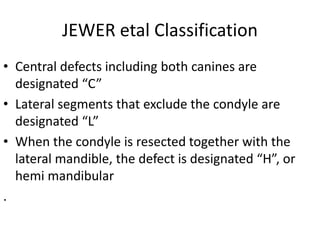
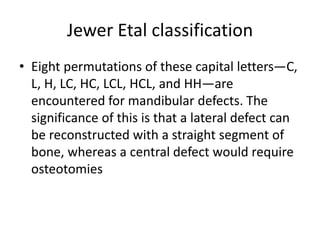
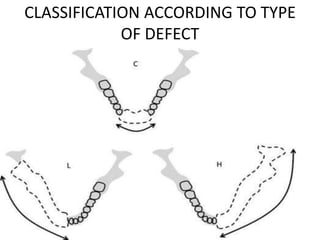
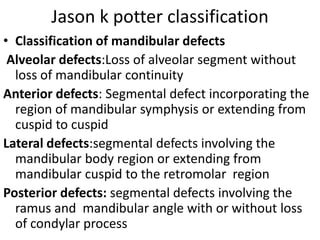
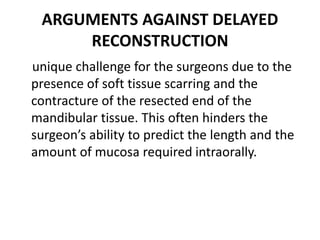
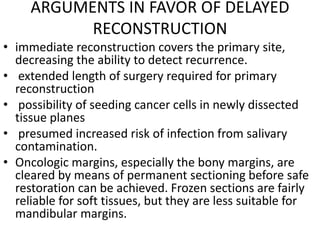
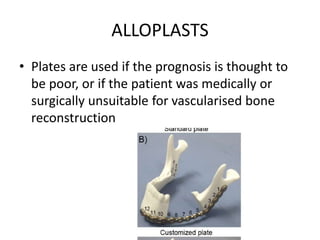
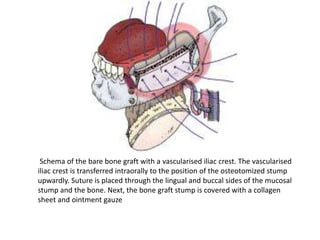
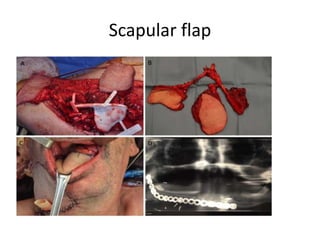
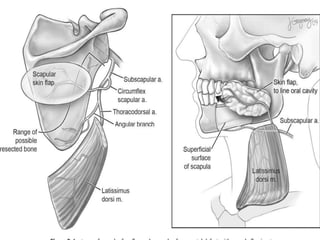
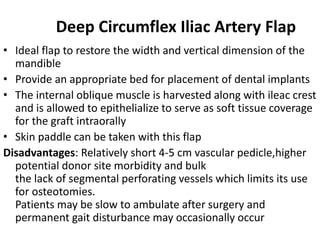
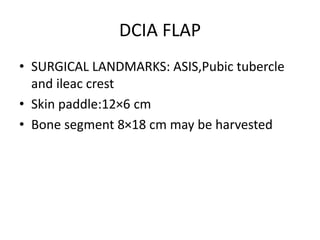
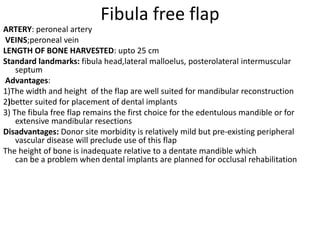
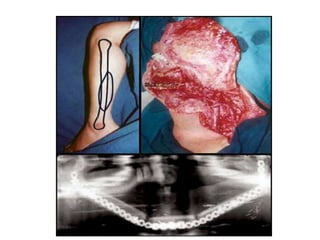
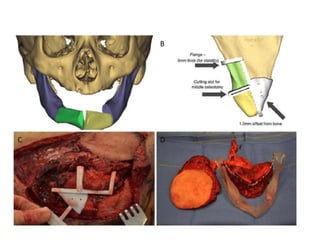
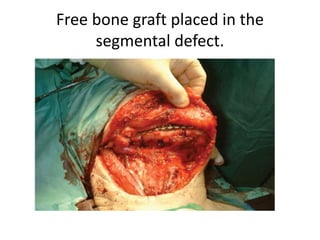
This document discusses various techniques for mandibular reconstruction after resection for tumors or injuries. The goals of reconstruction are to restore mandibular continuity, alveolar bone height, facial contours and function. Options include reconstruction plates, non-vascularized bone grafts for smaller defects, and microvascular free flaps for larger defects or those needing implant placement. The fibula and scapula flaps are commonly used, providing adequate bone stock. Proper classification of defect type and immediate versus delayed reconstruction must be considered to achieve optimal aesthetic and functional outcomes.