This document provides information on left ventricular aneurysms including:
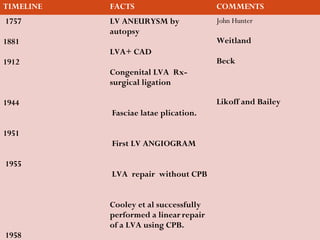
- A timeline of important discoveries and advances in LV aneurysm research and treatment from 1757 to 1958.
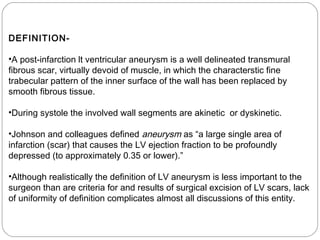
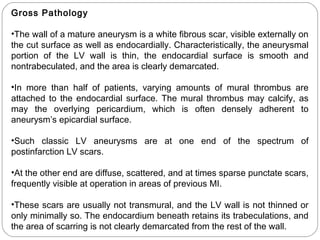
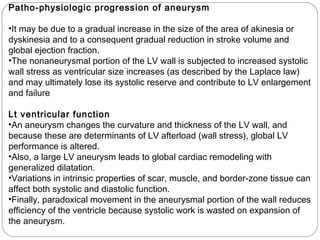
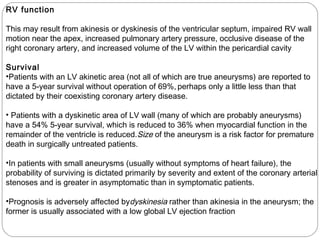
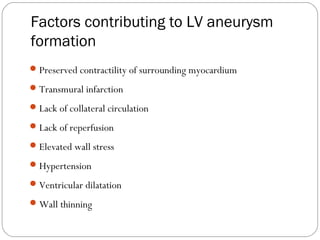
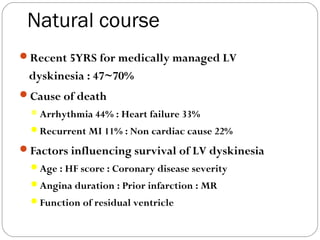
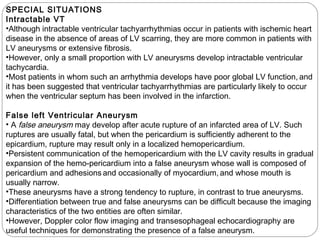
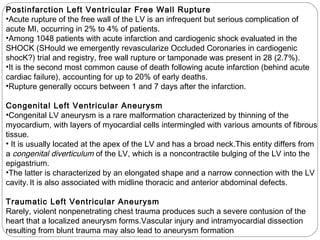
- Definitions, gross pathology, microscopic pathology, location, and natural history of LV aneurysms.
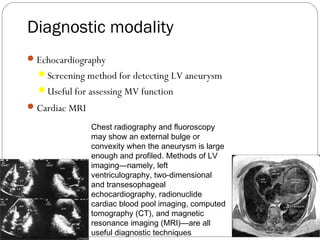
- Clinical features and diagnostic criteria for LV aneurysms.
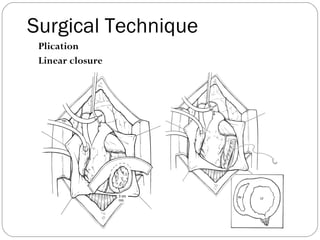
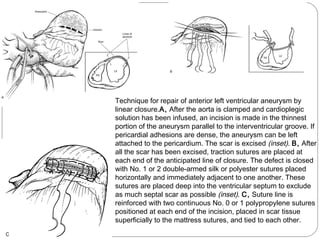
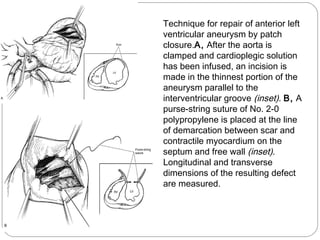
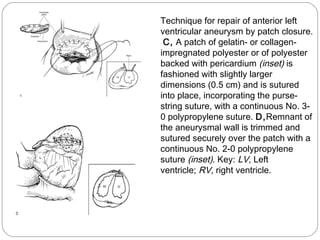
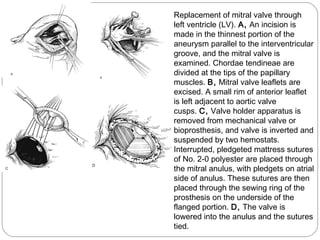
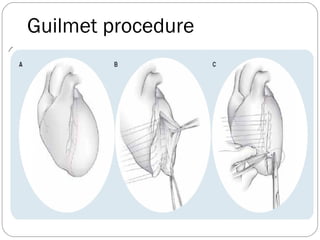
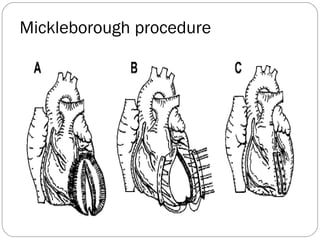
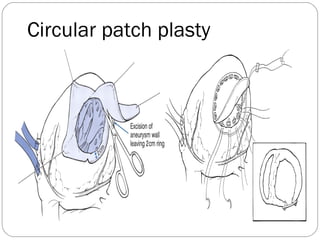
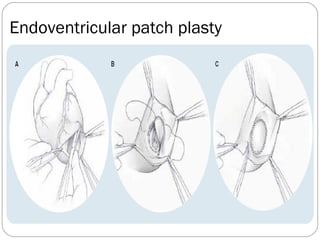
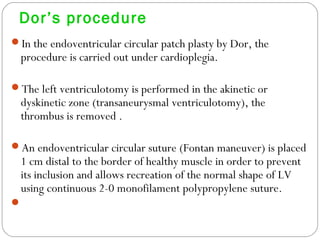
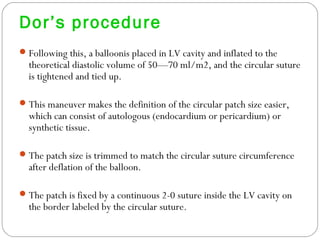
- Surgical techniques for repairing LV aneurysms including plication, linear closure, patch closure, and endoventricular circular patch repair.