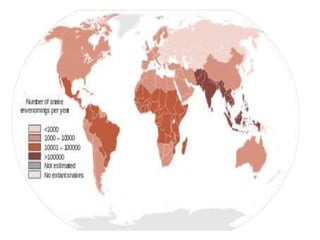
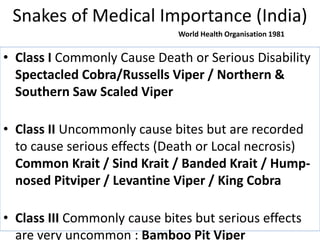
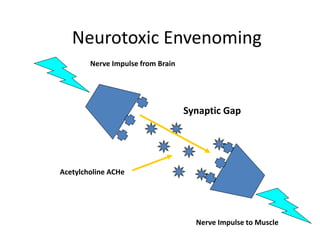
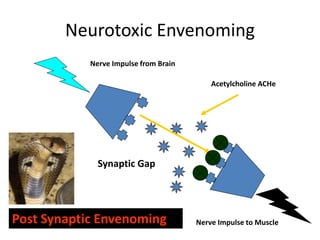
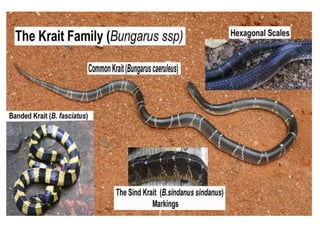
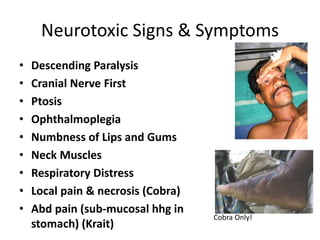
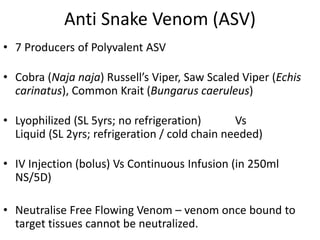
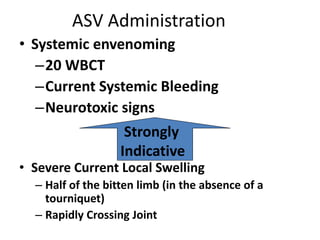
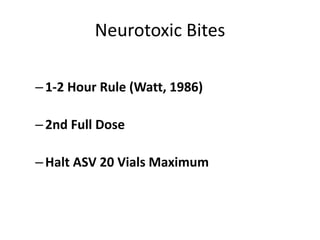
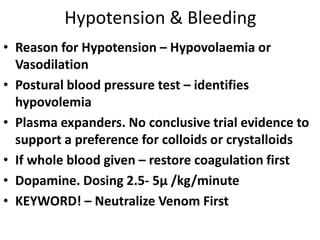
The document discusses the response to snake bites, highlighting the importance of accurate diagnosis and treatment protocols for envenomation, including the use of antivenom (ASV). It outlines various snake species, their associated risks, symptoms of envenomation, and effective first aid procedures, while also dispelling common misconceptions about treatment. Additionally, it emphasizes the need for immediate medical attention and proper monitoring of patients following a snake bite to ensure effective recovery.