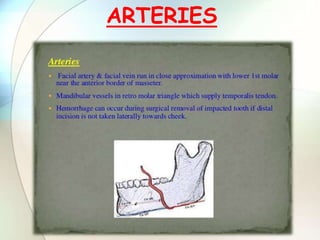
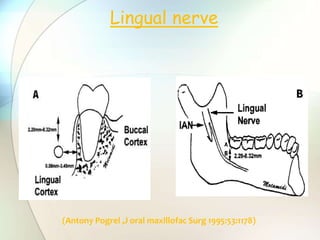
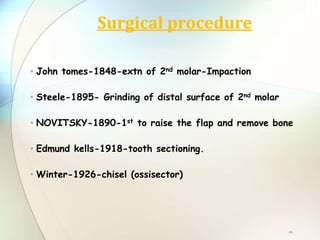
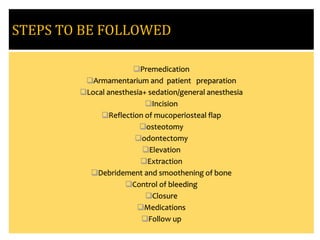
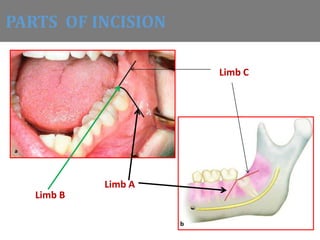
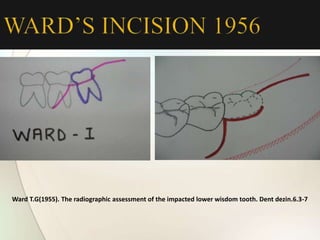
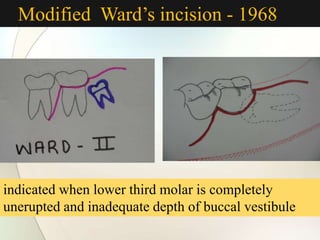
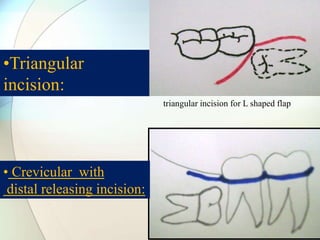
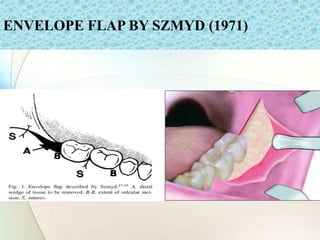
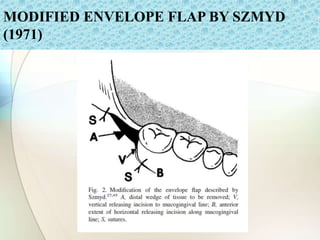
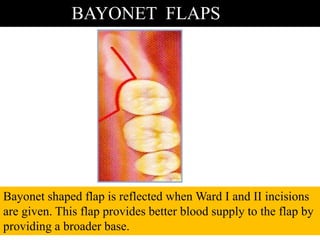
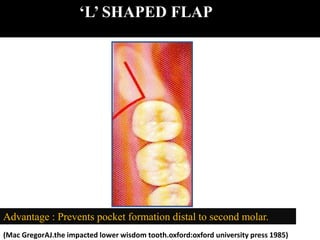
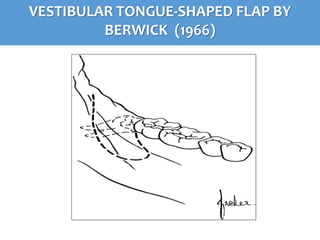
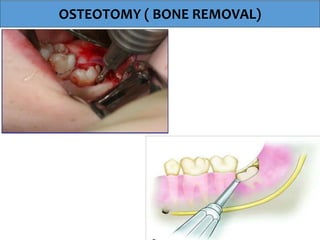
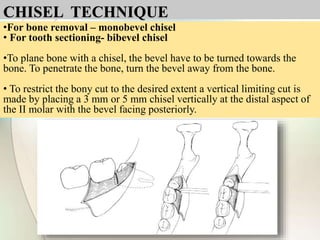
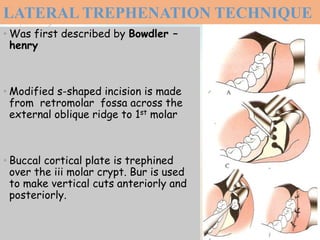
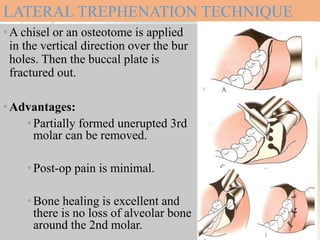
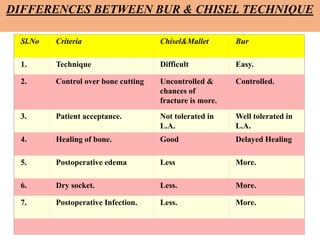
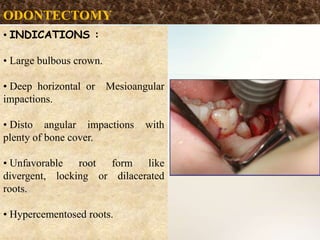
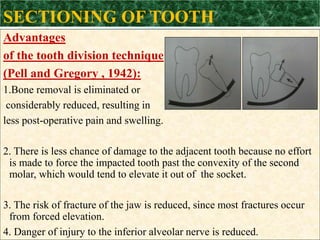
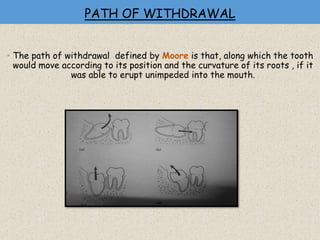
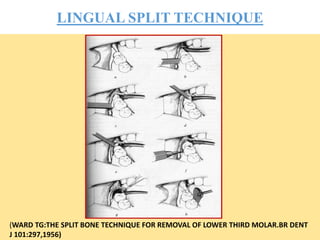
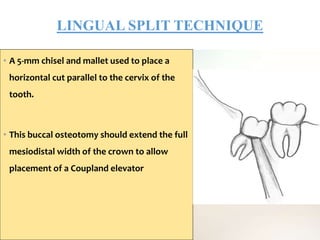
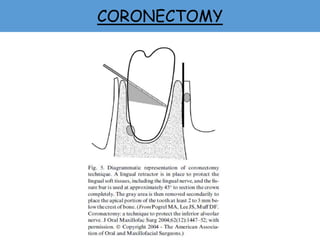
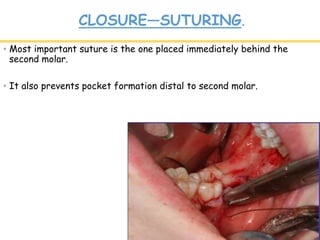
This document provides information about impaction of teeth. It begins with definitions of terms like impacted tooth and discusses various theories of impaction such as orthodontic theory and phylogenic theory. It then covers the causes, order of frequency, and complications of impacted teeth. The document outlines indications and contraindications for removal of impacted teeth and classifications of impaction. Surgical procedures for removal are also summarized, including incisions, osteotomy techniques, tooth sectioning, and closure methods.