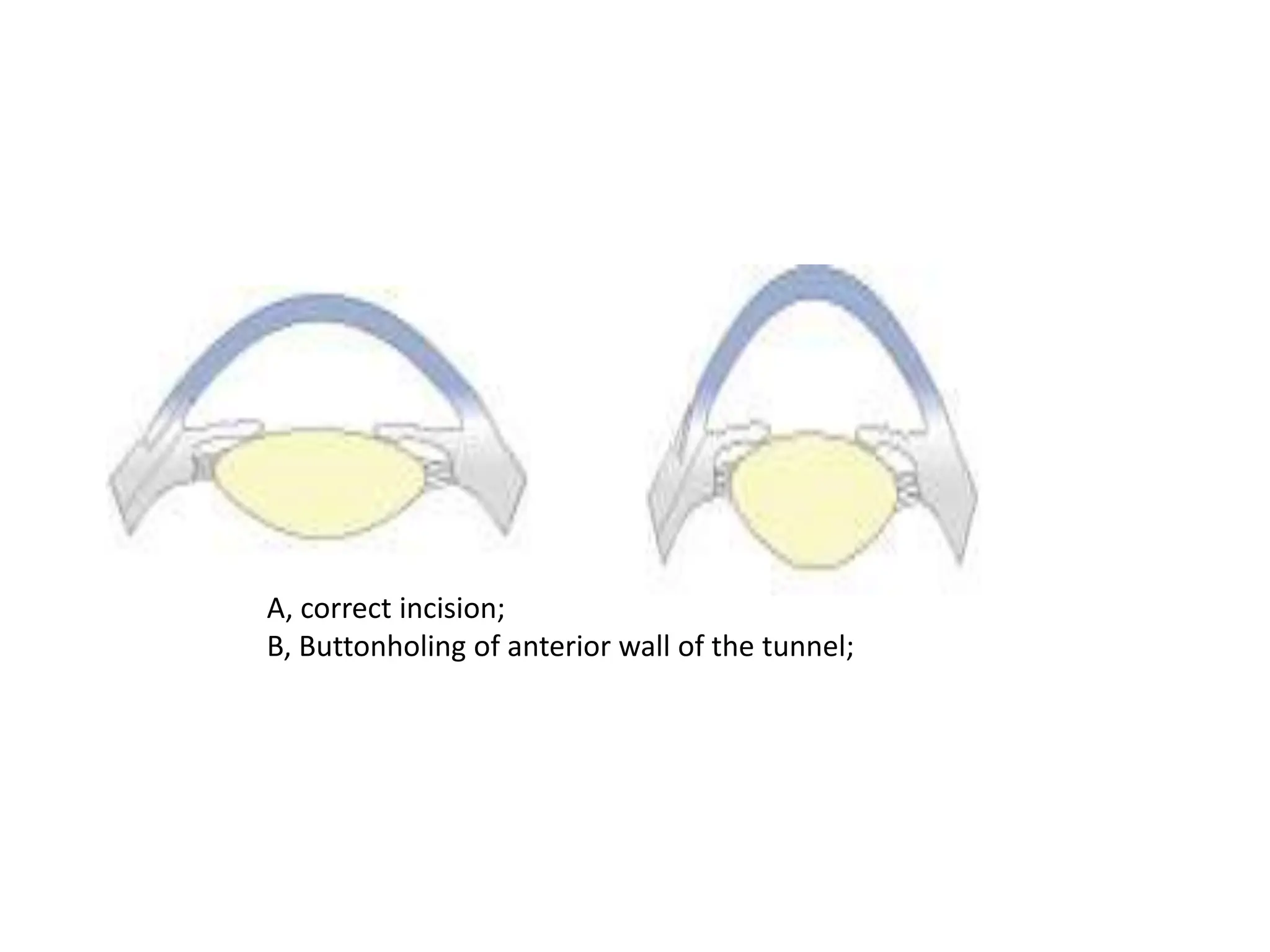
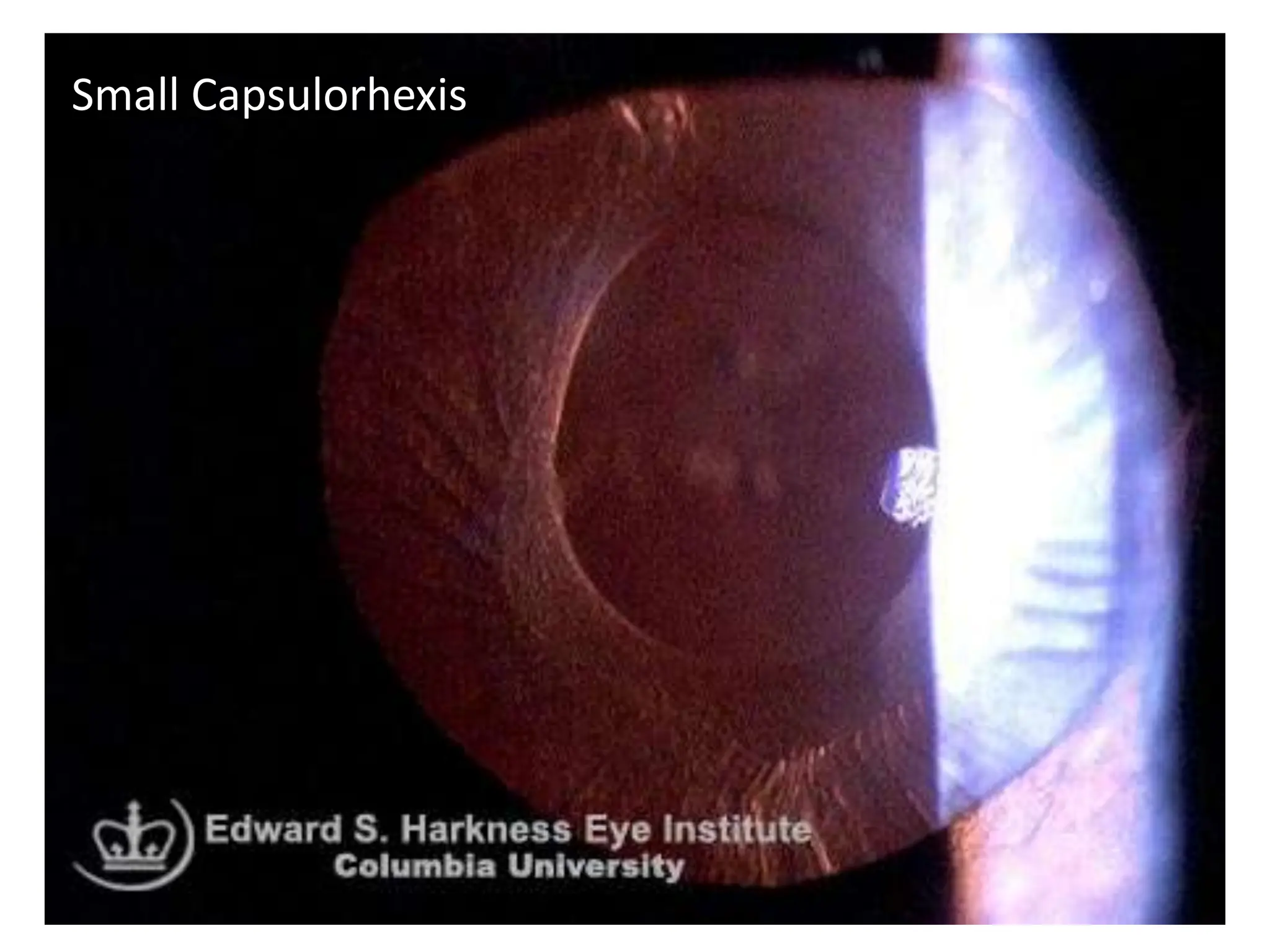
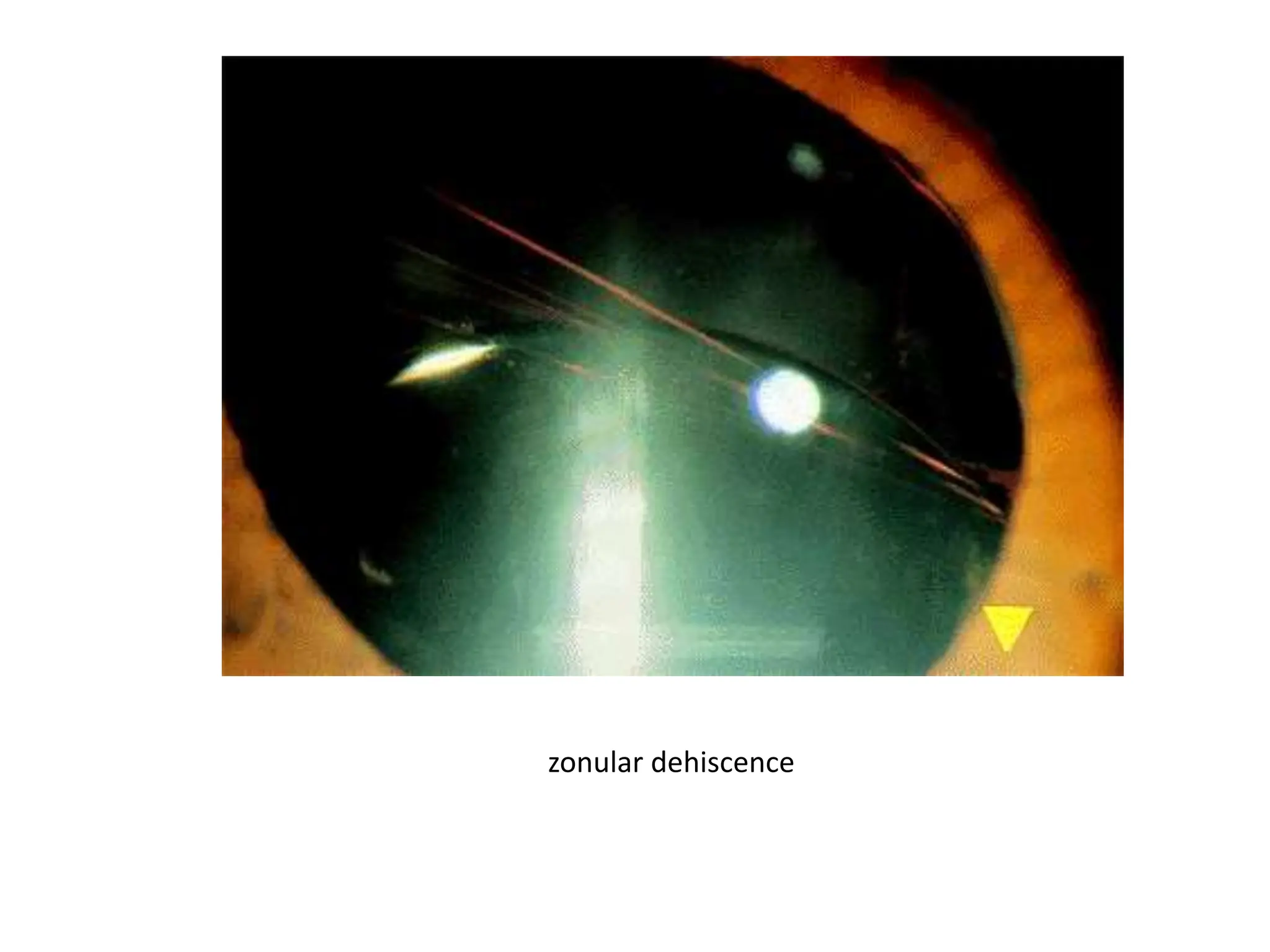
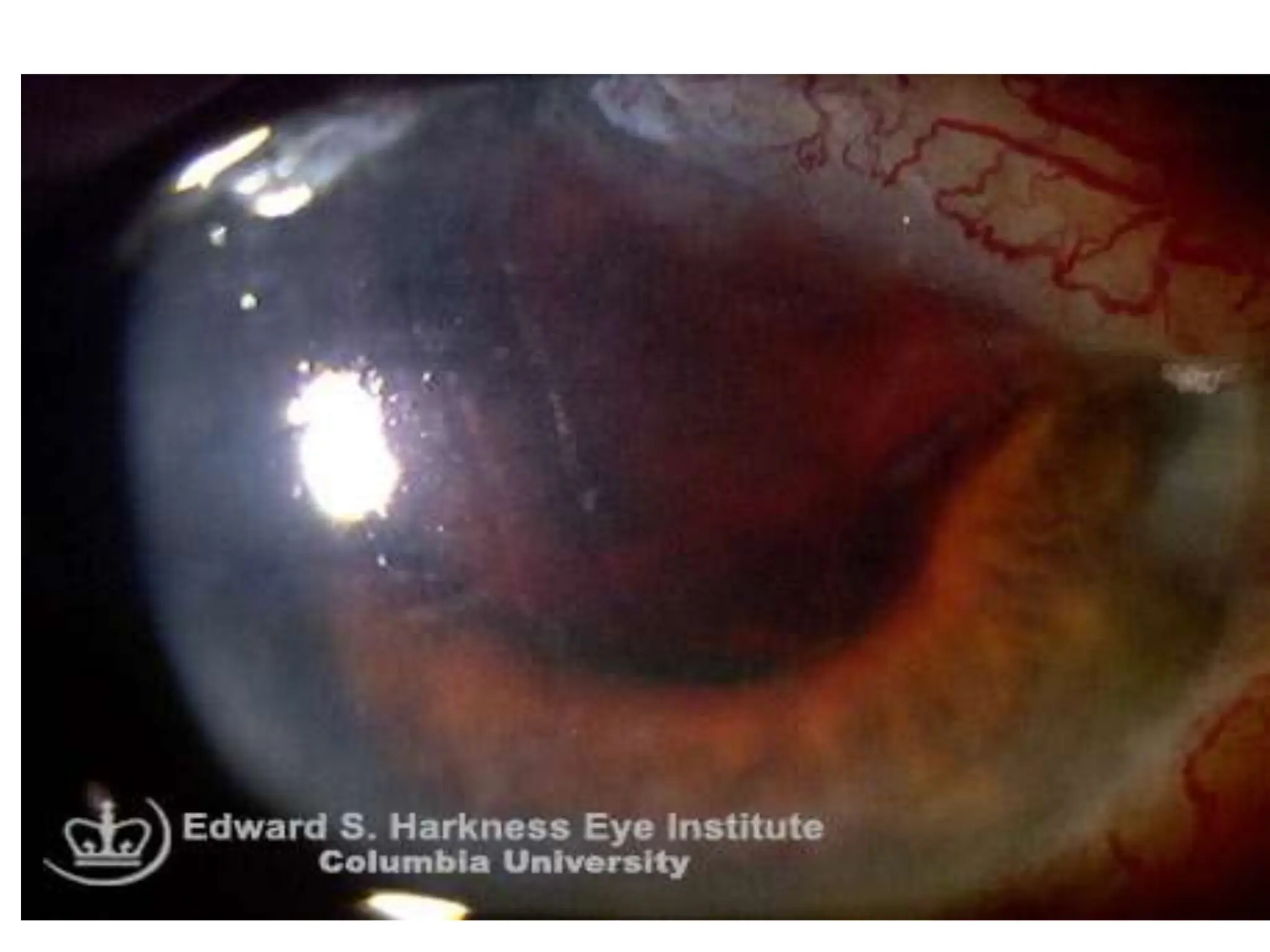
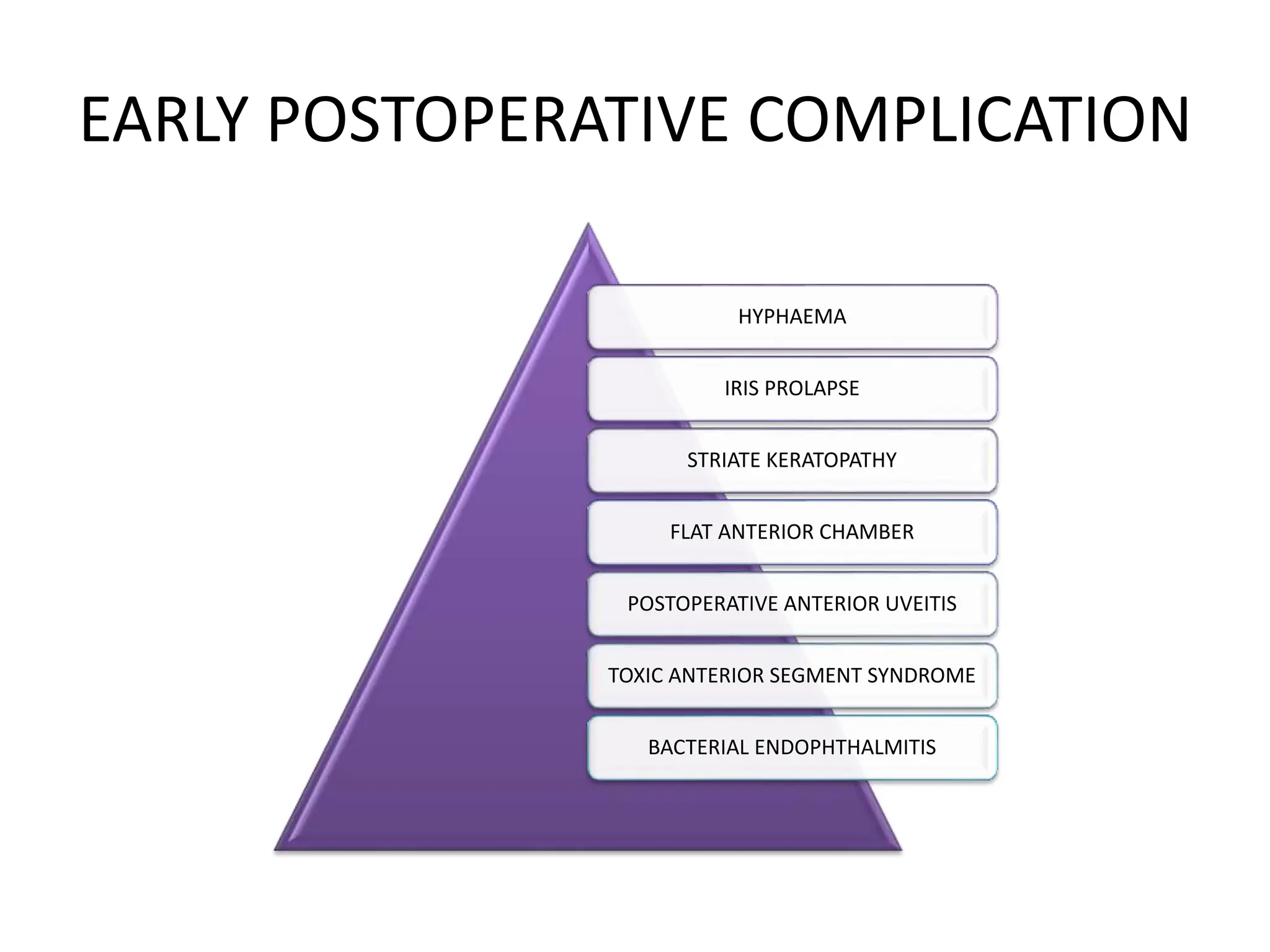
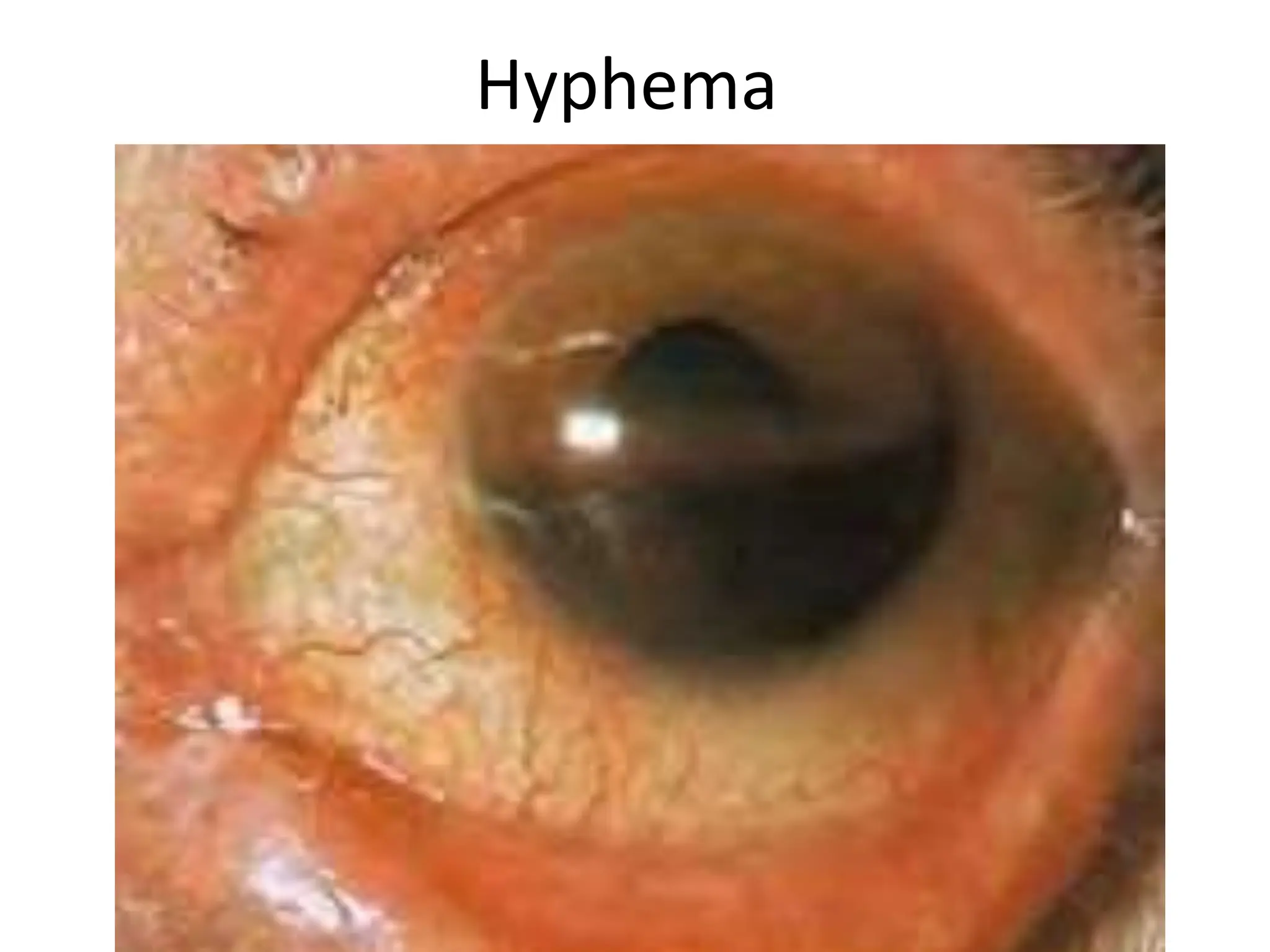
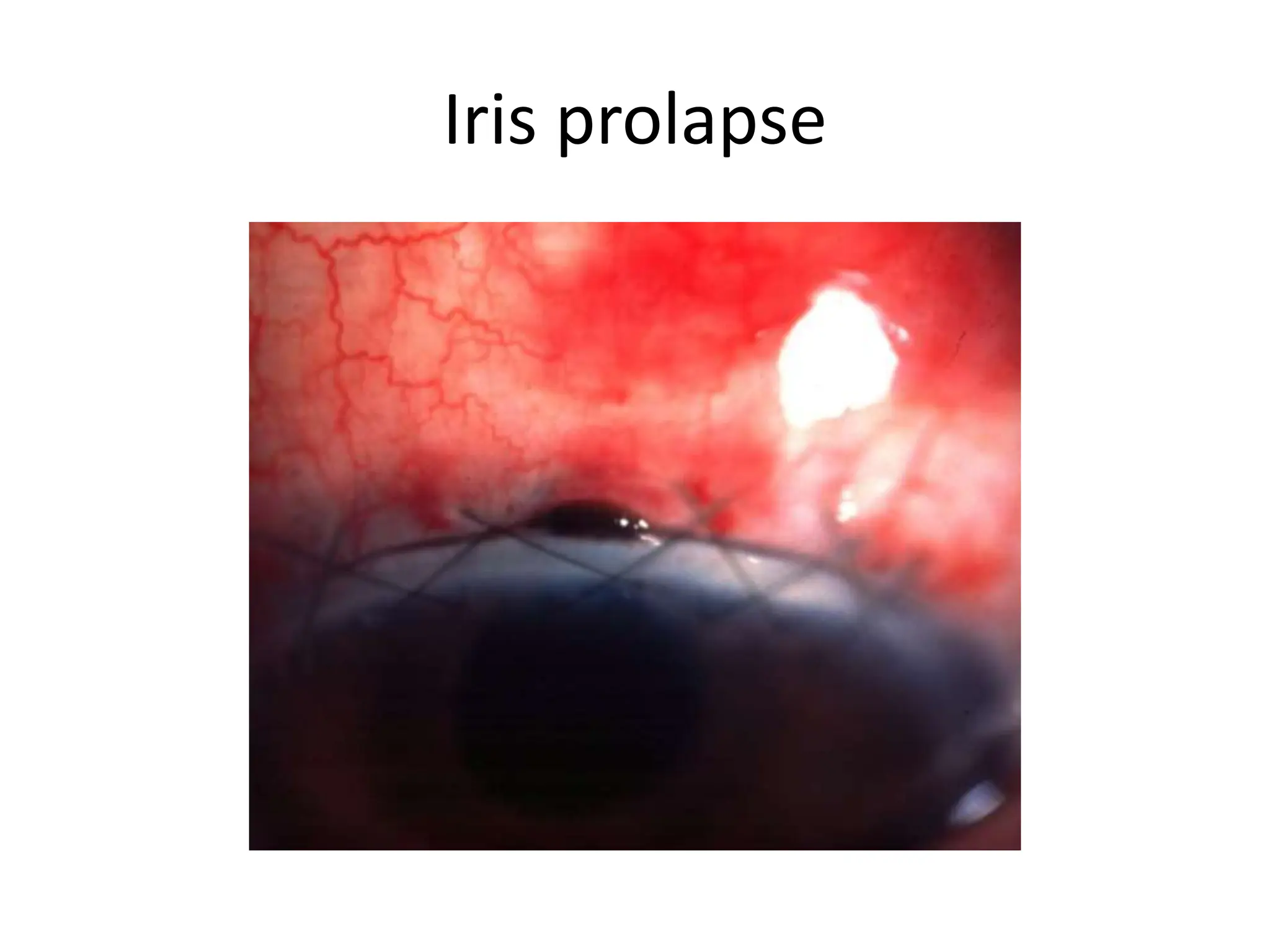
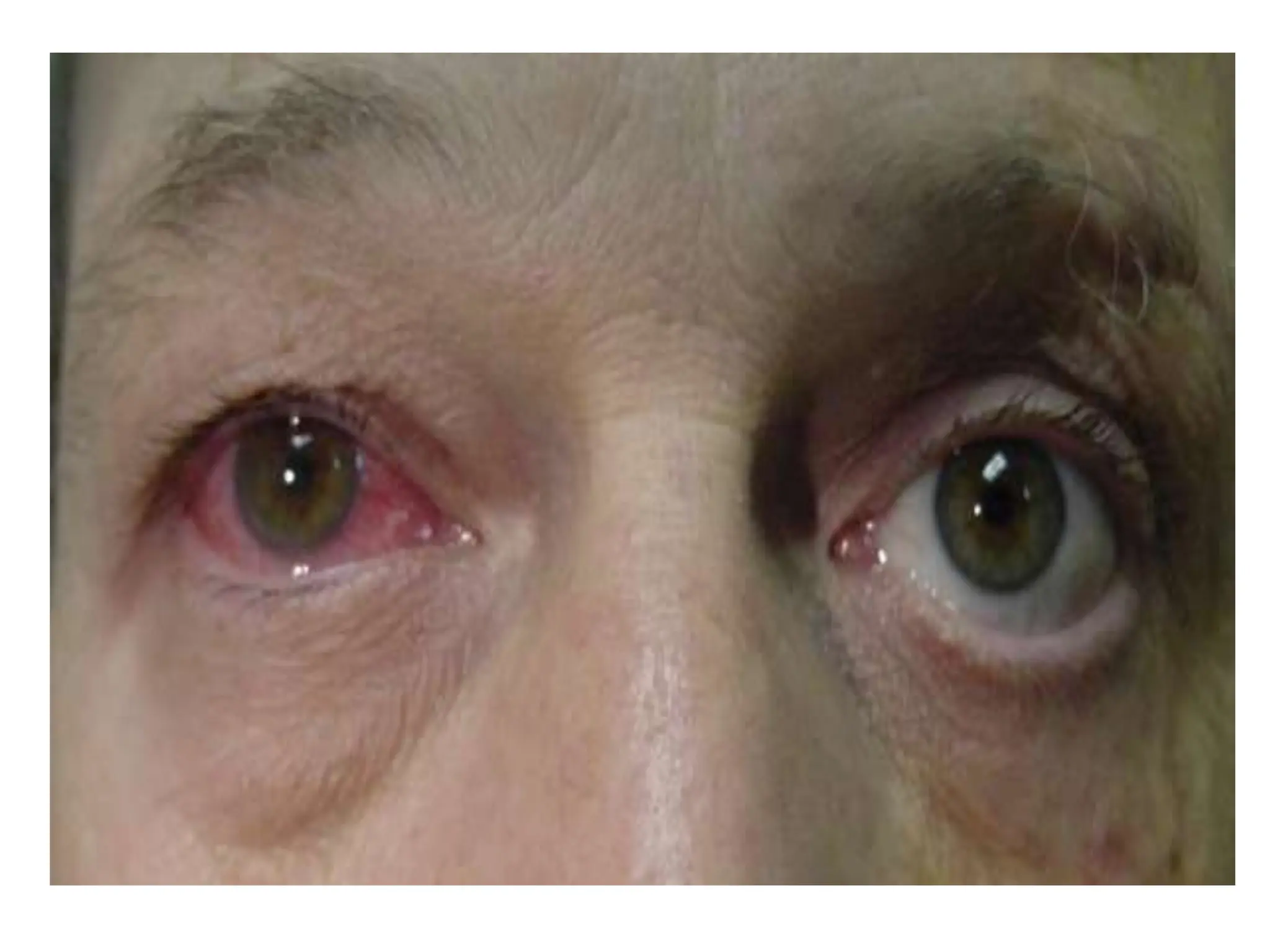
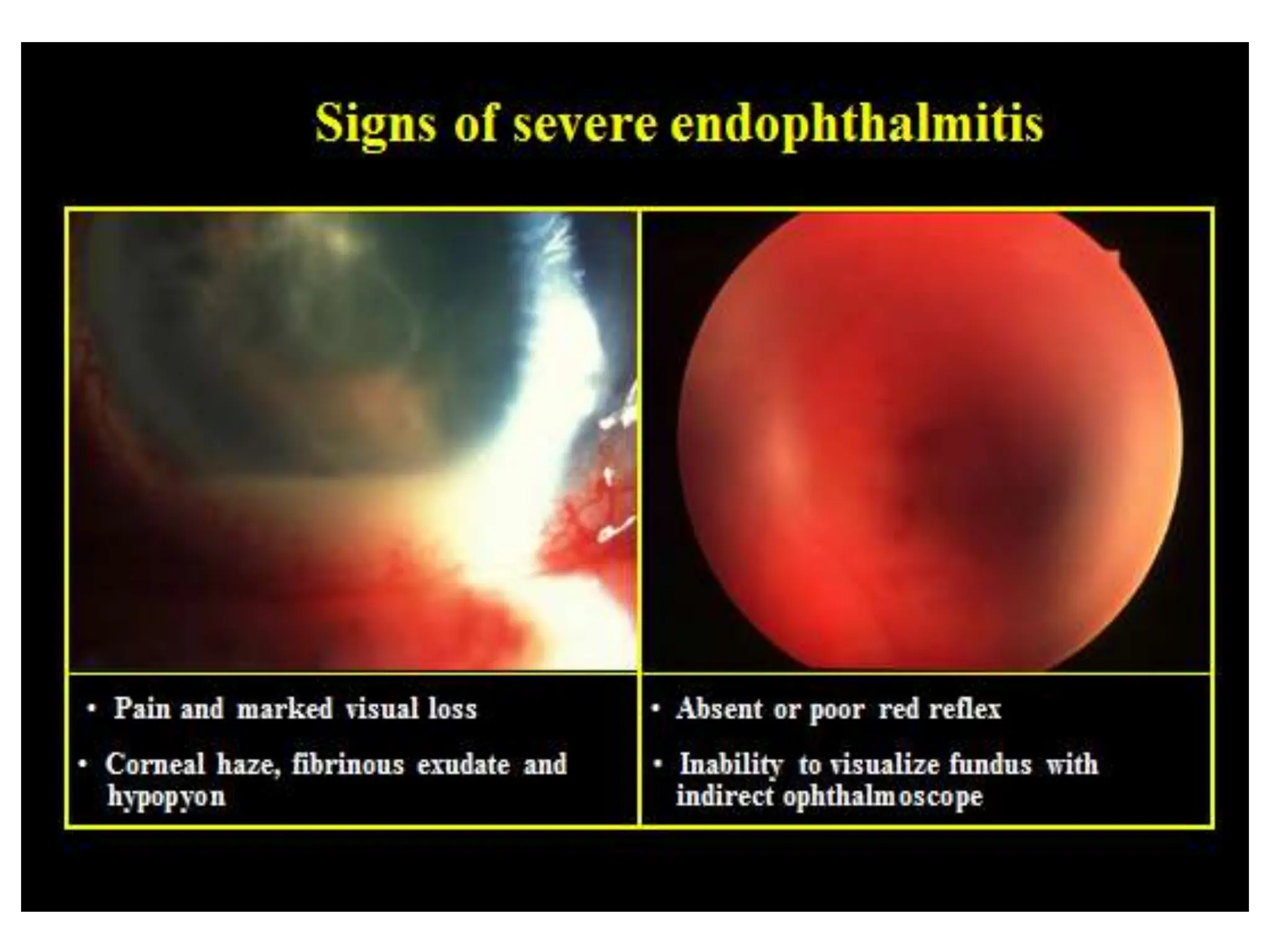
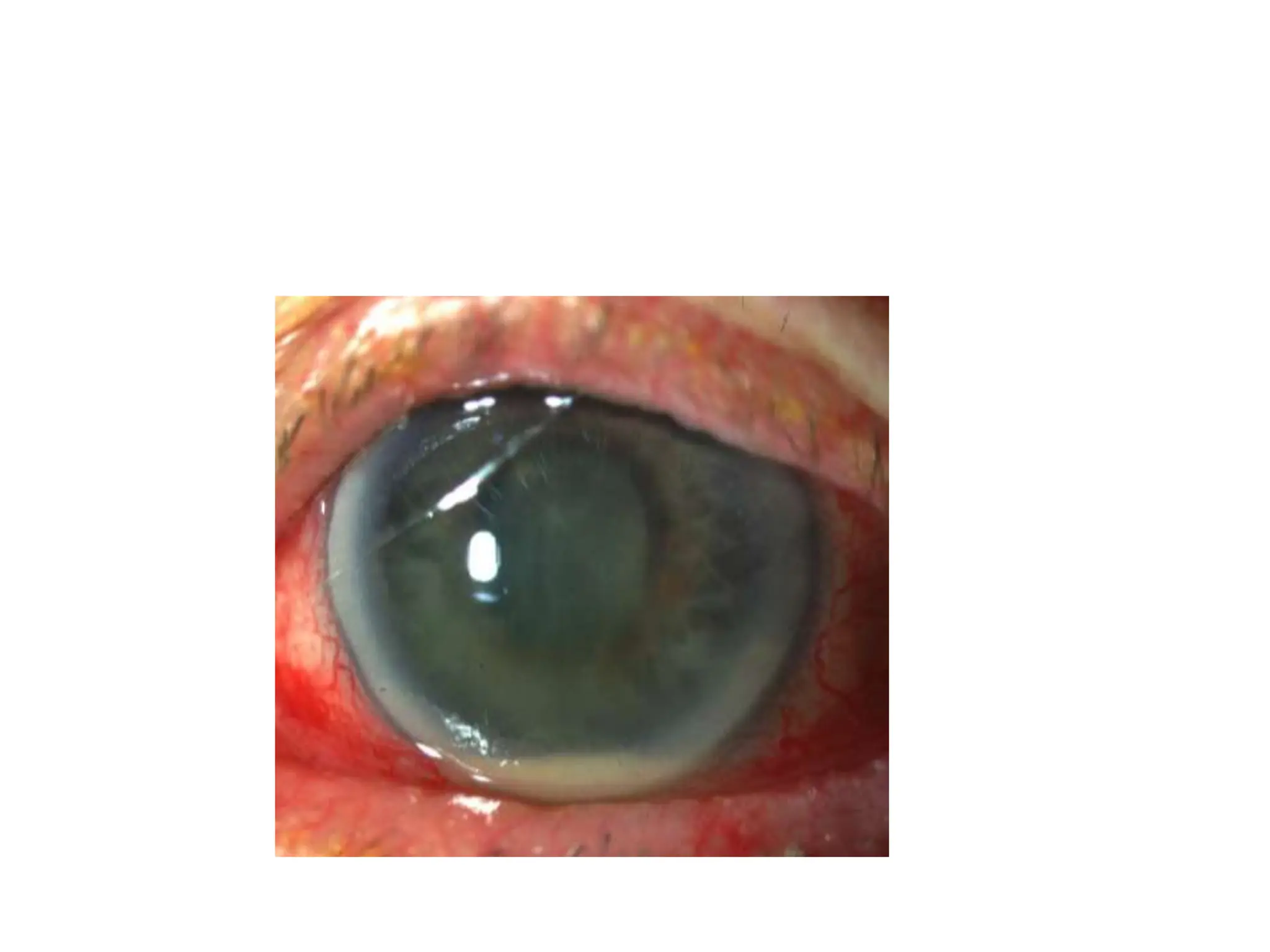
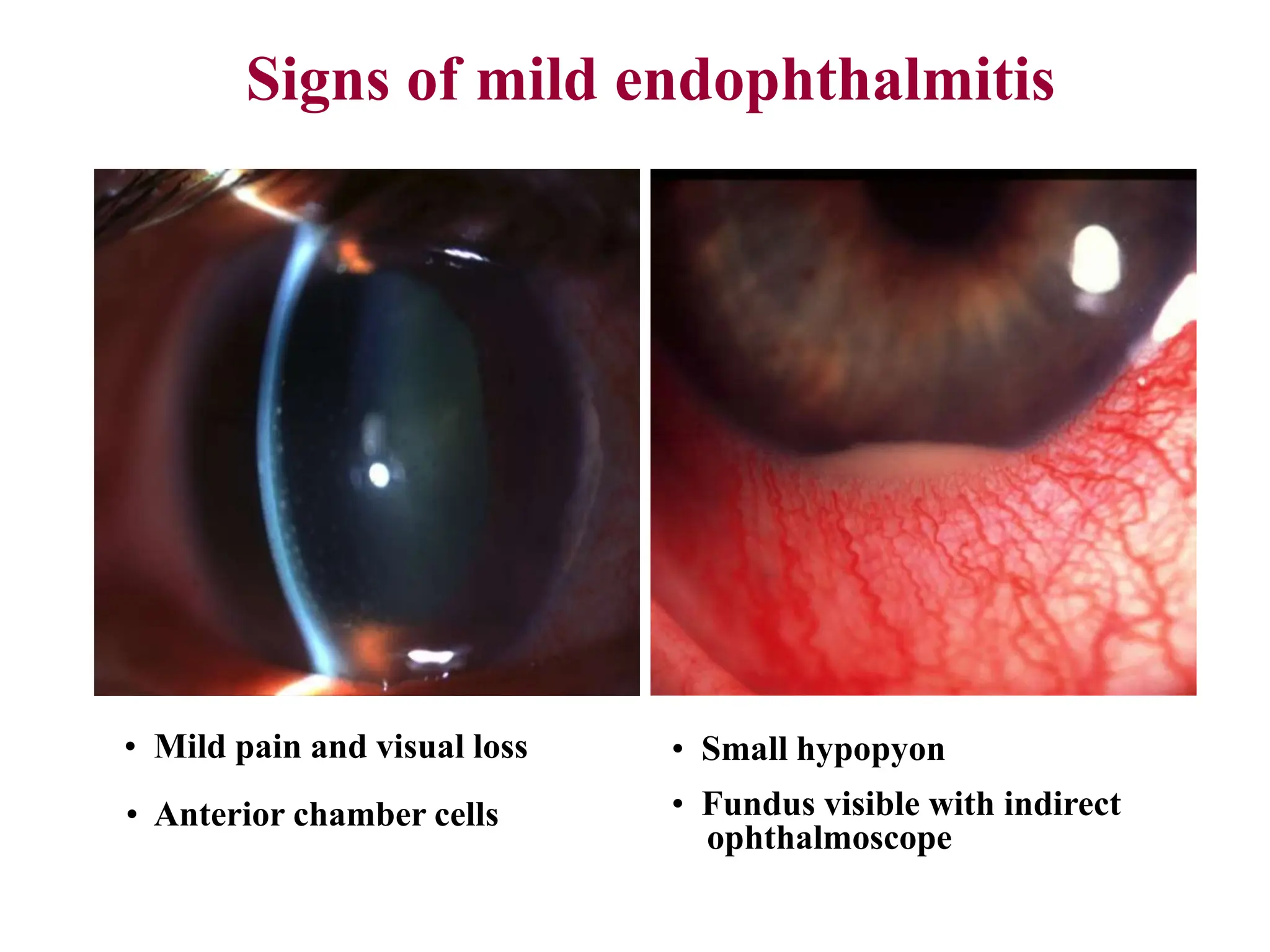
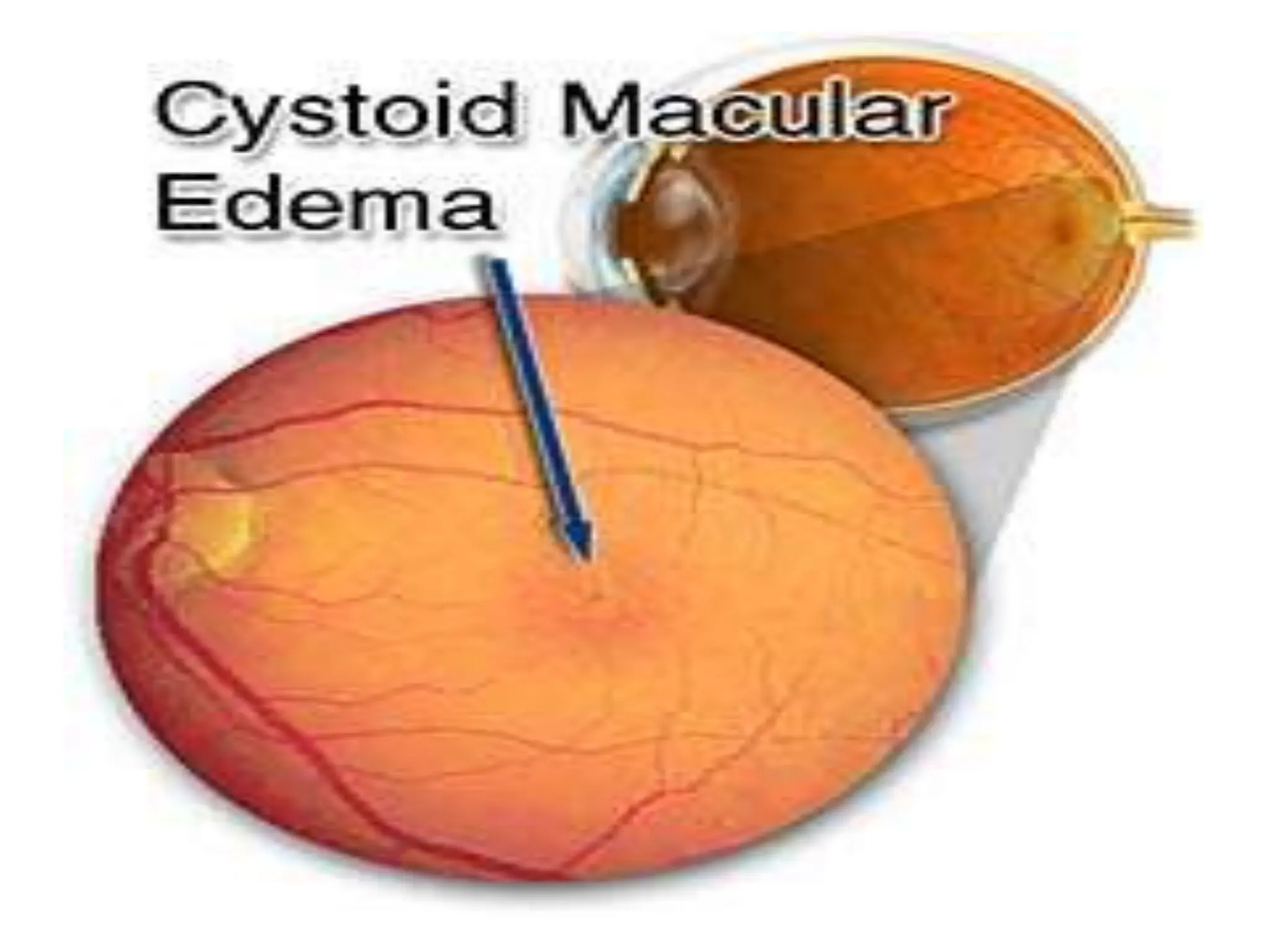
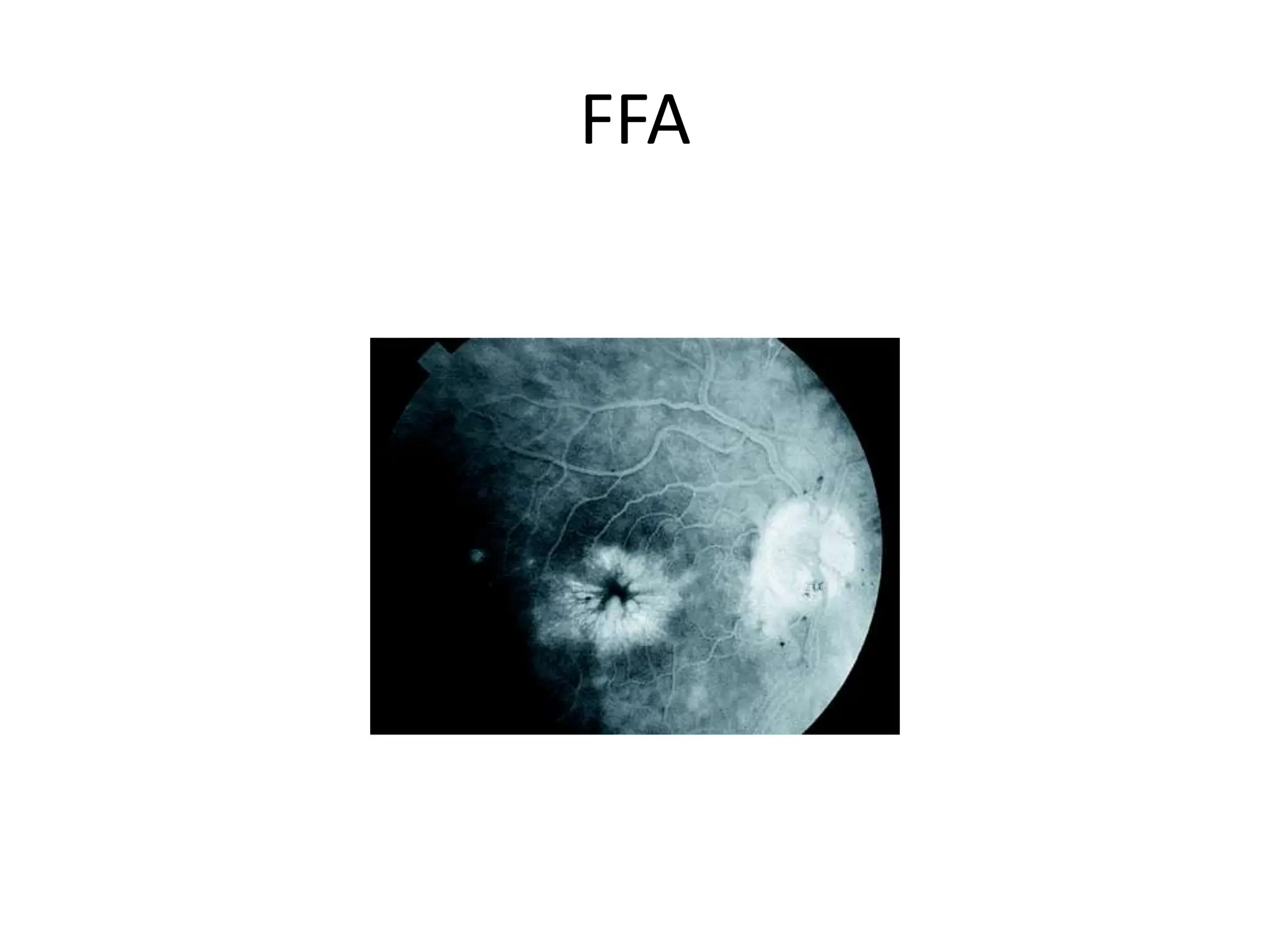
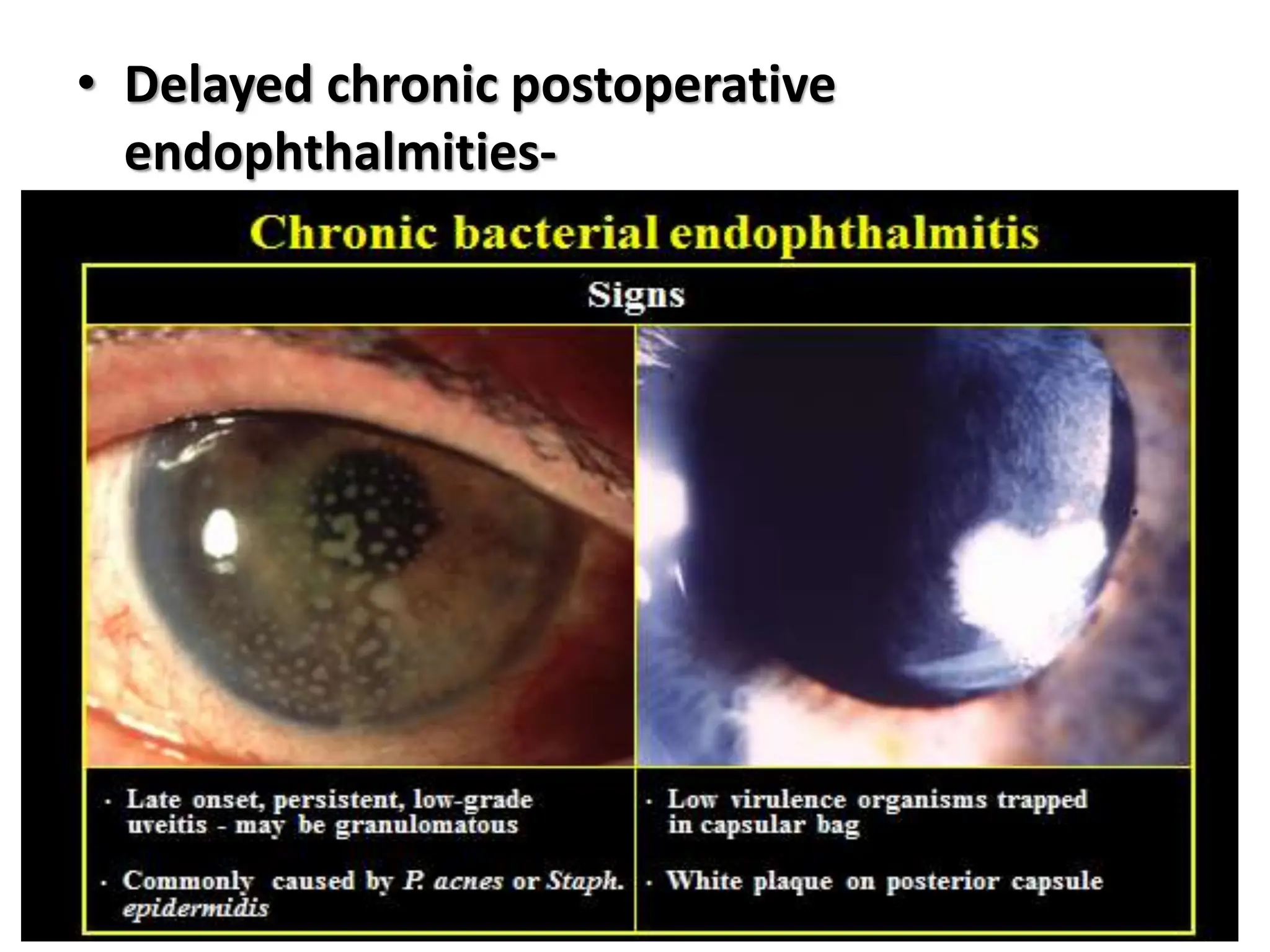
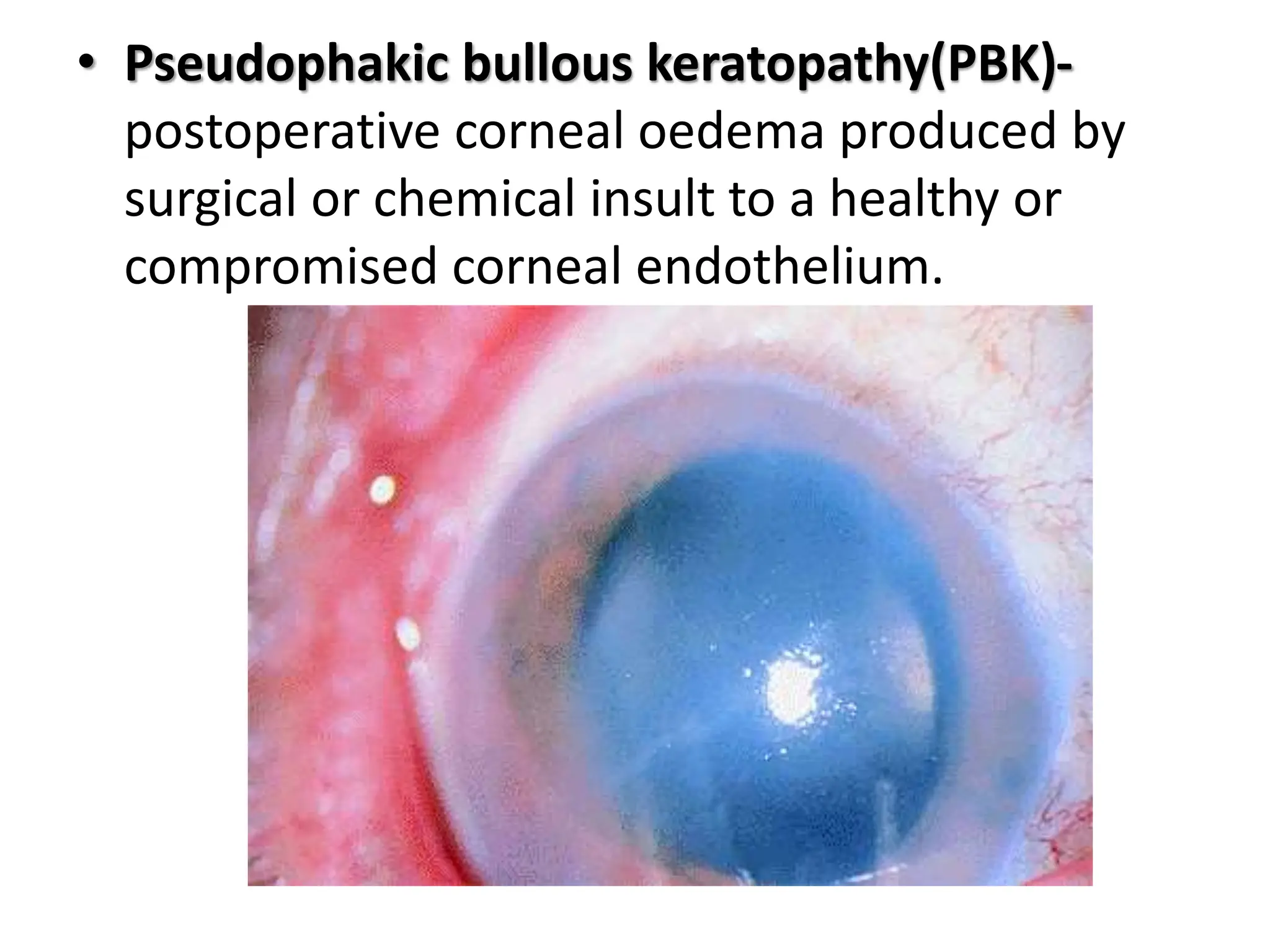
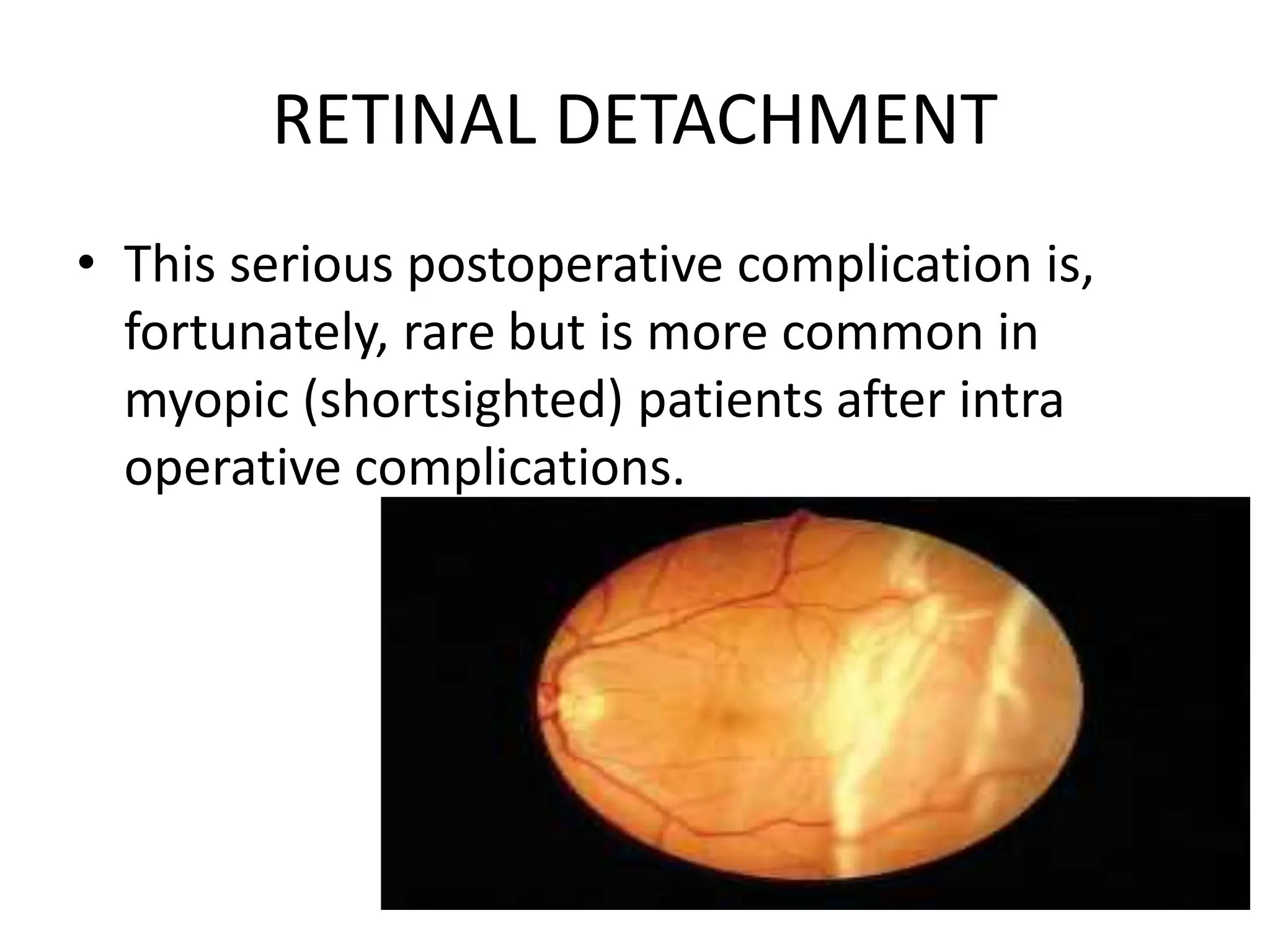
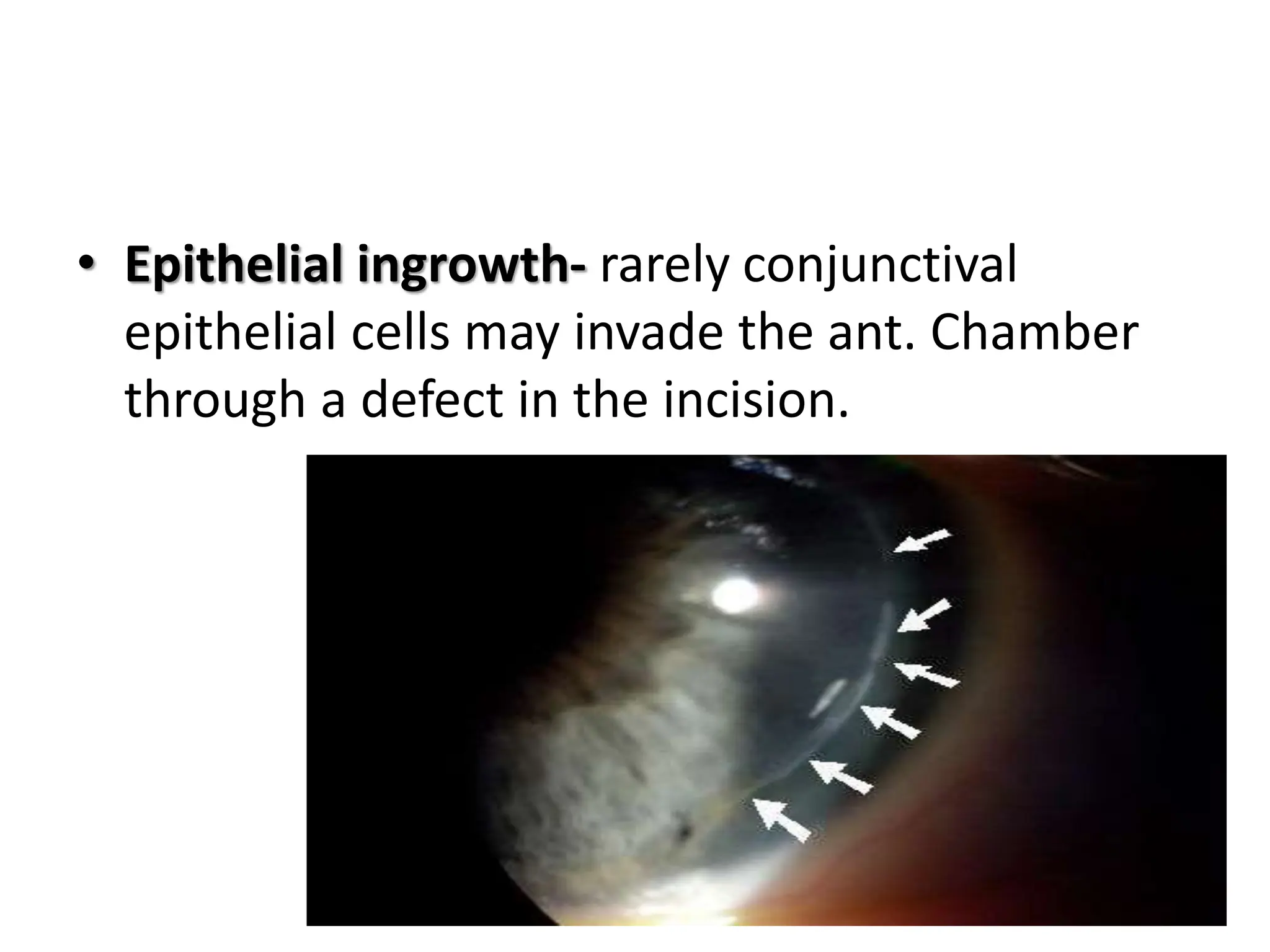
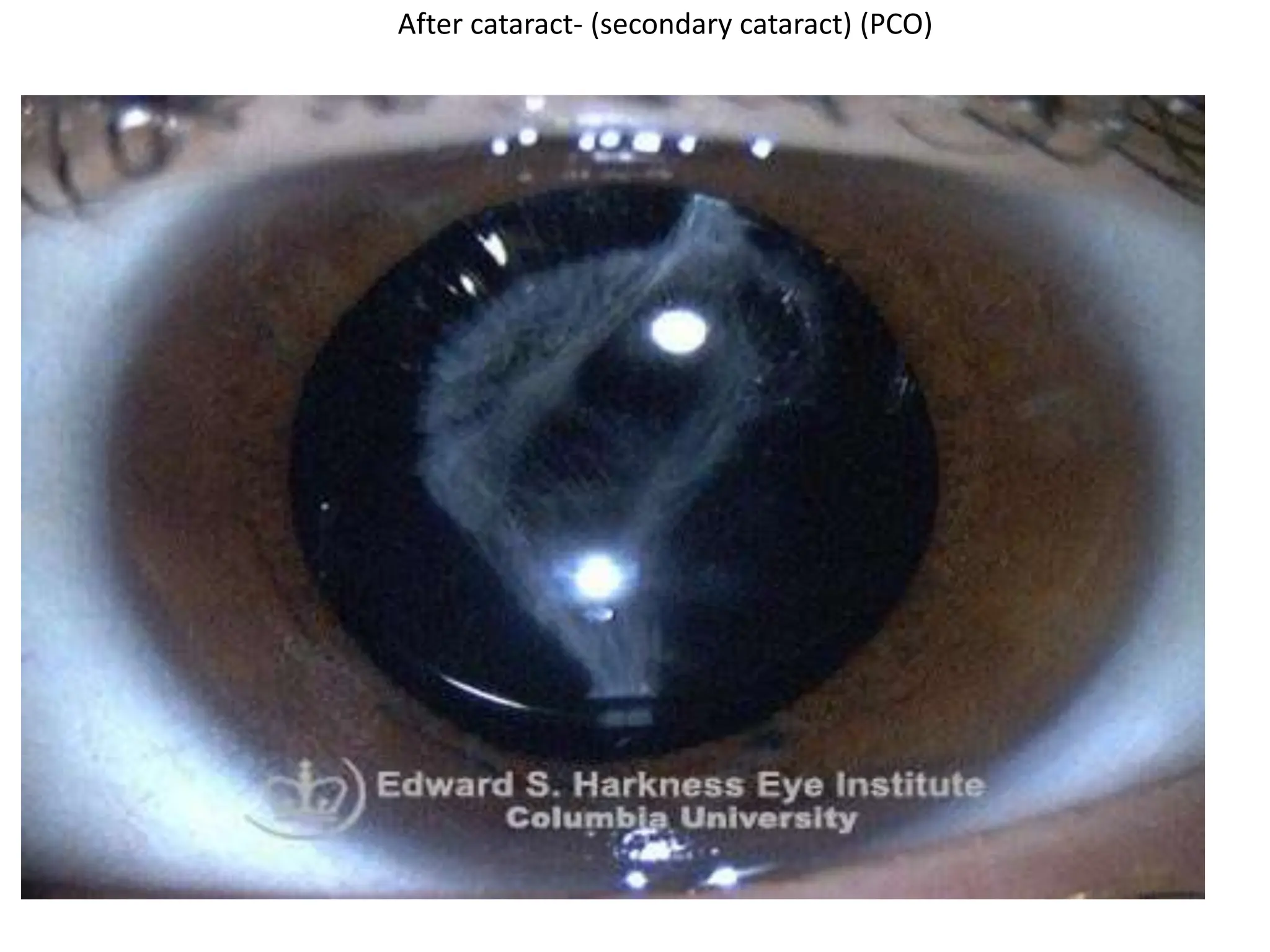
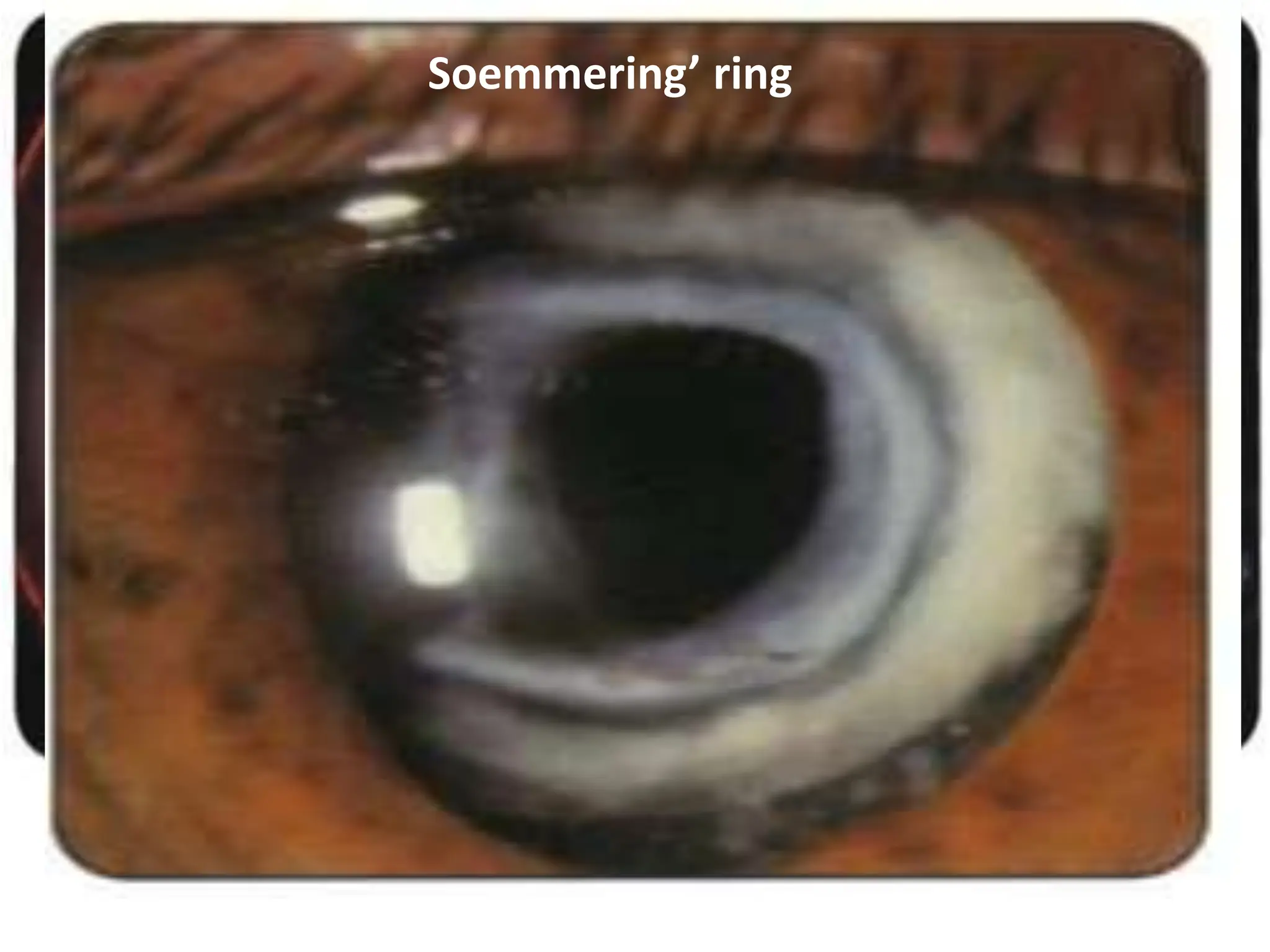
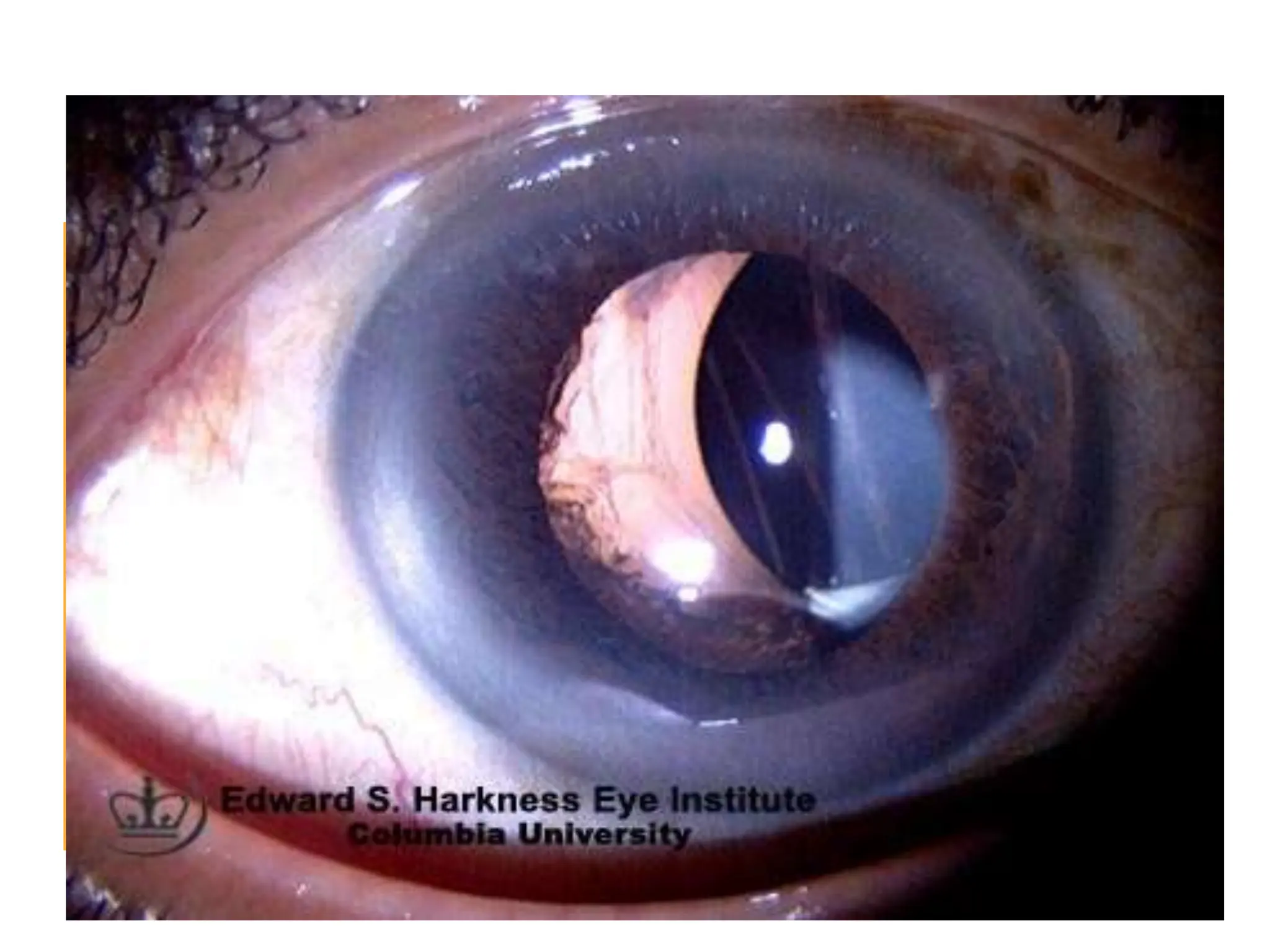
The document summarizes various potential complications that can occur during and after cataract surgery. It describes preoperative complications such as anxiety, nausea, allergic conjunctivitis, corneal abrasion, and issues with local anesthesia. Operative complications include injuries to tissues in the eye from surgical instruments as well as issues like posterior capsule rupture. Early postoperative complications include hyphaema, iris prolapse, and endophthalmitis. Late postoperative complications include cystoid macular edema, retinal detachment, and glaucoma. The document also discusses complications related to intraocular lenses like malpositioning and pupillary capture of the IOL.