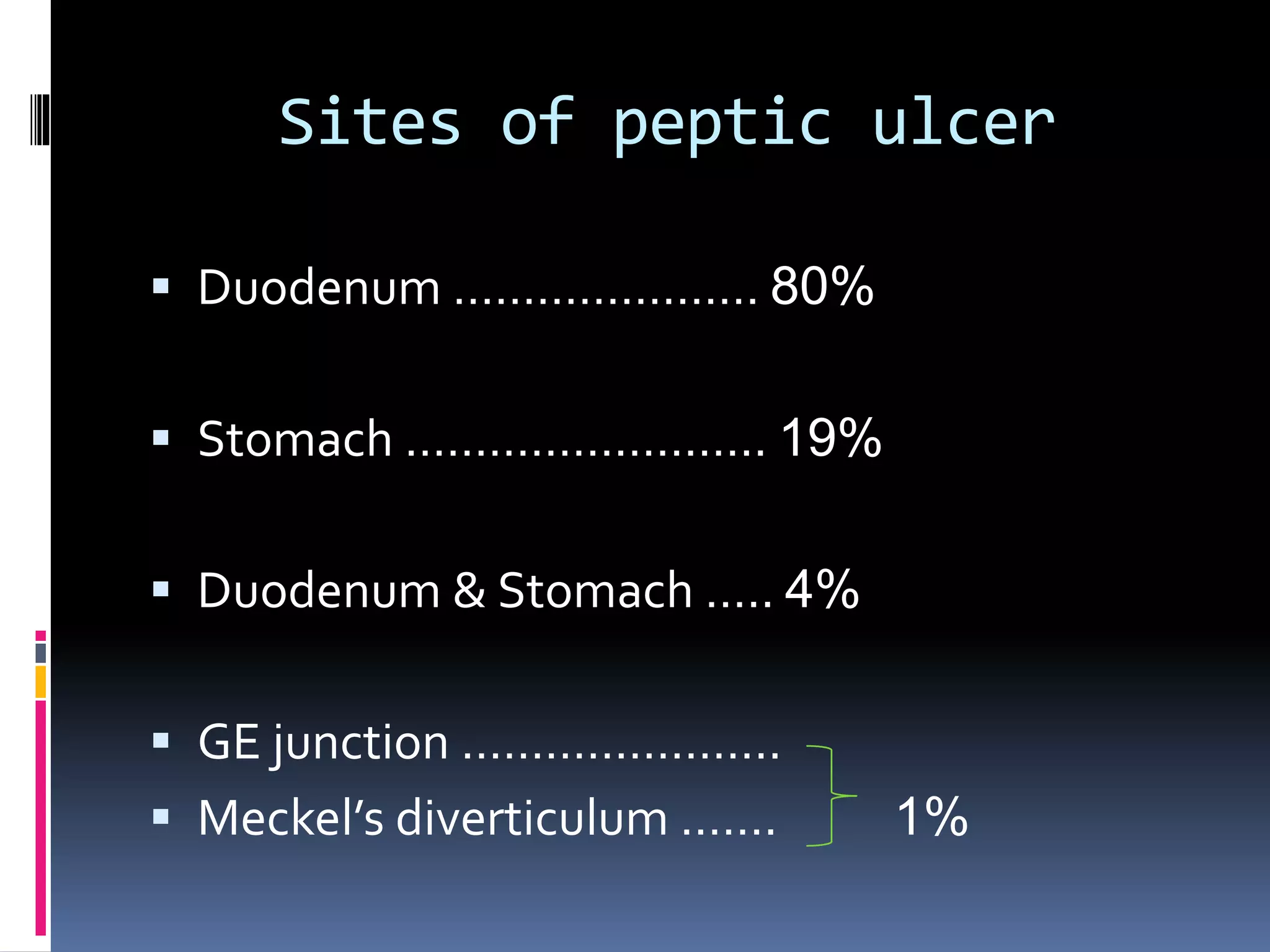
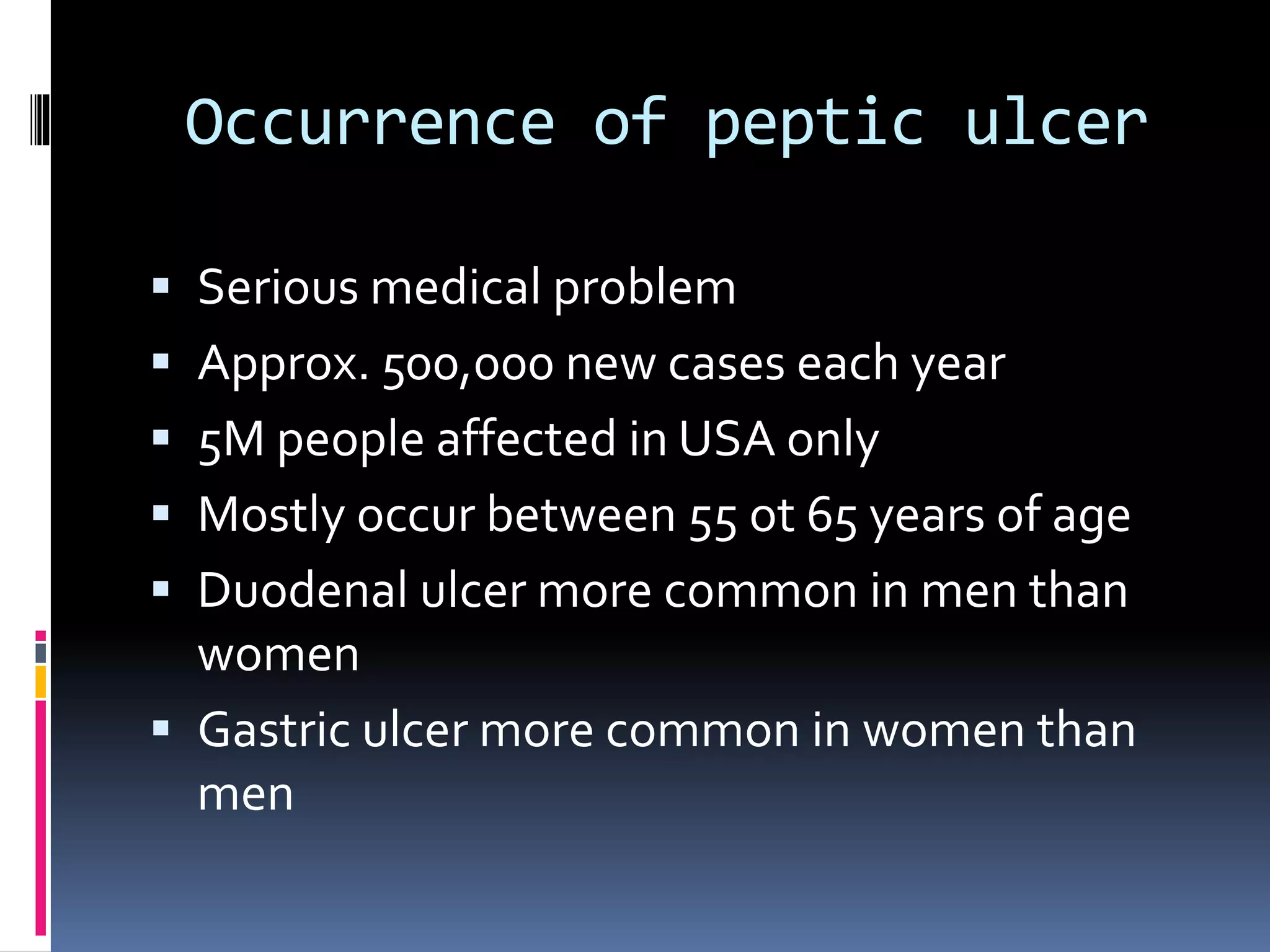
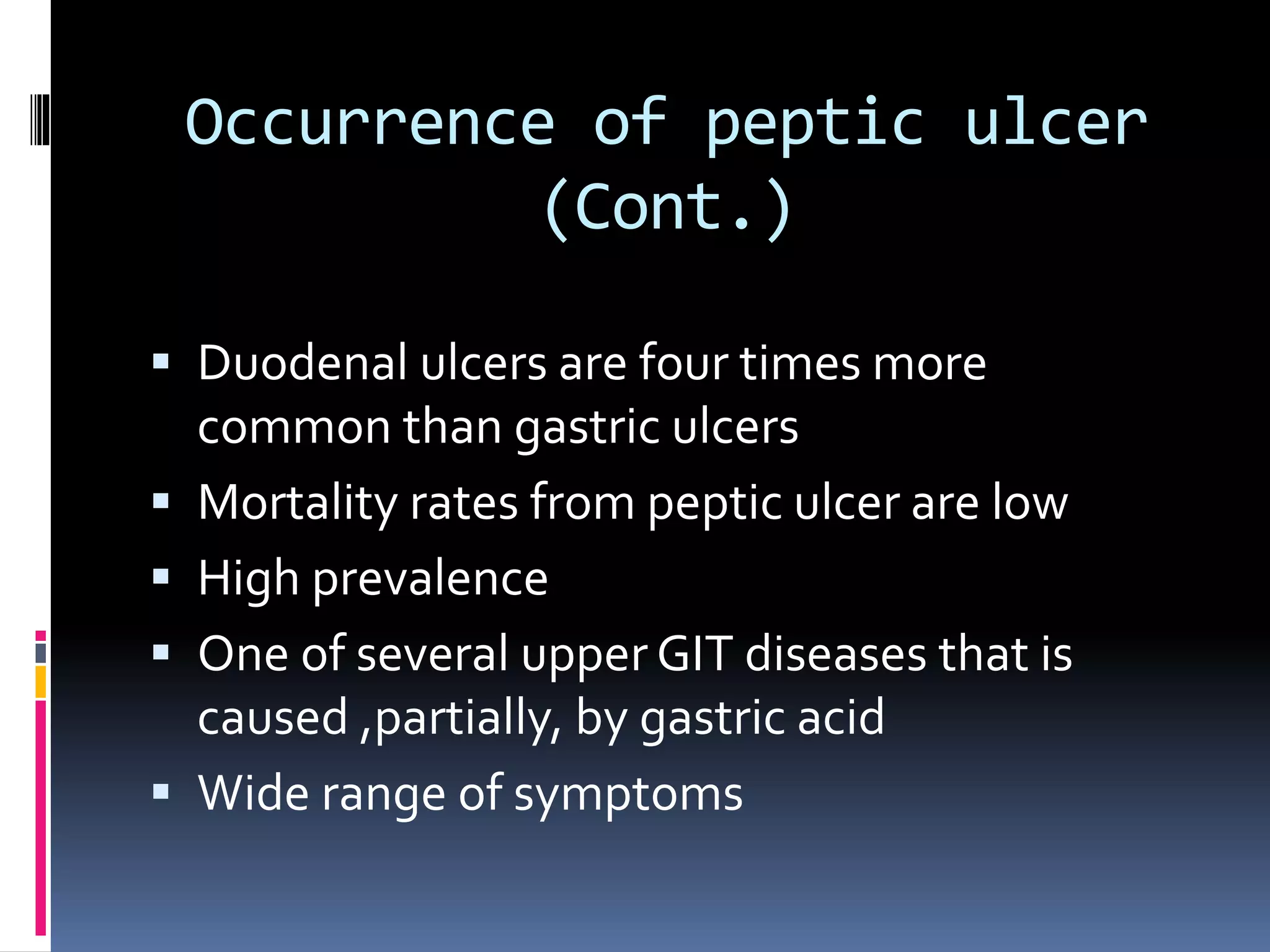
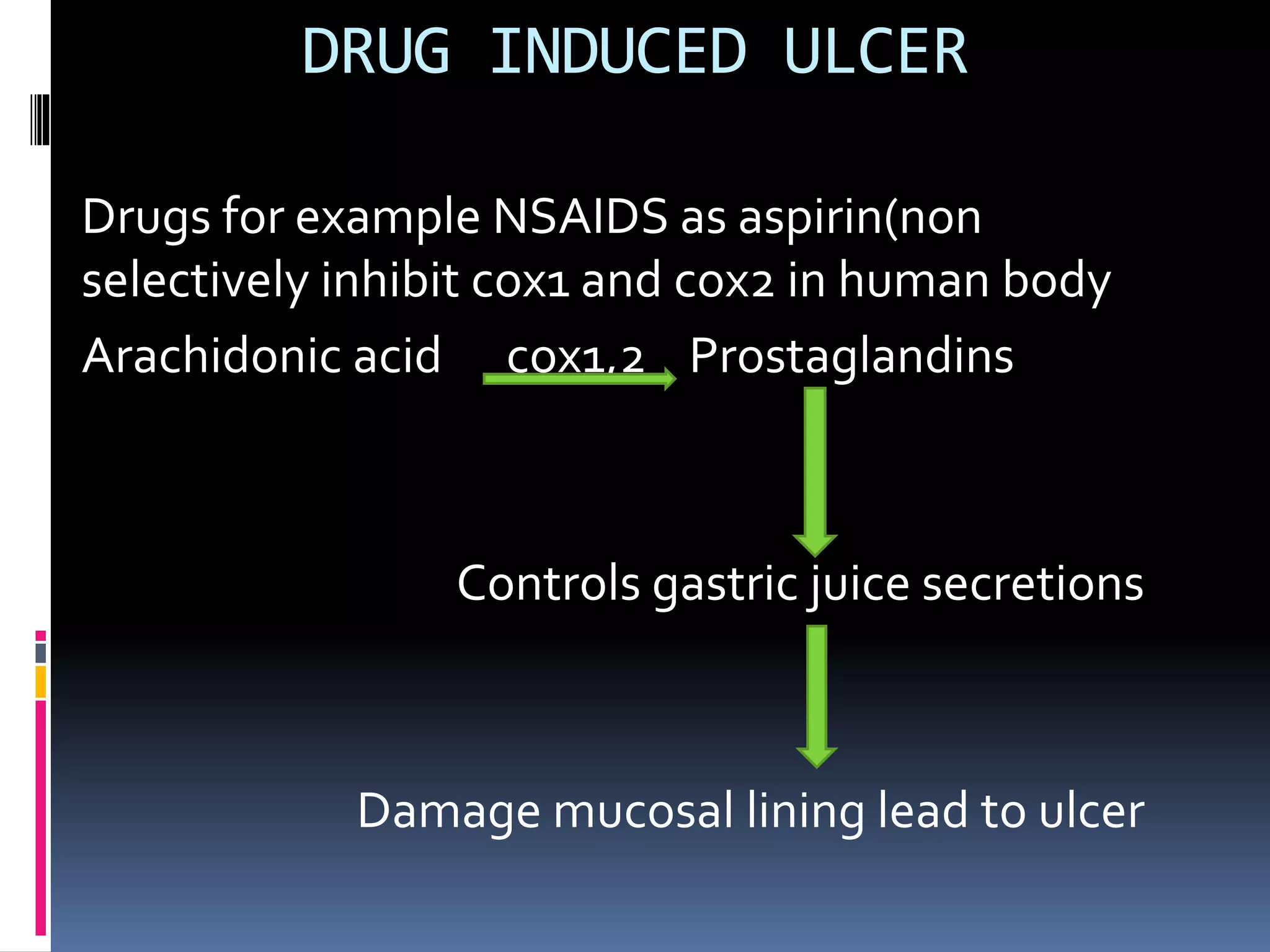
This document provides information about peptic ulcers, including their types, causes, symptoms, and treatment. It discusses the different types of peptic ulcers that can occur in the stomach, duodenum, and esophagus. The main causes of peptic ulcers are infection with Helicobacter pylori bacteria and use of non-steroidal anti-inflammatory drugs. Common symptoms include abdominal pain, nausea, vomiting, and weight loss. Treatment involves lifestyle changes, medications to reduce acid production or treat H. pylori, and sometimes surgery for complications.