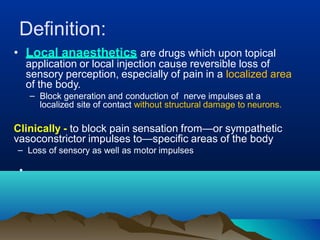
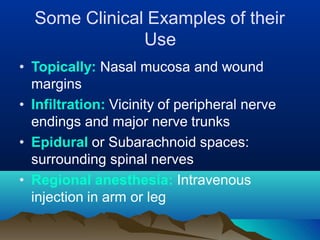
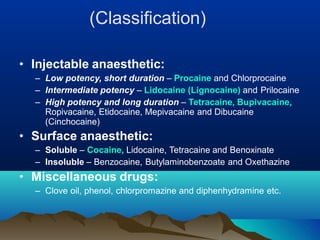
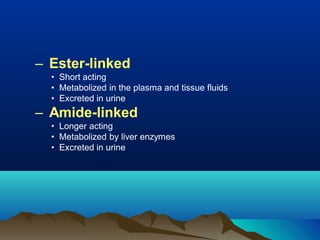
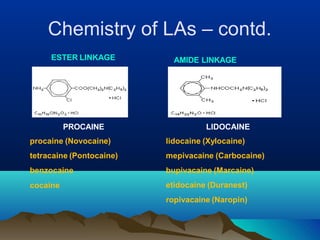
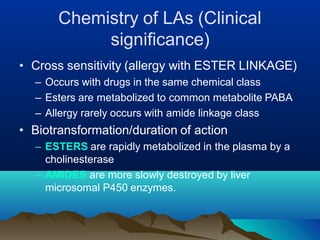
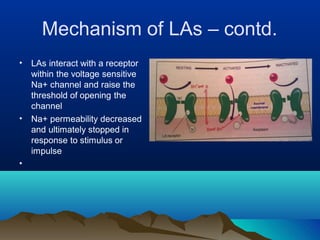
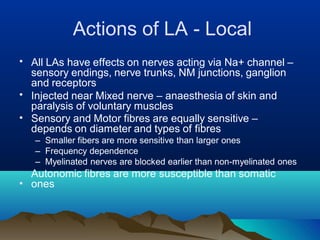
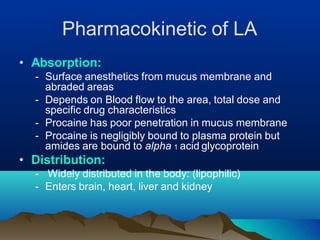
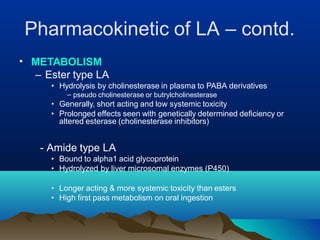
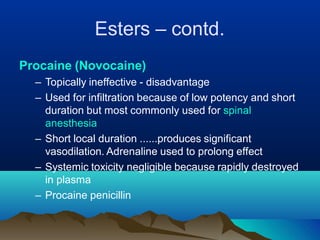
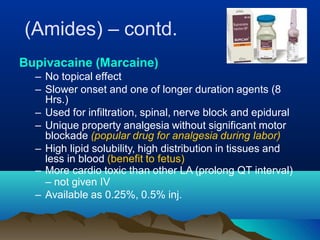
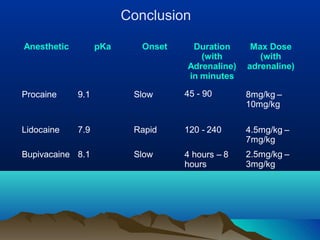
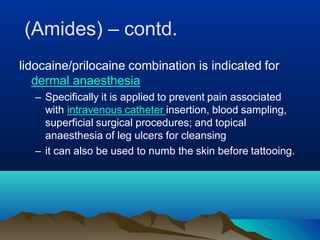
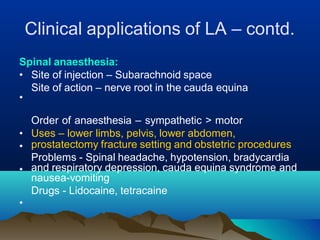
Local anesthetics are drugs that reversibly block nerve impulses and sensation of pain in localized areas. They work by inhibiting sodium influx through voltage-gated sodium channels in neurons. Common examples include lidocaine, bupivacaine, and tetracaine. Esters like procaine have a short duration due to rapid metabolism, while amides like lidocaine and bupivacaine have a longer duration due to liver metabolism. Local anesthetics are used topically, for infiltration, in spinal or epidural spaces, and for regional nerve blocks to provide anesthesia for various procedures.