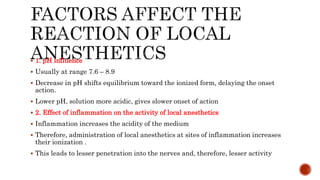
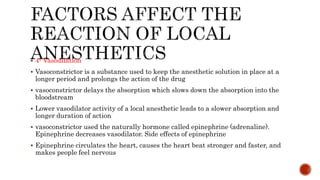
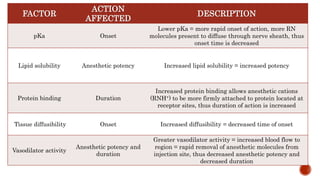
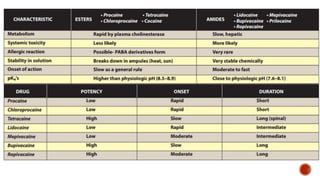
Local anesthetics work by reversibly blocking nerve conduction. They alter the nerve membrane potential and decrease nerve firing and depolarization rates. Local anesthetics are classified as esters, amides, or ketones. After injection, esters are quickly broken down while amides have longer half-lives and their toxicity is more likely if liver function is impaired. The onset and duration of local anesthetics are affected by tissue pH, concentration, and lipid solubility, with pH being most important. Adding epinephrine decreases systemic toxicity and increases duration by reducing absorption. Local anesthetic toxicity can cause CNS stimulation or depression as well as cardiovascular effects.