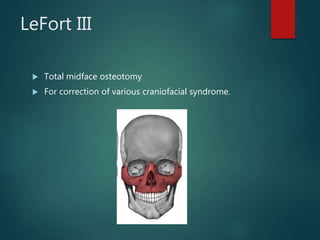
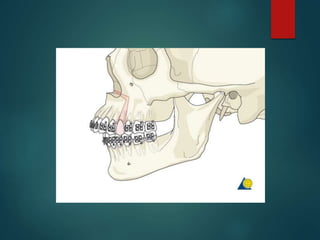
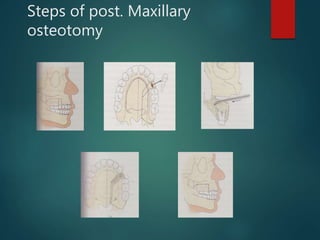
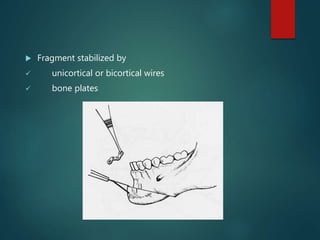
This document provides an overview of major surgical procedures, including orthognathic surgeries. It defines orthognathic surgery as combining orthodontics and oral surgery to correct dentofacial deformities. The key steps are described as diagnosis, presurgical orthodontics, surgical treatment planning, mock surgery, the surgery and stabilization, and postsurgical orthodontics. Various surgical methods are outlined for maxillary osteotomies including LeFort I, II, and III, and for mandibular procedures including sagittal split osteotomy and genioplasty. Distraction osteogenesis is also summarized as a technique for gradual bone expansion.