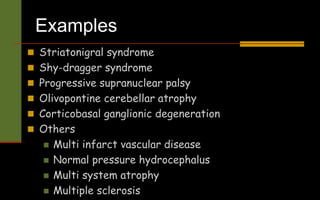
The document discusses extrapyramidal disorders and basal ganglia disorders. It provides information on:
- The extrapyramidal system and basal ganglia, which are involved in motor control and other functions.
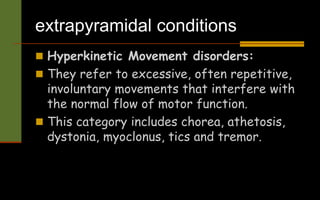
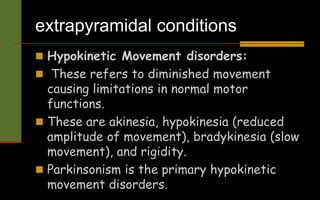
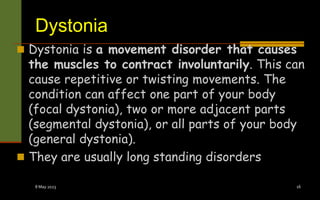
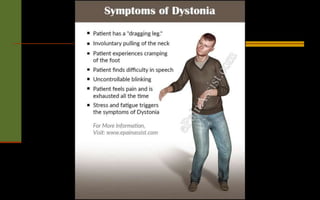
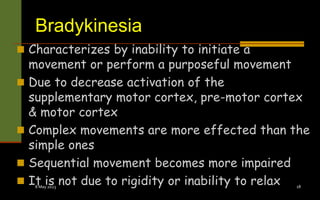
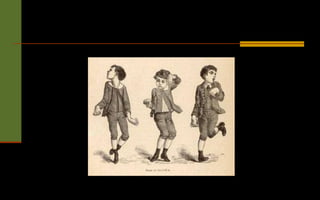
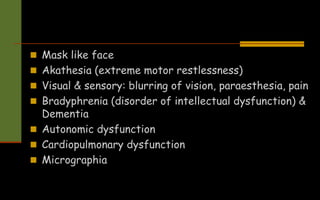
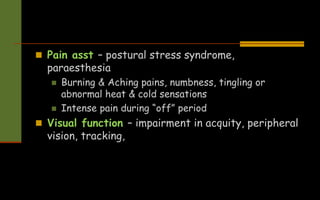
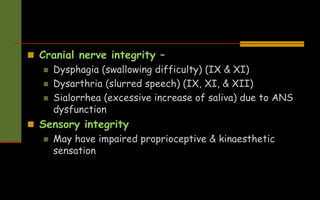
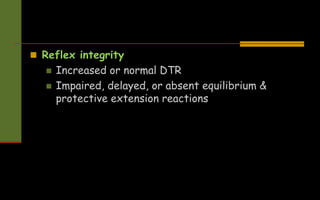
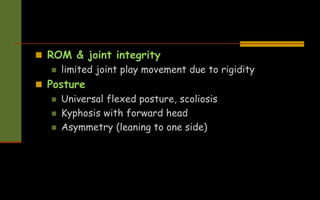
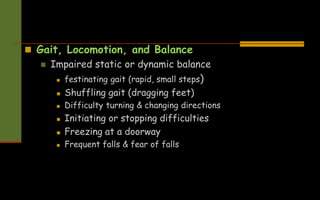
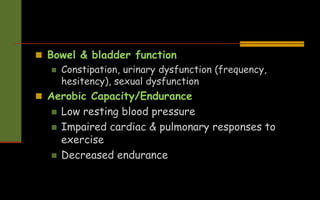
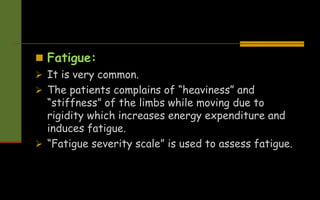
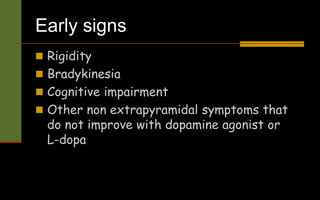
- Movement disorders are divided into hyperkinetic disorders involving excessive movements (chorea, dystonia) and hypokinetic disorders with diminished movement (akinesia, bradykinesia, rigidity).
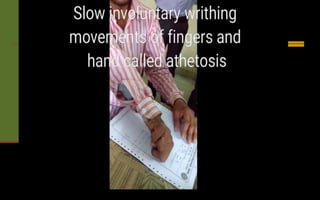
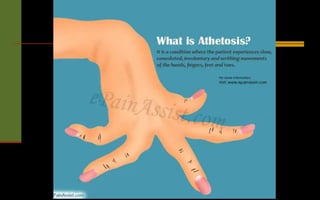
- Lesions in the basal ganglia can cause specific movement disorders like athetosis, dystonia, bradykinesia, rigidity, tremor, and others.
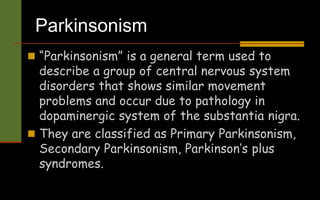
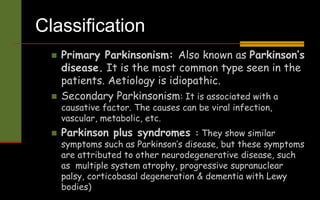
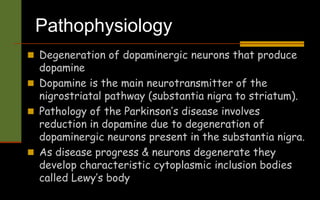
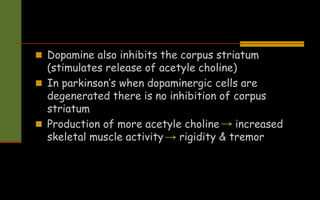
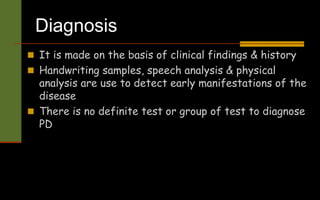
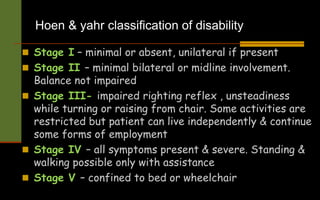
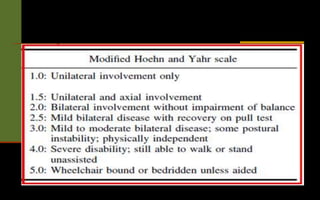
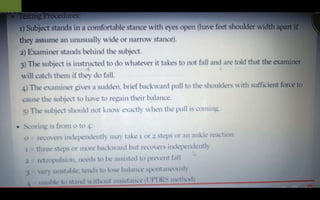
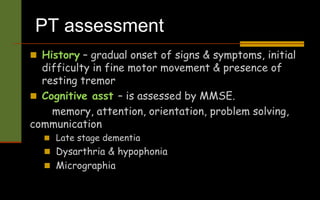
- Parkinson's disease is discussed as a primary hypokinetic disorder caused by degeneration of dopaminergic