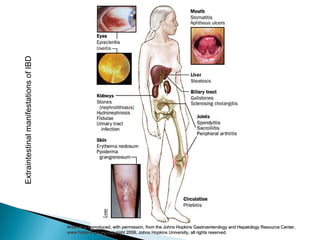
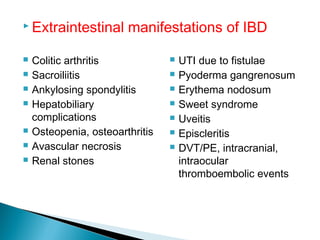
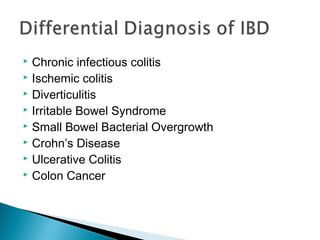
1) Inflammatory bowel disease (IBD) includes Crohn's disease and ulcerative colitis, which are chronic inflammatory disorders of the gastrointestinal tract of unknown cause.
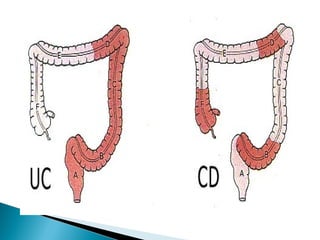
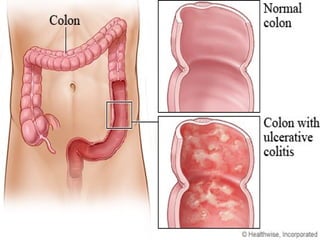
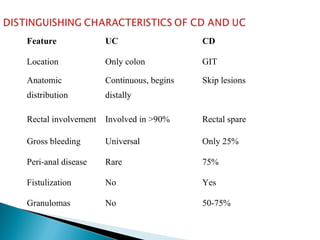
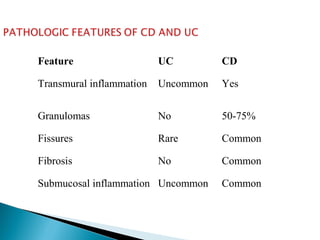
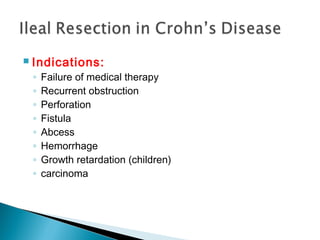
2) Crohn's disease can affect any part of the GI tract and causes granulomatous inflammation, while ulcerative colitis causes non-granulomatous inflammation of the rectum and colon.
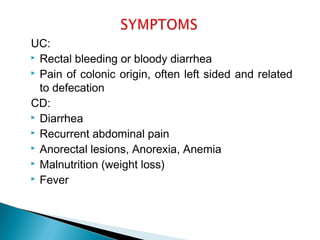
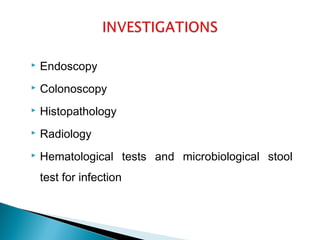
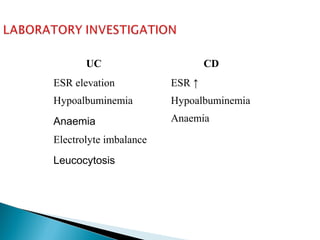
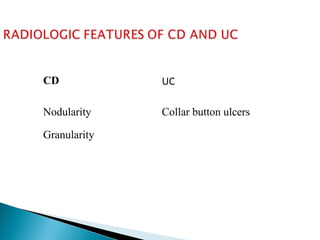
3) Symptoms of IBD include diarrhea, abdominal pain, rectal bleeding, weight loss, and malnutrition. Diagnostic tests include endoscopy, colonoscopy, imaging, and lab tests.
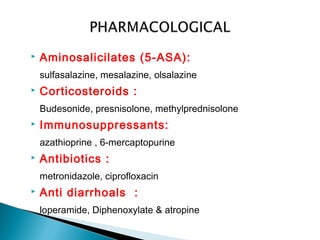
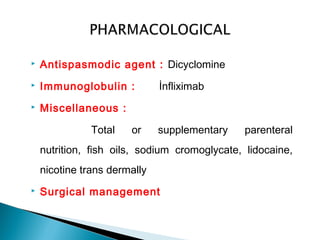
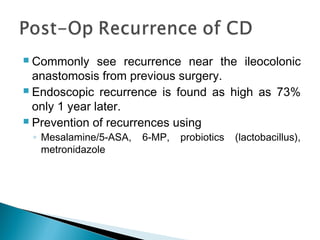
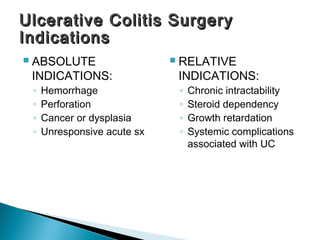
4) Treatment involves medications to reduce inflammation like aminosal