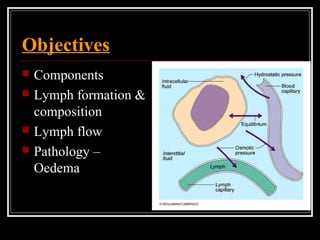
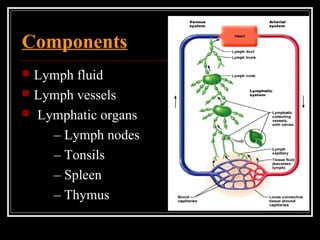
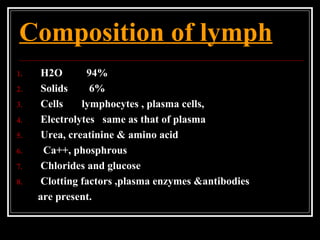
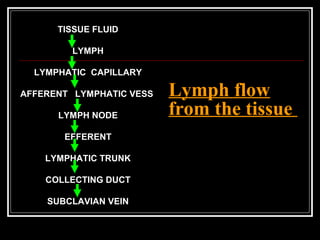
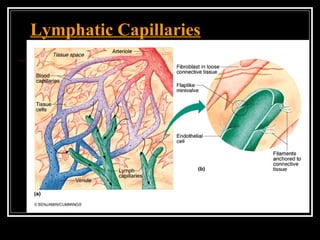
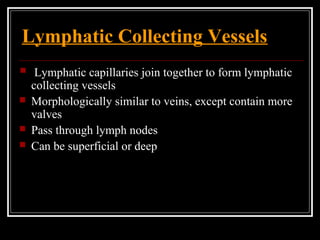
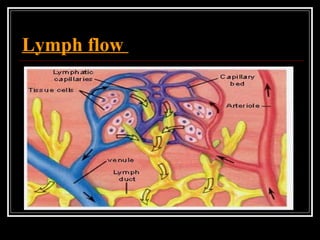
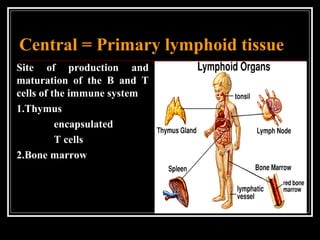
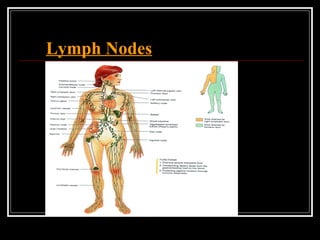
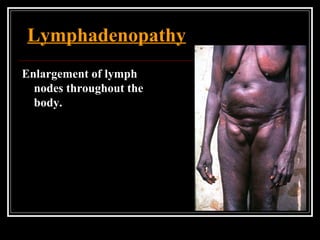
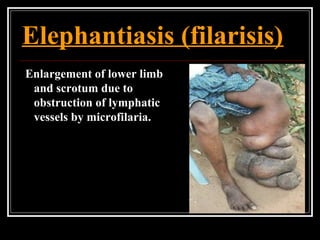
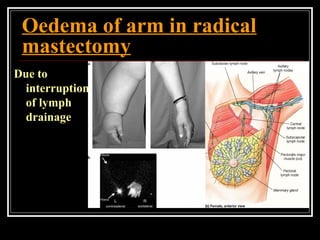
The lymphatic system consists of lymph fluid, lymph vessels, and lymphatic organs that include lymph nodes and tonsils. Lymph is formed from interstitial fluid and contains water, proteins, cells, and other components. It flows from lymph capillaries through collecting vessels and trunks into the thoracic duct or right lymphatic duct and returns to the bloodstream. The lymphatic system helps remove excess fluid from tissues, transports fat and proteins, and plays a role in immune defense and absorption of nutrients. Disruptions in lymph flow can cause edema or other pathologies like lymphadenopathy or elephantiasis.