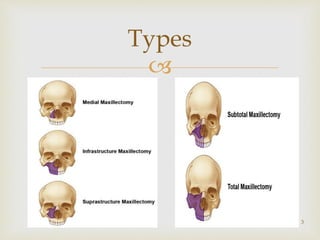
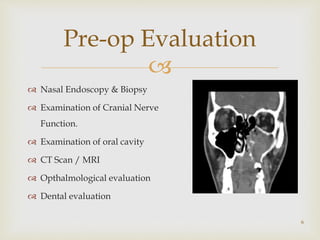
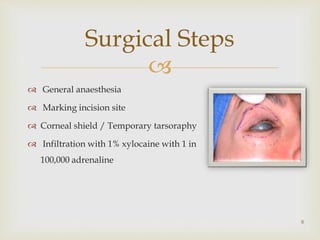
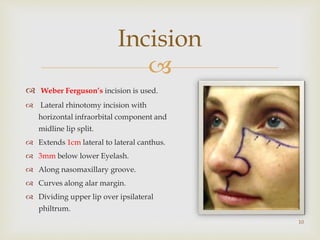
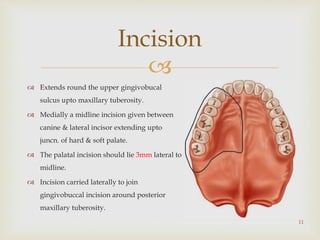
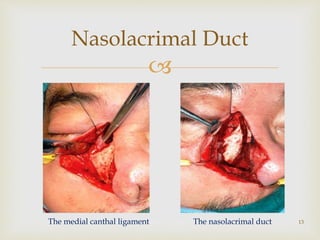
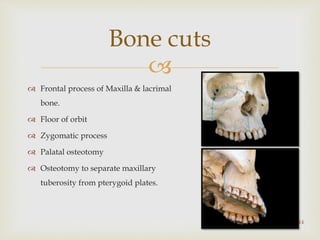
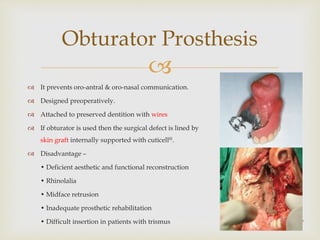
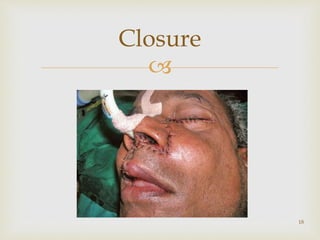
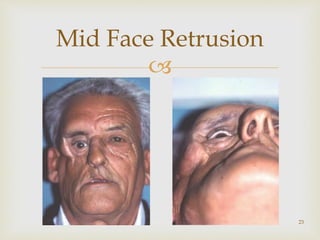
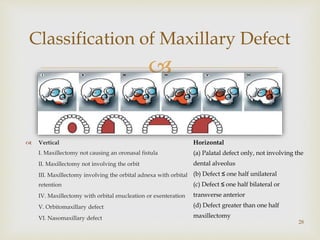
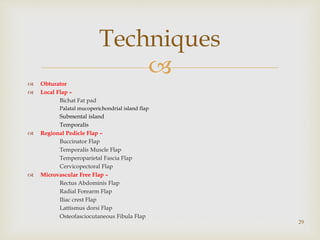
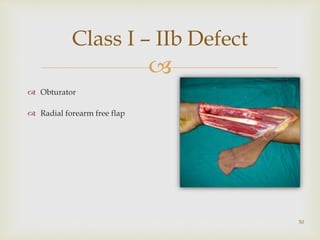
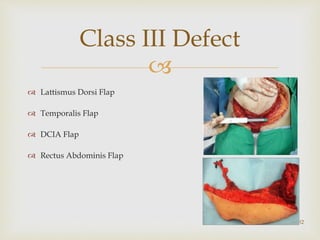
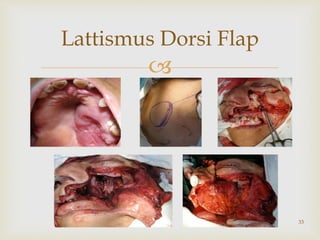
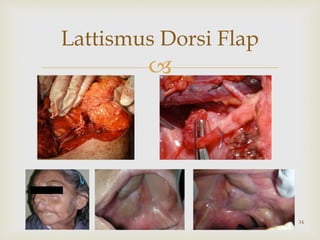
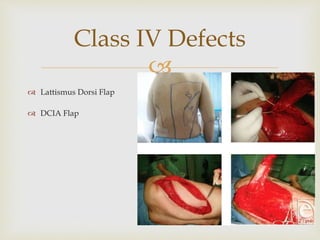
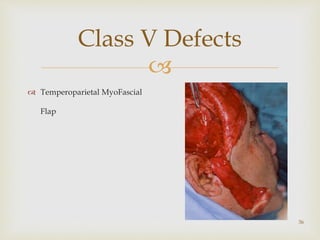
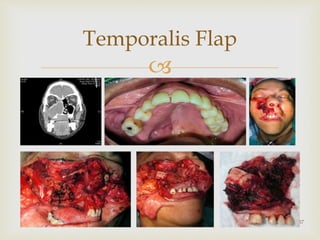
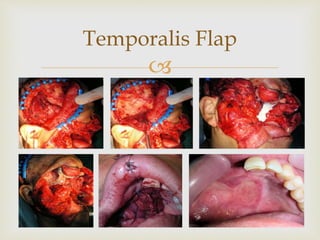
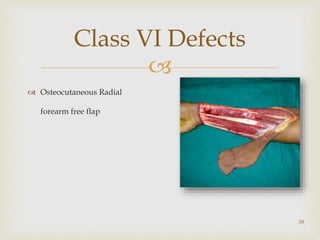
The document outlines the historical development and surgical techniques for maxillectomy, detailing various approaches and methods for addressing maxillary tumors. It includes indications, contraindications, pre-operative evaluations, surgical steps, complications, and reconstruction techniques for managing maxillary defects. Post-operative care and common complications such as bleeding, mid-face retrusion, and numbness are also highlighted.