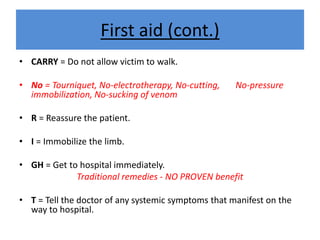
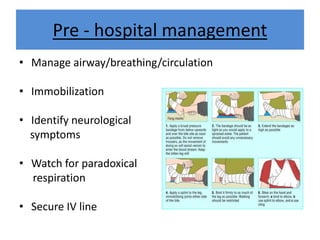
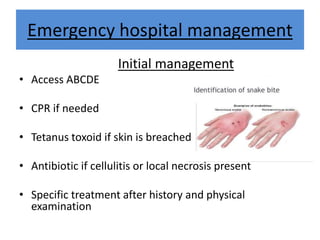
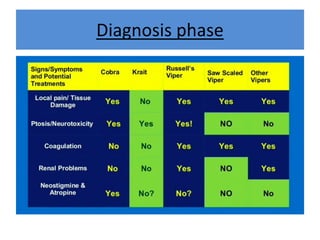
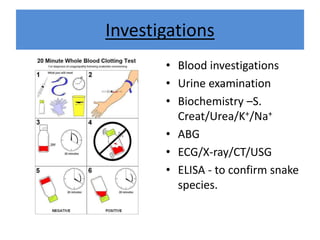
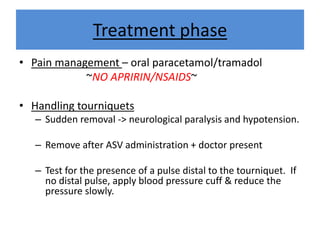
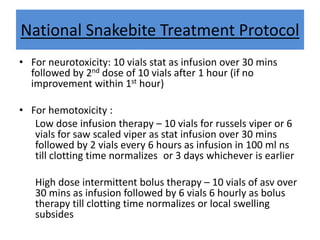
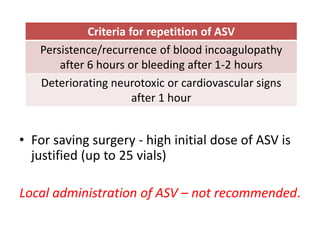
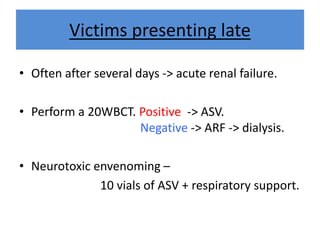
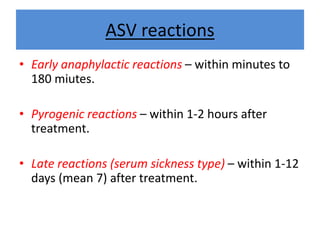
India experiences the highest snakebite mortality worldwide, with 2.8 million cases and 46,900 deaths annually. The document outlines the clinical features, first aid measures, and treatment protocols for snakebite management, highlighting the importance of emergency care, antivenom administration, and the role of supportive measures. Following WHO guidelines, it emphasizes the need for proper diagnosis and timely intervention to reduce morbidity and mortality associated with snakebite incidents.