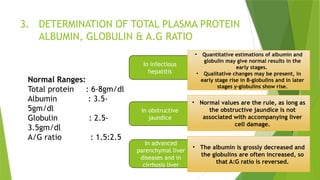
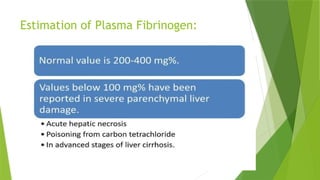
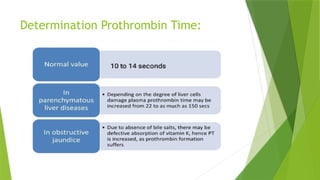
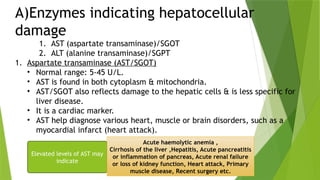
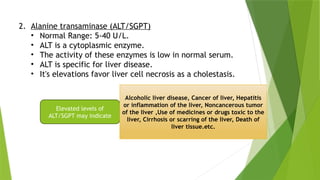
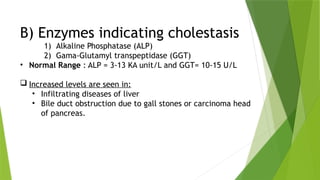
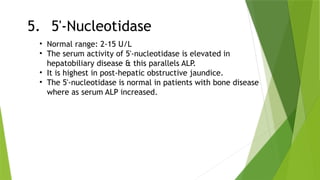
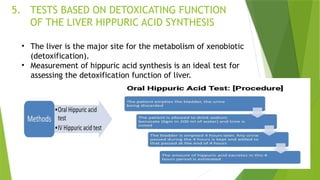
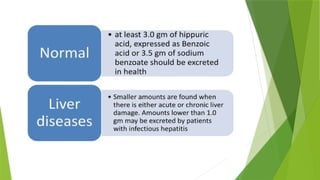
Liver function tests (LFT) assess the liver's metabolic, excretory, synthetic, detoxifying, storage, and protective functions. They help detect liver diseases, differentiate types, and monitor treatment response through various tests like serum bilirubin, enzyme levels, and protein measurements. The document outlines essential liver functions and the relevance of specific tests in diagnosing conditions such as jaundice and liver damage.