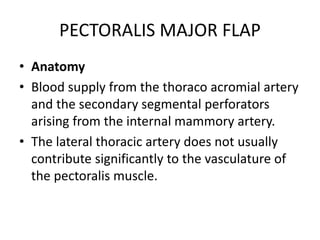
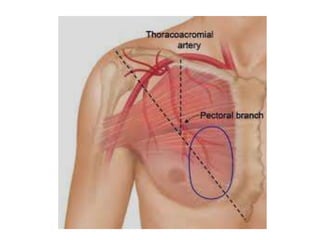
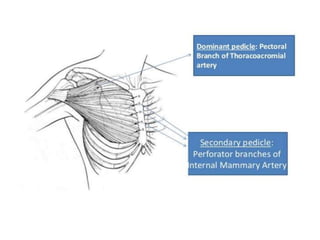
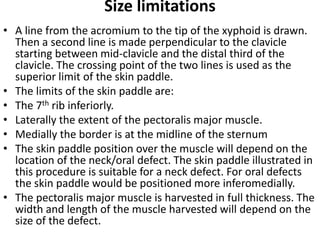
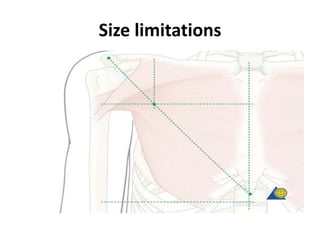
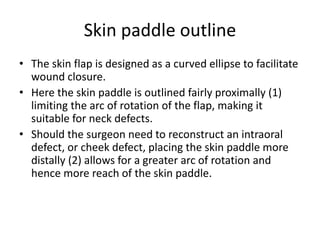
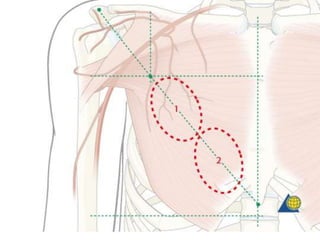
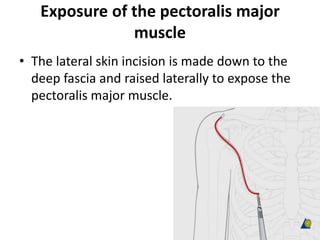
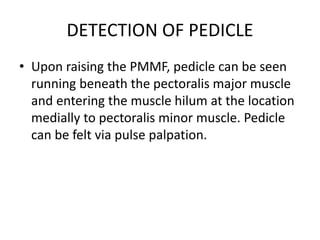
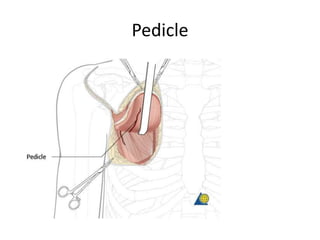
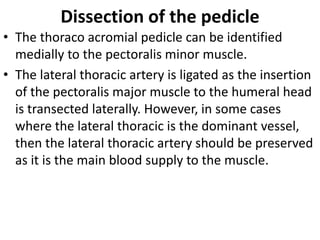
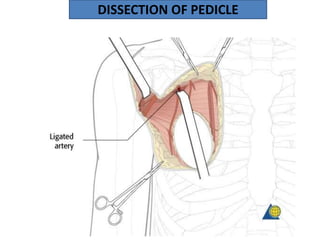
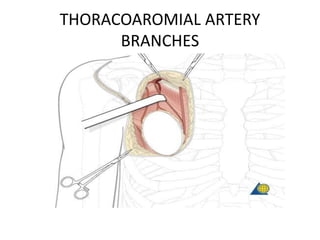
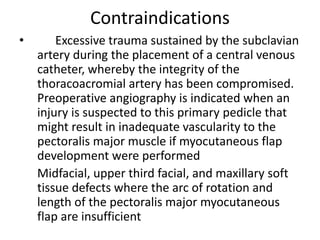
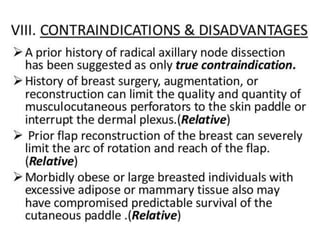
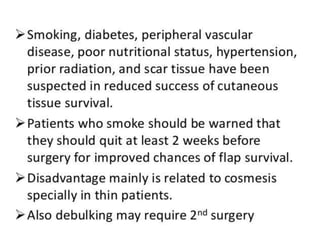
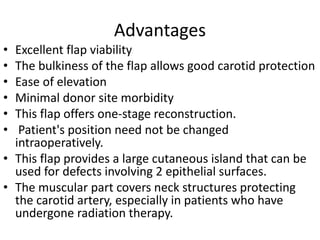
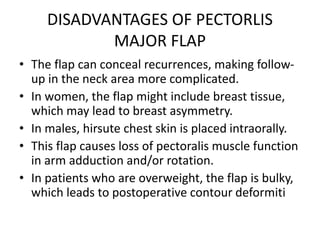
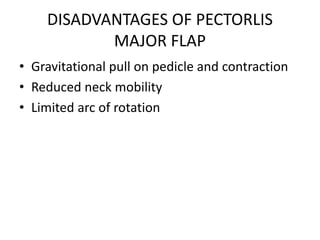
The pectoralis major flap uses the pectoralis major muscle and overlying skin to reconstruct head and neck defects. It has a reliable blood supply from the thoracoacromial artery. The muscle is raised from the chest wall and tunneled to the defect site. The skin paddle size and position can be adjusted depending on the location and size of the defect. Complications are rare but include infection, partial flap necrosis, and donor site issues. It provides a bulky well-vascularized tissue for reconstruction with minimal morbidity.