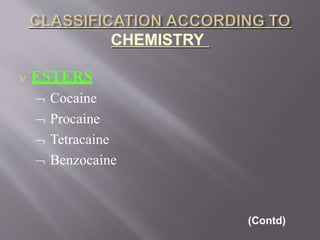
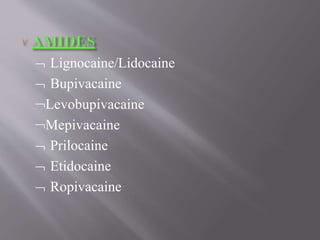
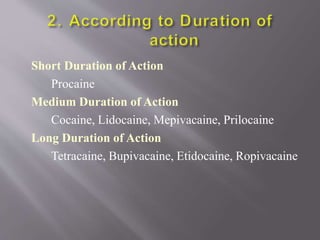
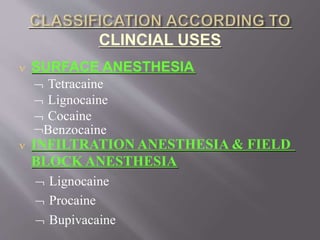
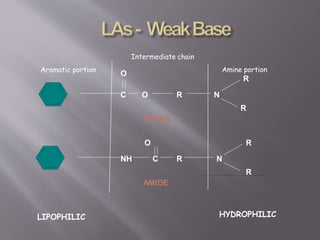
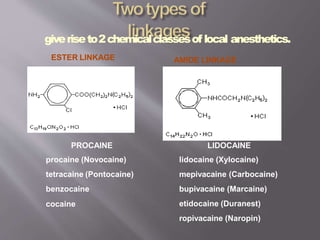
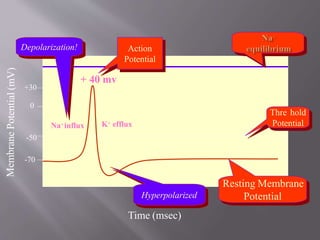
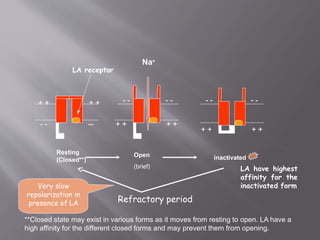
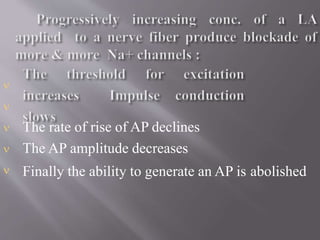
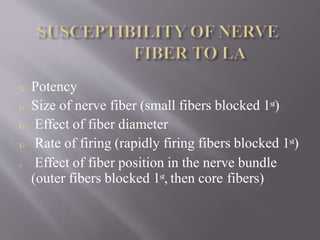
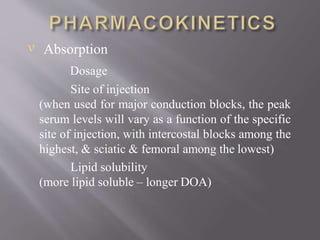
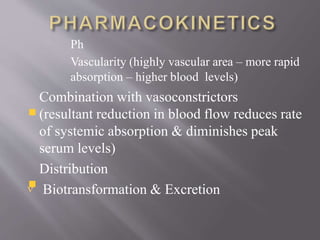
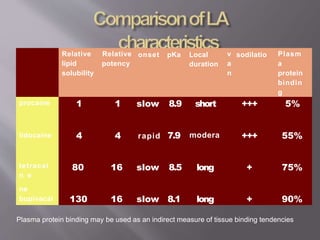
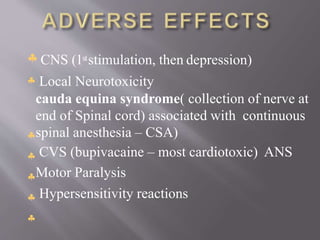
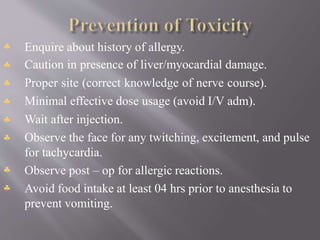
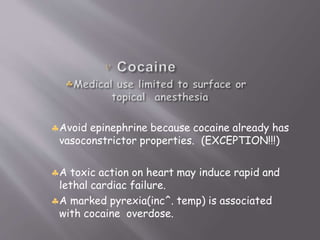
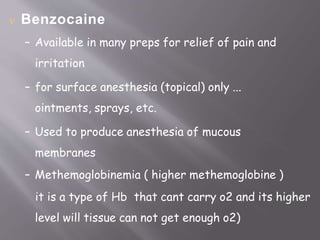
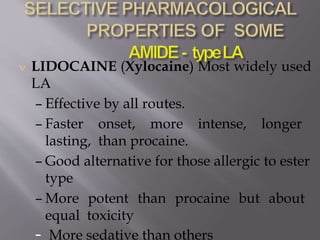
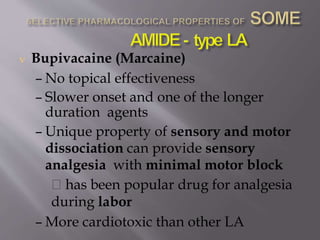
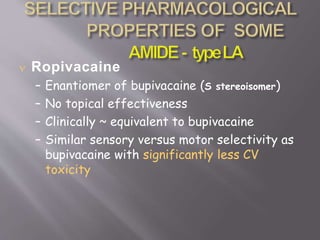
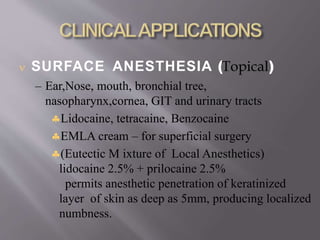
The document discusses local anesthetics, emphasizing their ability to produce reversible loss of sensation in targeted areas. It covers the classes of anesthetics, their mechanisms of action, clinical uses, and key examples like lidocaine and bupivacaine, along with their pharmacokinetics and side effects. Additionally, it details various administration methods, including infiltration and spinal anesthesia, providing insights into their applications and precautions.