The document discusses liver function tests and bilirubin metabolism. It provides details on:
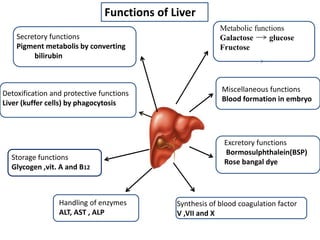
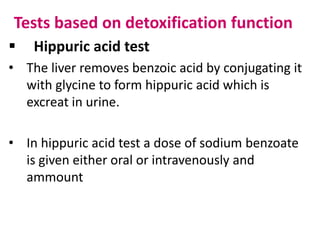
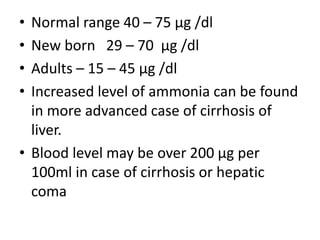
1. The metabolic, secretory, detoxification and other functions of the liver.
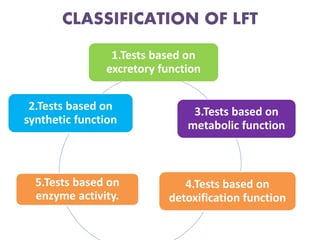
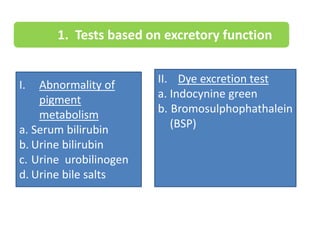
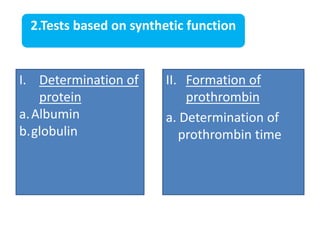
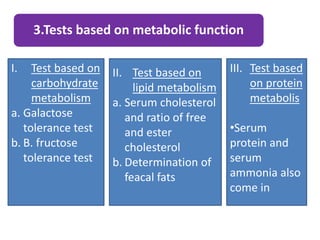
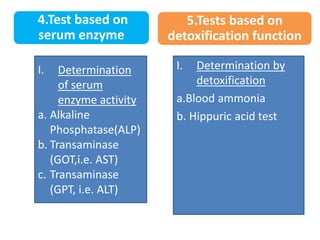
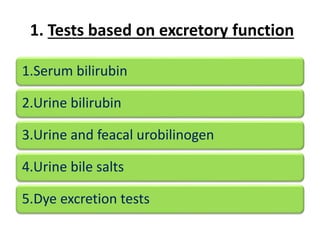
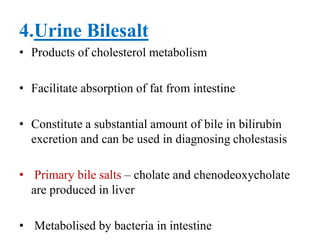
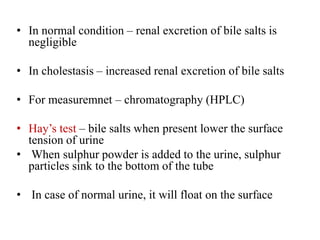
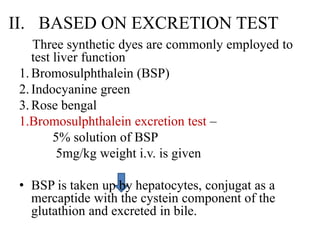
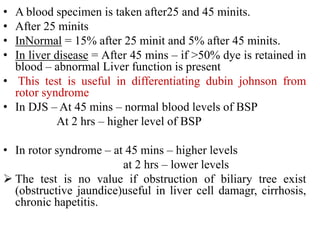
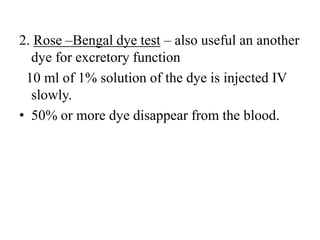
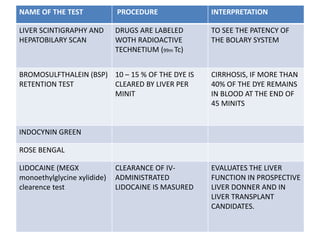
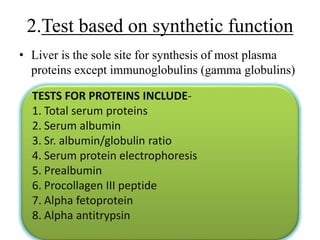
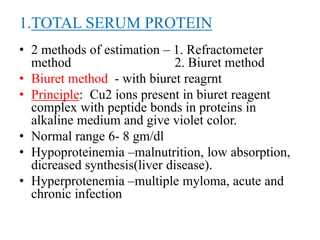
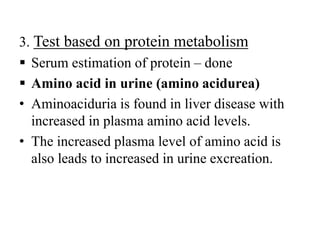
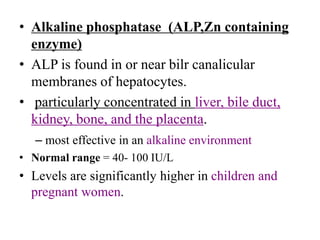
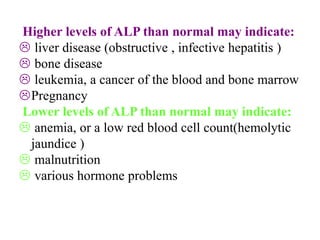
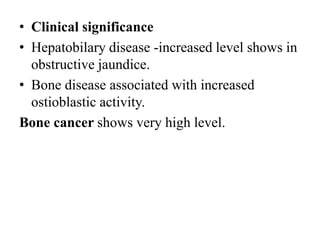
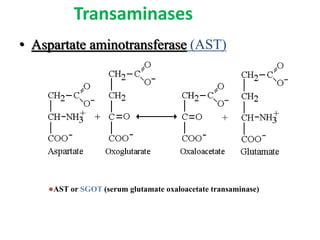
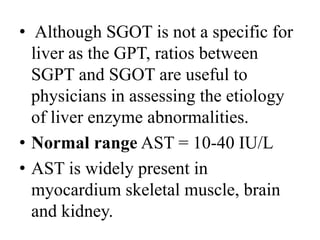
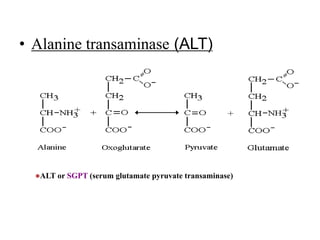
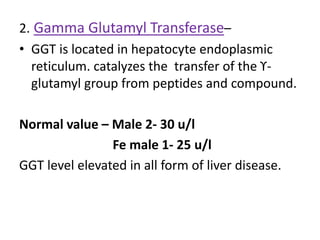
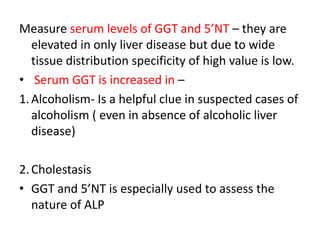
2. Classification of liver function tests including those based on excretory, synthetic, metabolic, detoxification and enzyme activity functions.
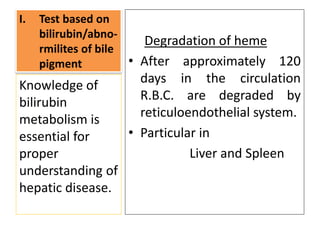
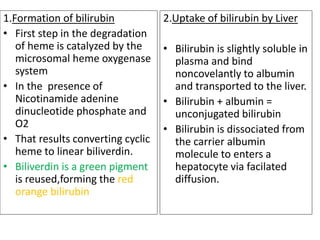
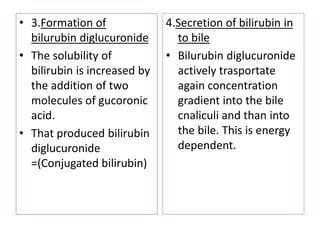
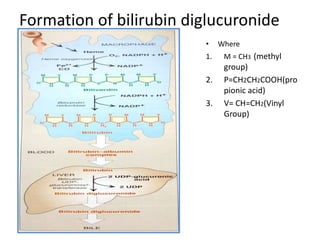
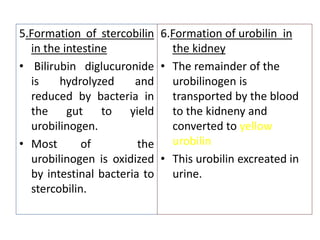
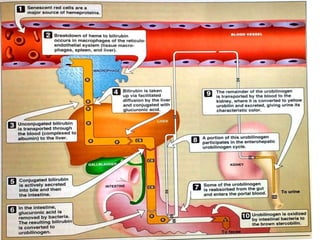
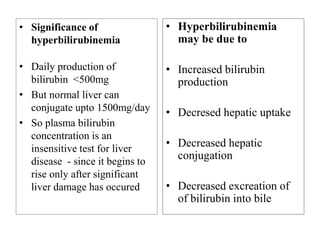
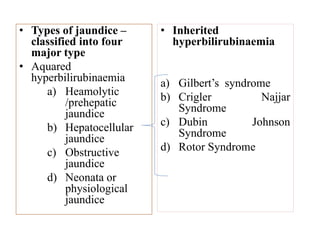
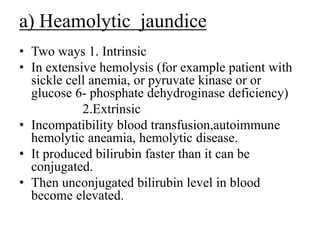
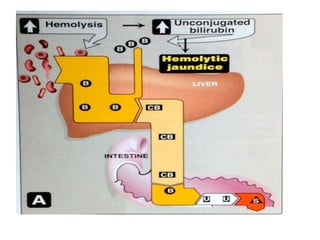
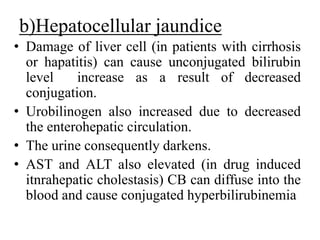
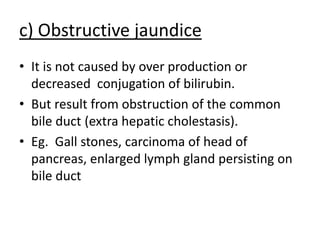
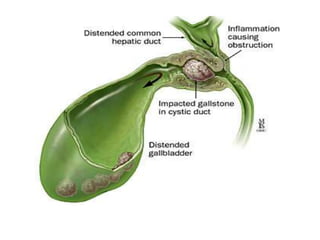
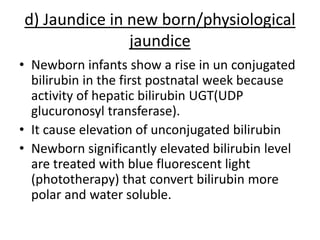
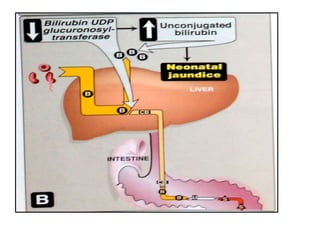
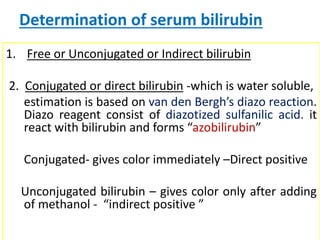
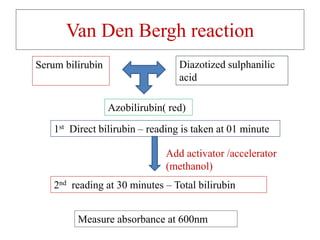
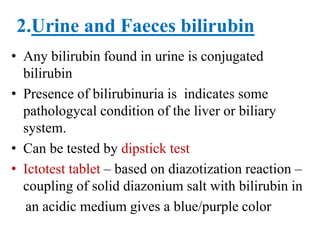
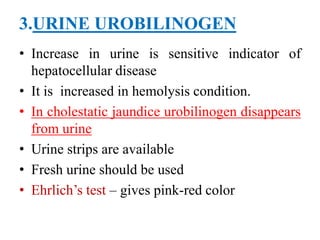
3. Bilirubin metabolism including formation, uptake, conjugation and excretion from the liver and intestines.