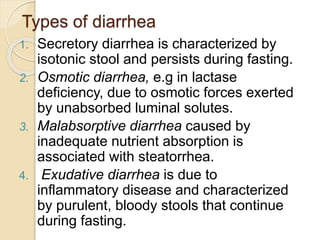
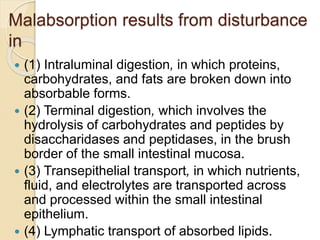
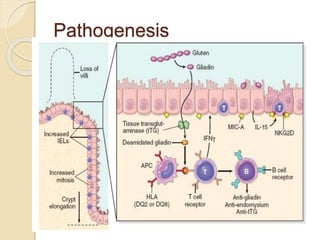
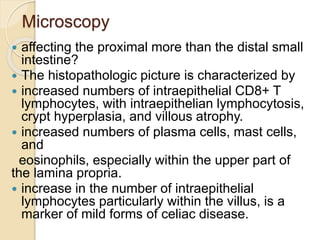
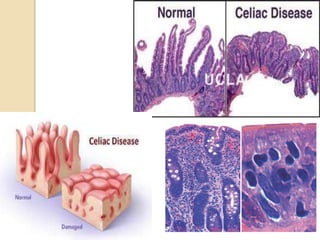
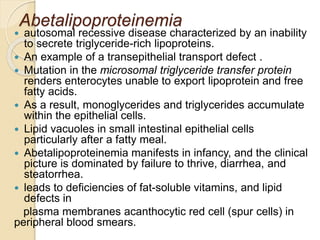
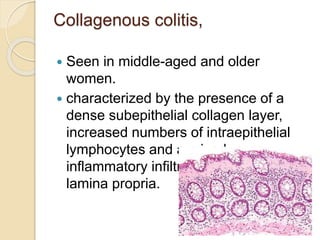
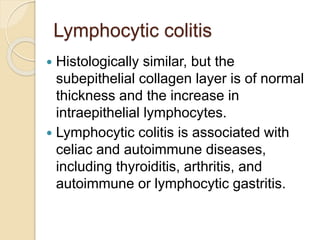
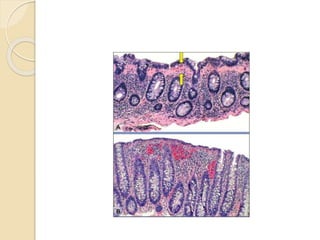
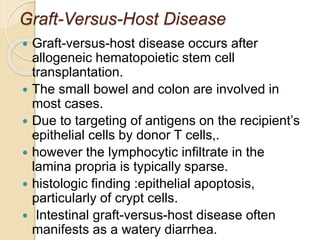
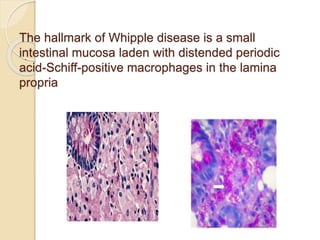
Malabsorption results from defects in intraluminal digestion, terminal digestion, transepithelial transport, and lymphatic transport. It is characterized by weight loss, abdominal distention, diarrhea, and steatorrhea. Causes of malabsorption include cystic fibrosis, celiac disease, lactase deficiency, environmental enteropathy, abetalipoproteinemia, microscopic colitis, graft-versus-host disease, and Whipple's disease. Histological examination often reveals villous atrophy, increased intraepithelial lymphocytes, and lipid-laden macrophages in the lamina propria.