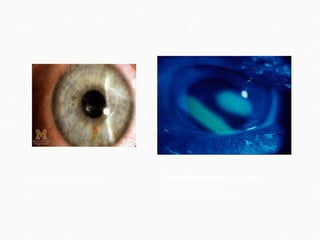
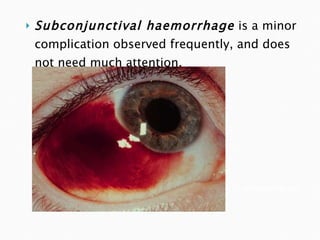
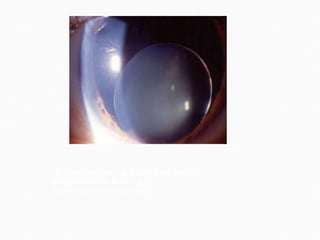
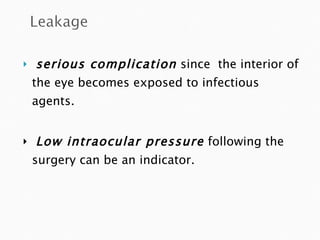
Some potential complications from cataract surgery include: corneal abrasion from Schiotz tonometry; retrobulbar hemorrhage from retrobulbar block requiring pressure bandaging; oculocardiac reflex from retrobulbar block treated with atropine; perforated globe risk minimized with gentle injection; subconjunctival hemorrhage requiring no treatment. Posterior dislocation of the lens during retrobulbar block requires postponing surgery and managing as a posterior dislocation.












![Small pupil Prolonged phaco time [hard cataracts] Posterior capsular rupture Corneal thermal burns Intraoperative detection or occurrence of subluxation Malfunction of handpiece or machine](https://image.slidesharecdn.com/complicationsof-110319084701-phpapp01/85/Complications-of-118-320.jpg)