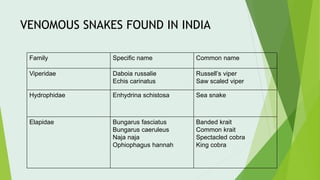
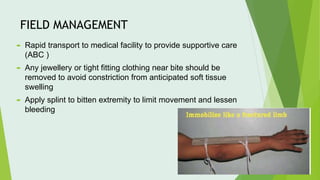
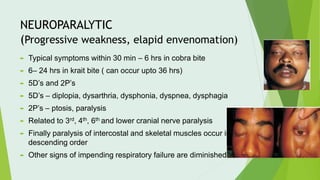
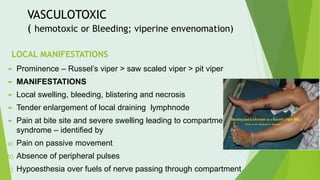
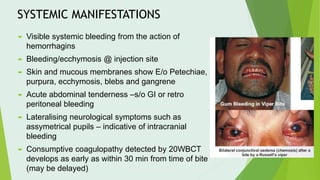
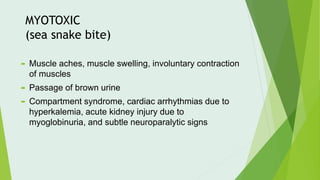
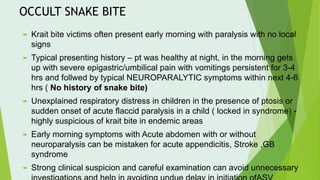
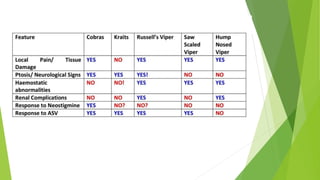
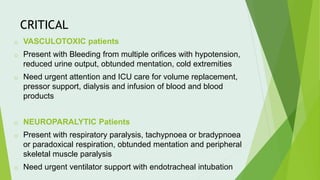
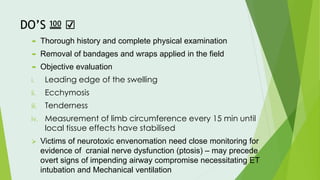
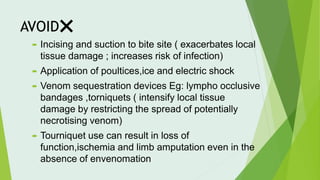
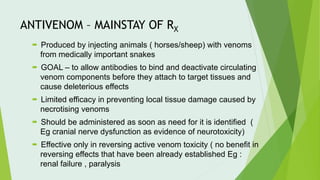
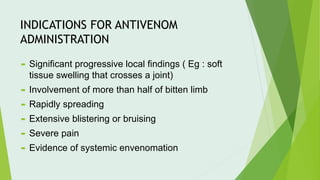
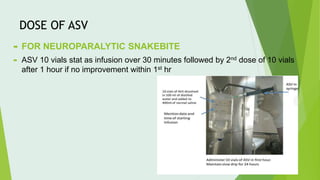
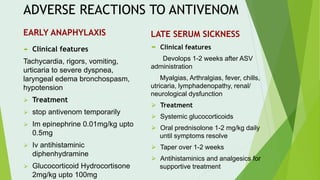
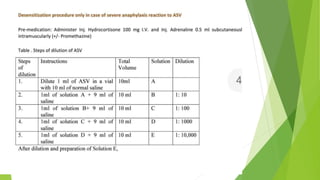
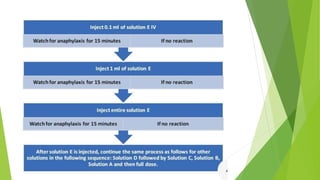
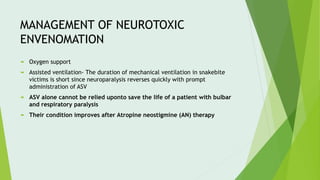
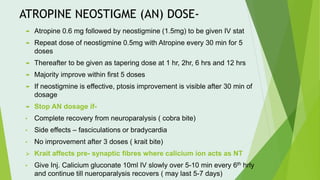
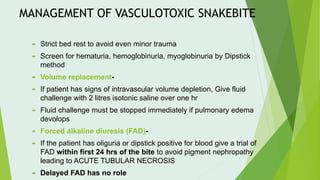
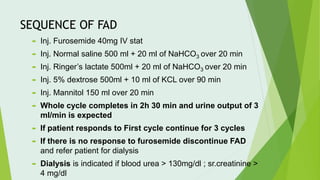
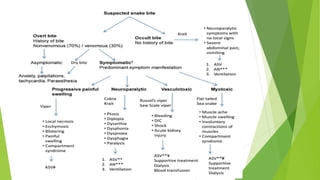
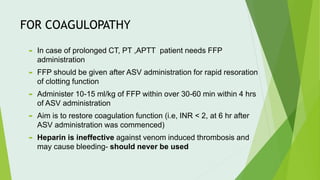
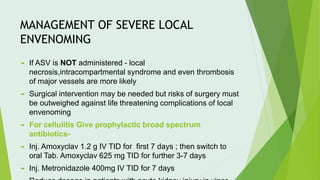
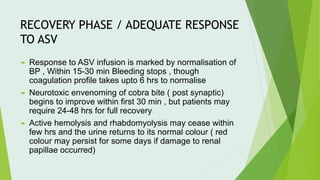
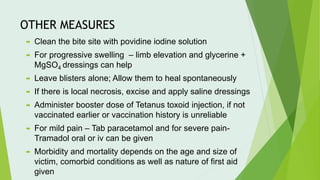
The document provides a comprehensive overview of snake bites, their management, and associated complications, highlighting the annual incidence of snakebites and the types of venomous snakes in India. It details the clinical presentation, the urgency of appropriate medical response, the application of antivenom, and specific treatment protocols based on the type of envenomation. It emphasizes the importance of rapid assessment, monitoring, and hospital management to mitigate life-threatening effects and complications from snake bites.