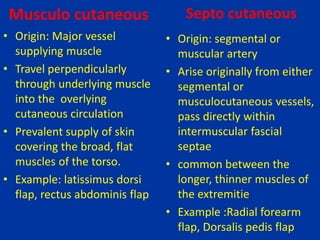
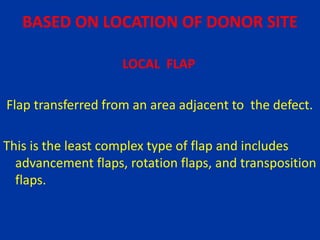
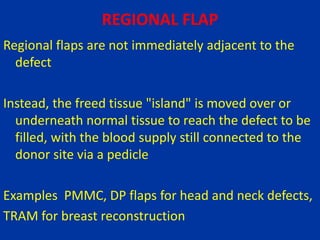
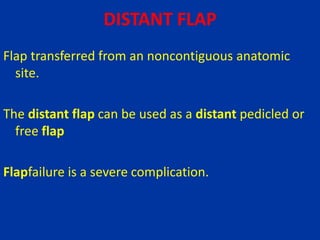
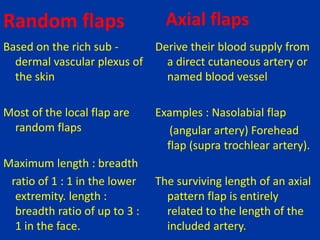
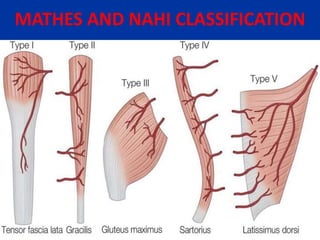
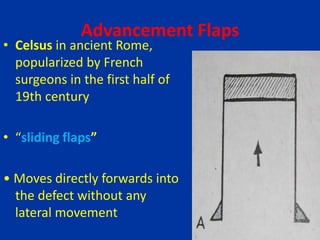
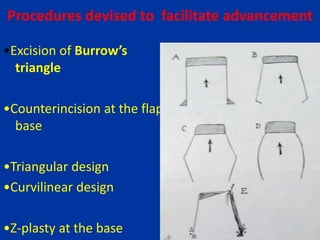
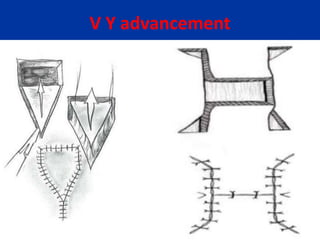
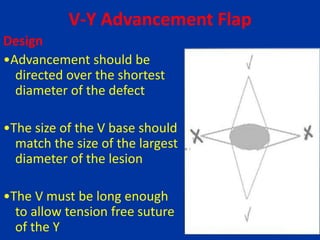
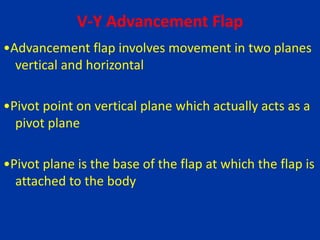
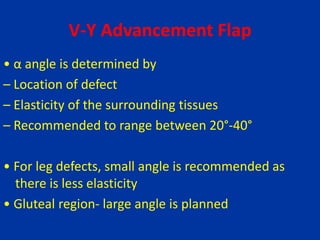
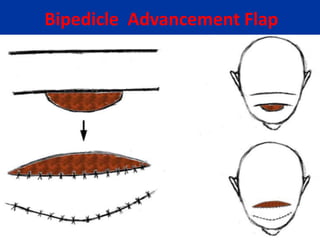
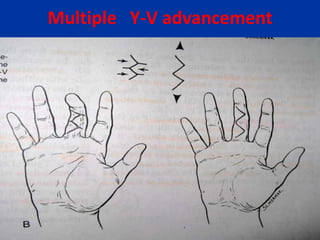
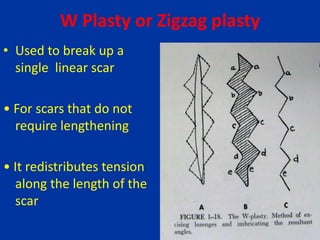
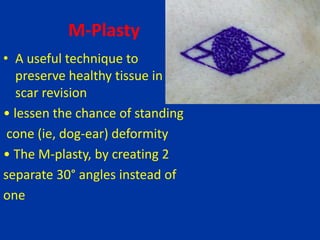
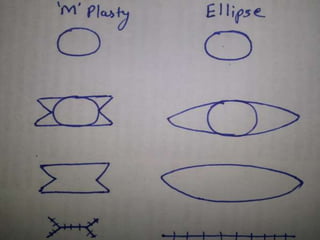
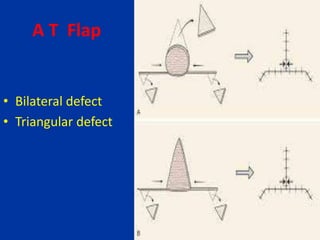
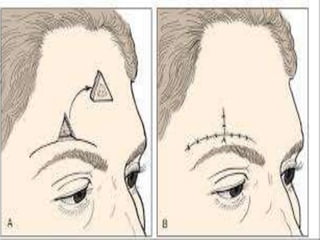
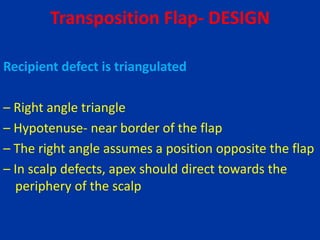
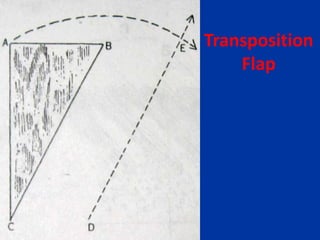
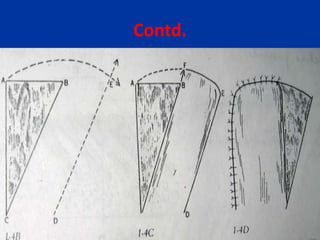
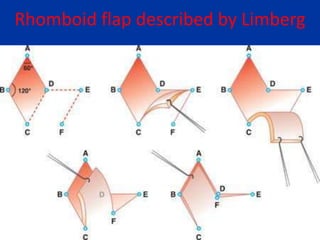
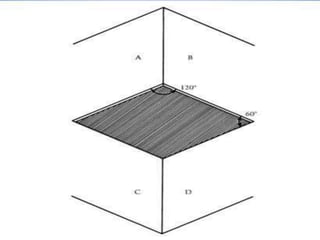
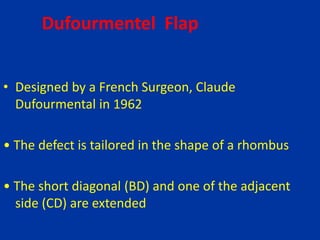
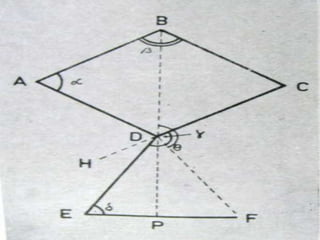
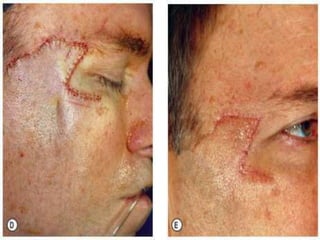
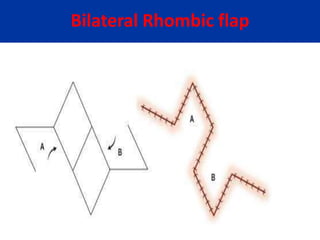
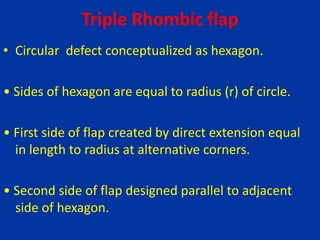
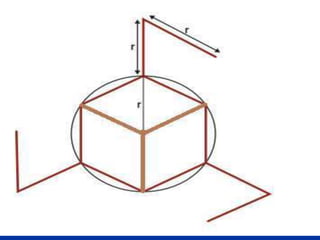
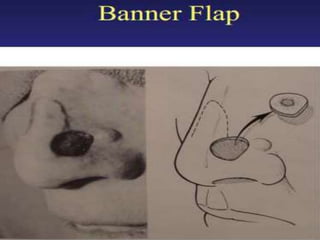
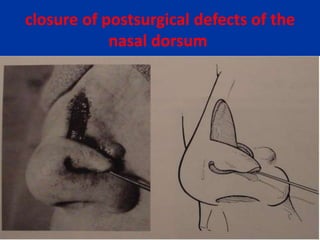
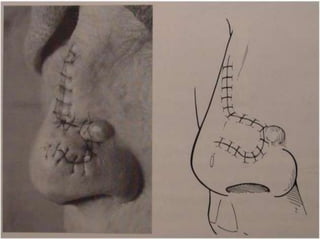
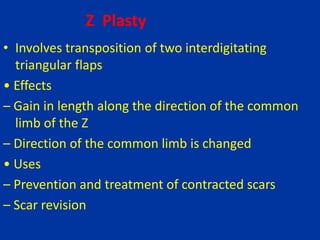
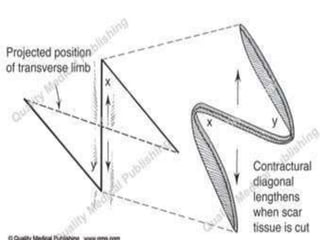
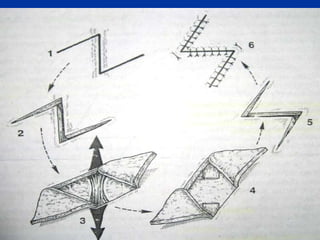
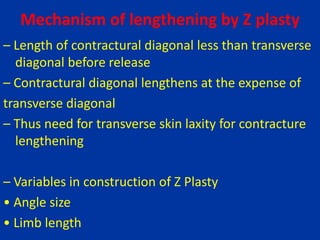
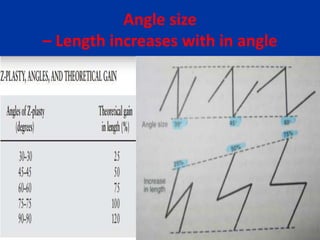
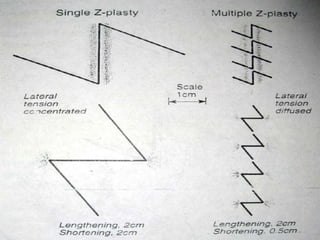
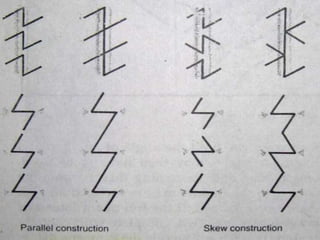
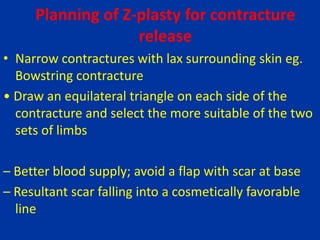
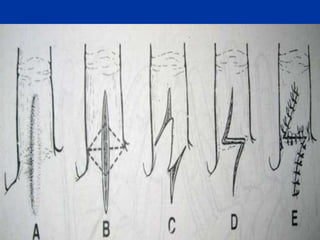
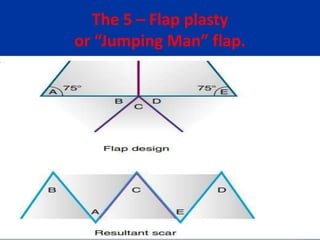
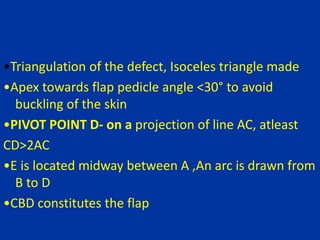
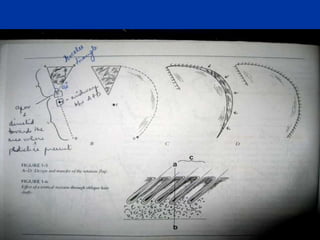
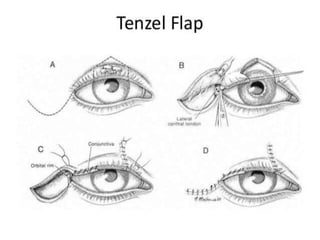
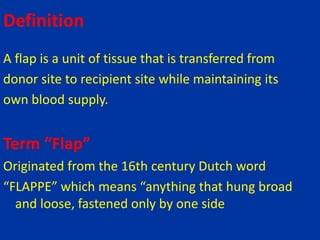
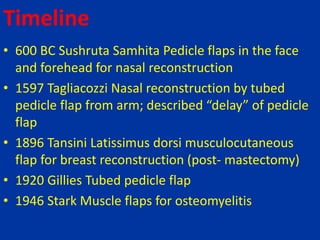
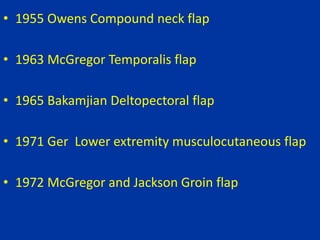
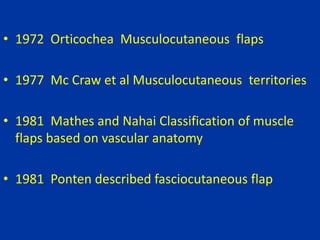
The document discusses various types of skin flaps used in reconstructive surgery. It defines a flap as a unit of tissue transferred from a donor site to a recipient site while maintaining its own blood supply. It then summarizes several types of local flaps used in reconstruction including advancement flaps, V-Y flaps, transposition flaps, and Z-plasties. The document also discusses regional flaps as well as modifications to flaps including flap delay and tissue expansion.

![Carl Manchot (1889 )
• Performed the first examination of the vascular
supply of the human integument.
• 40 cutaneous territories
• His work “Die Hautarterien des menschlichen
Körpers “ [The Cutaneous Arteries of the Human
Body] was initially published in German and later
translated to English by Milton.](https://image.slidesharecdn.com/skinflaps-190710171838/85/Skin-flaps-8-320.jpg)