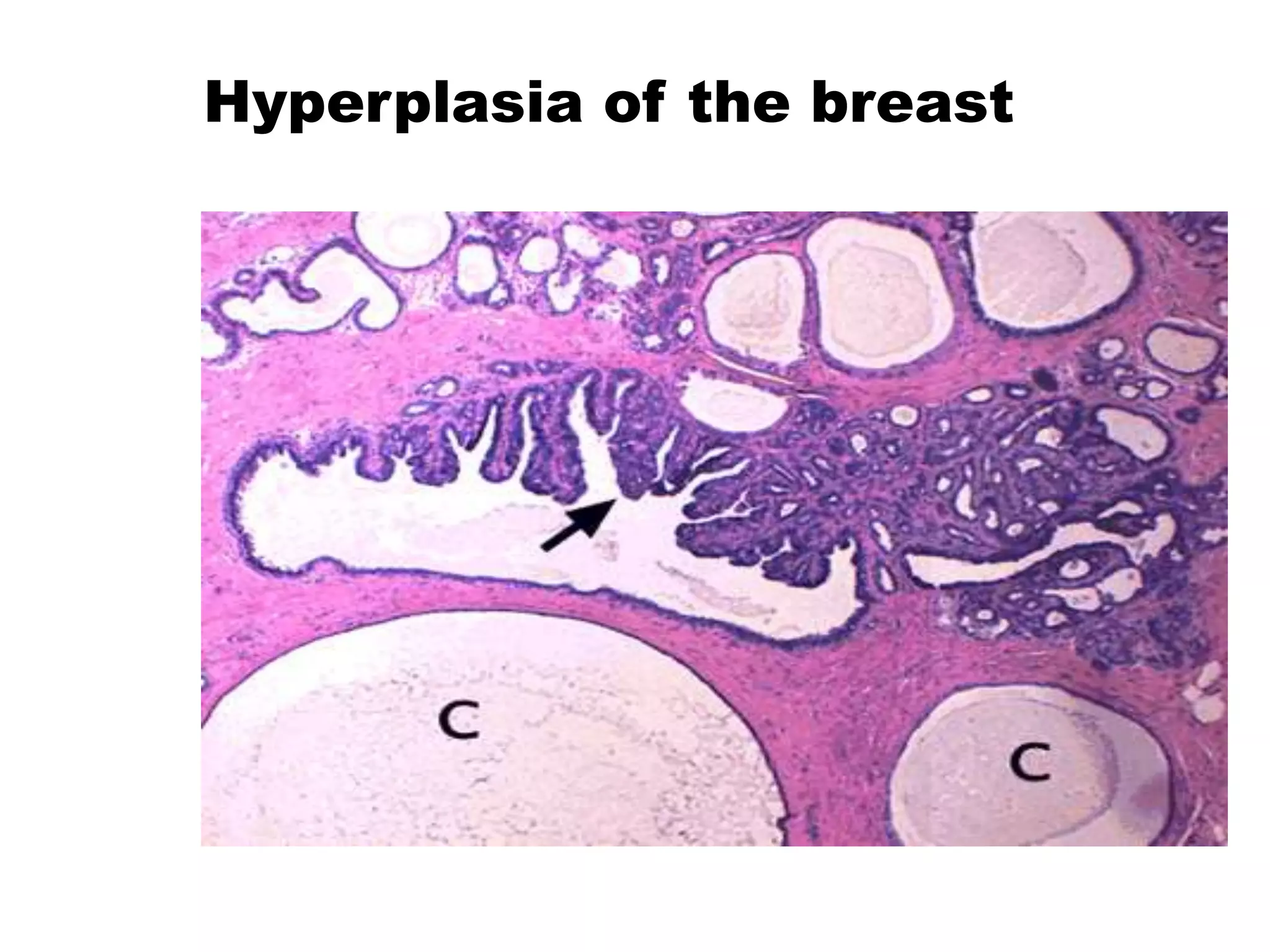
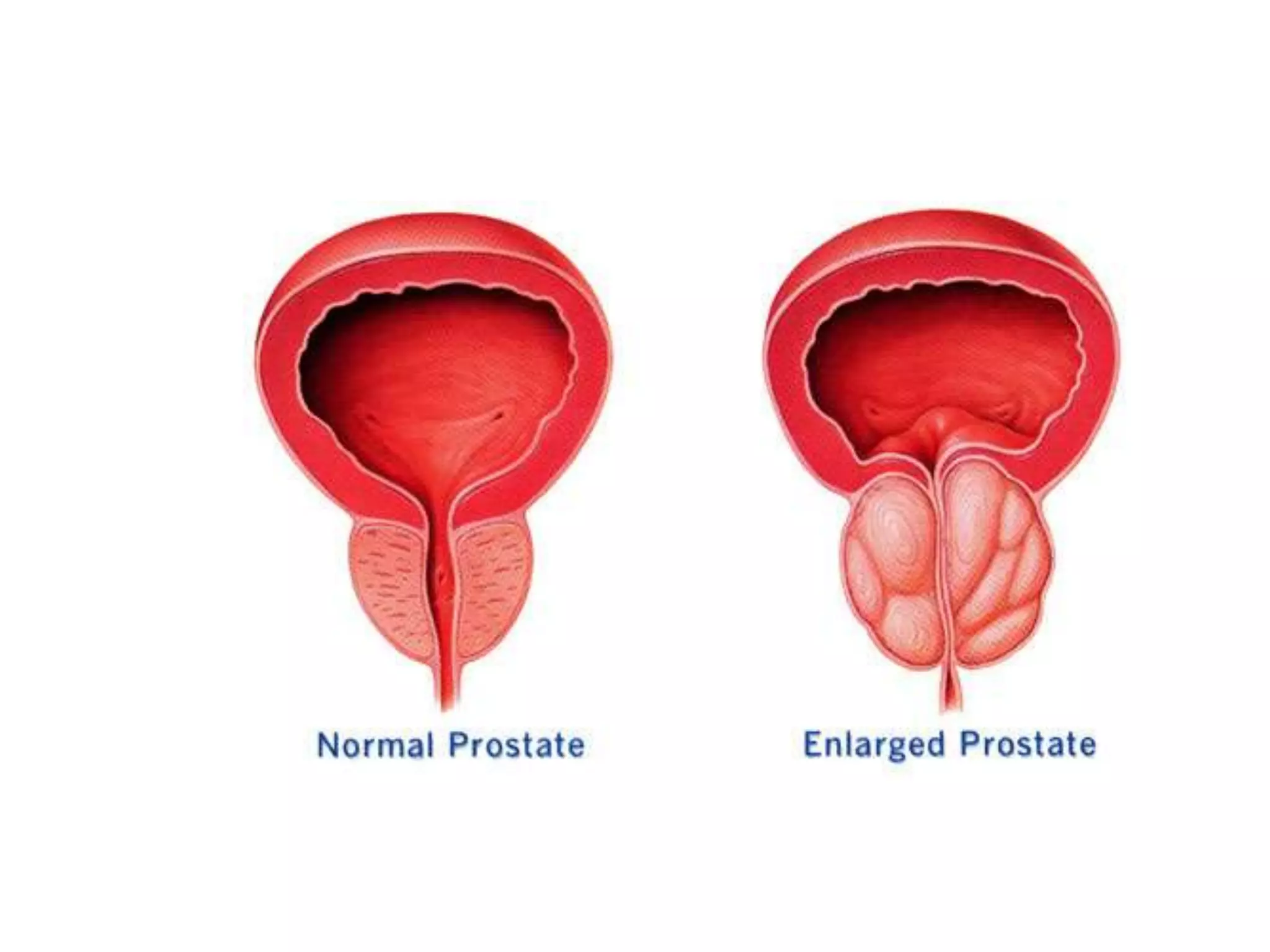
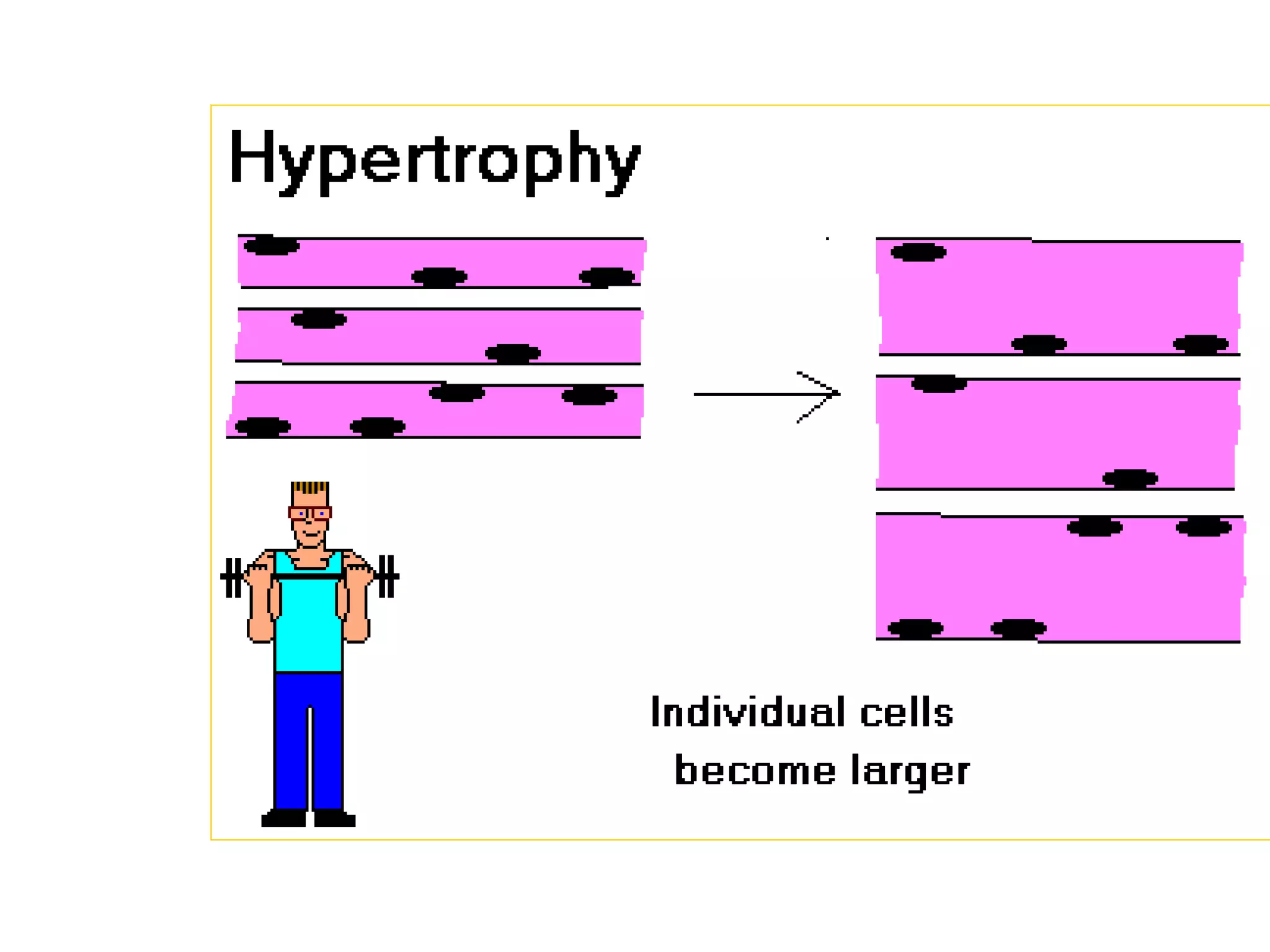
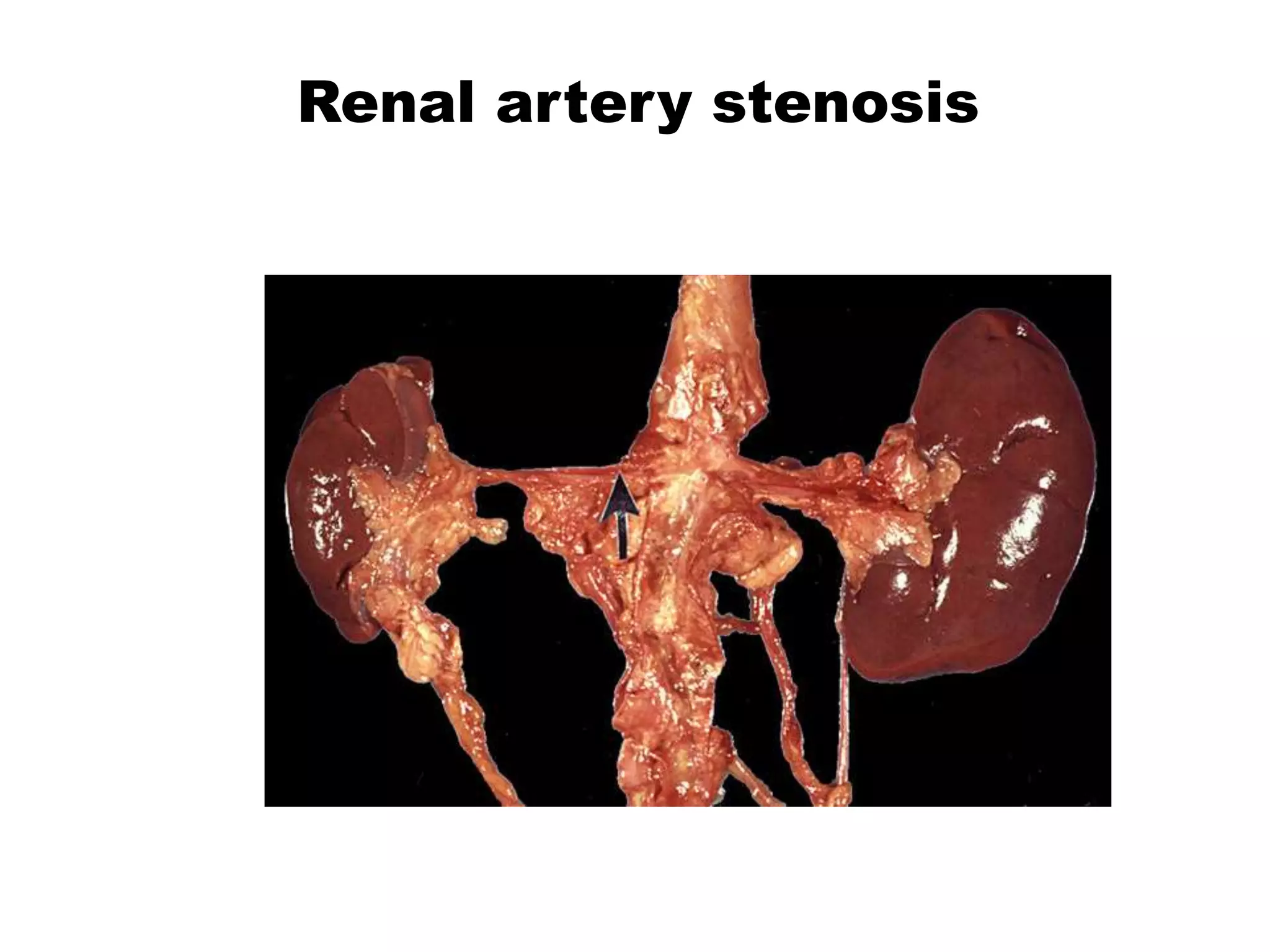
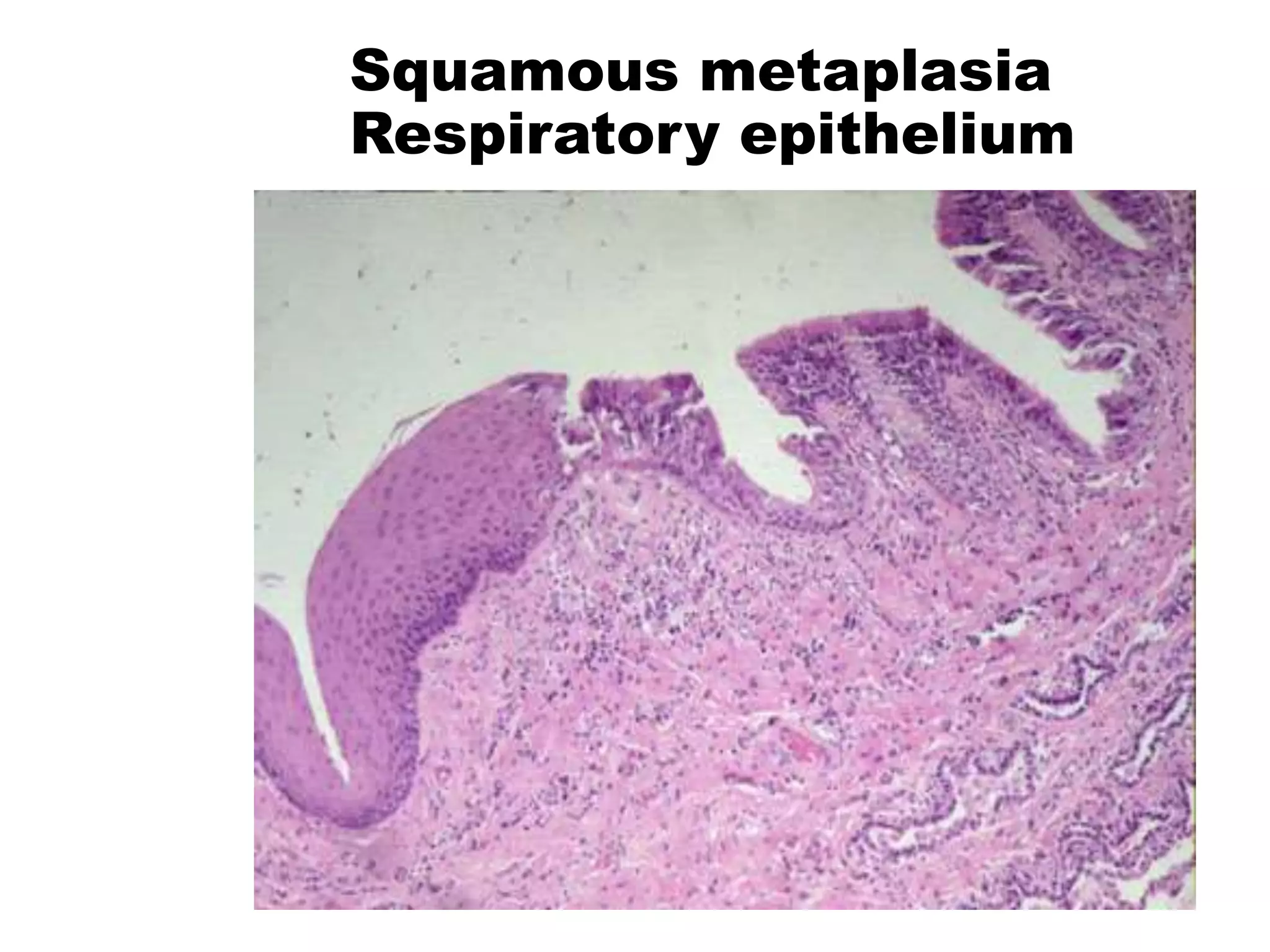
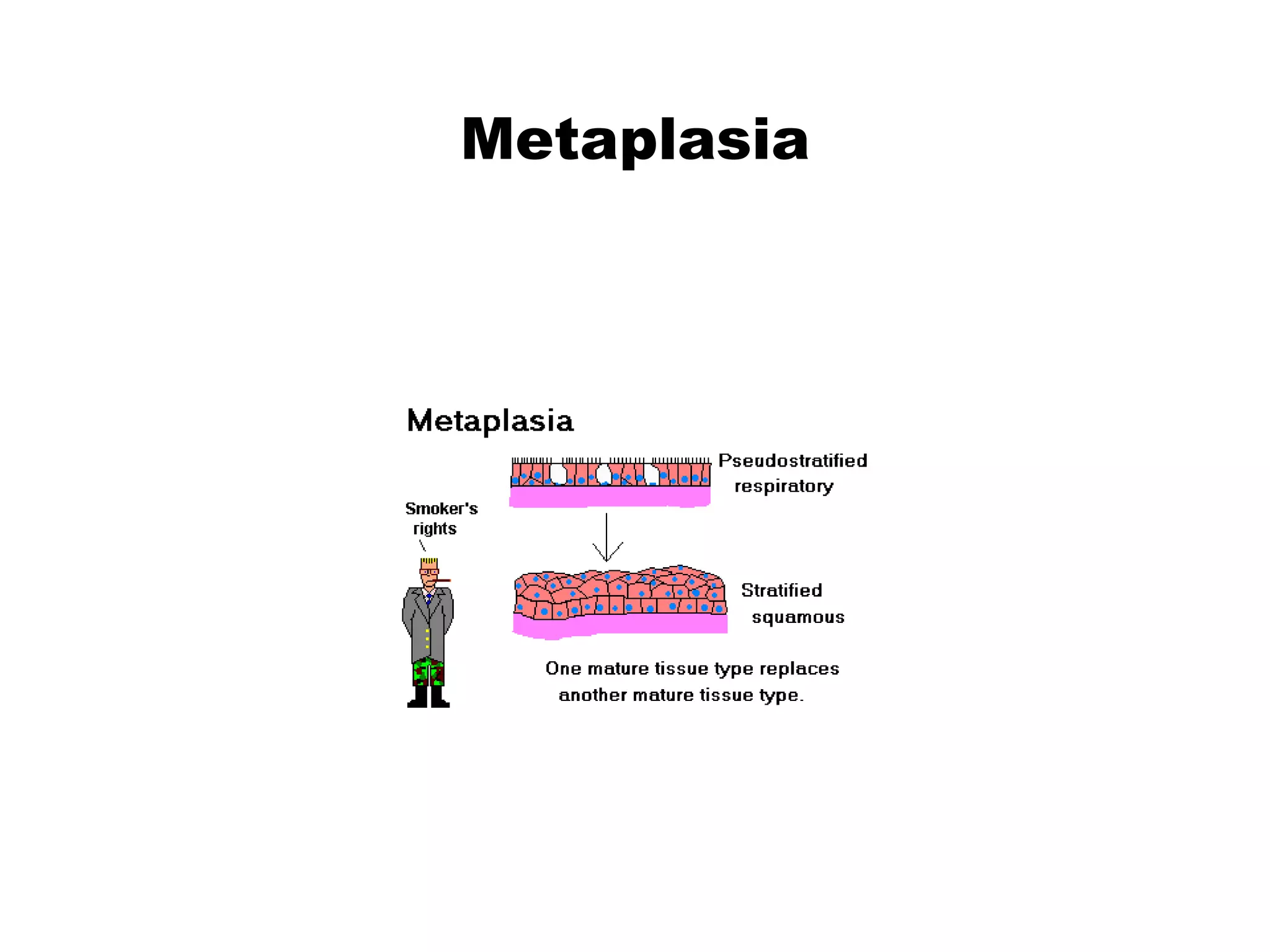
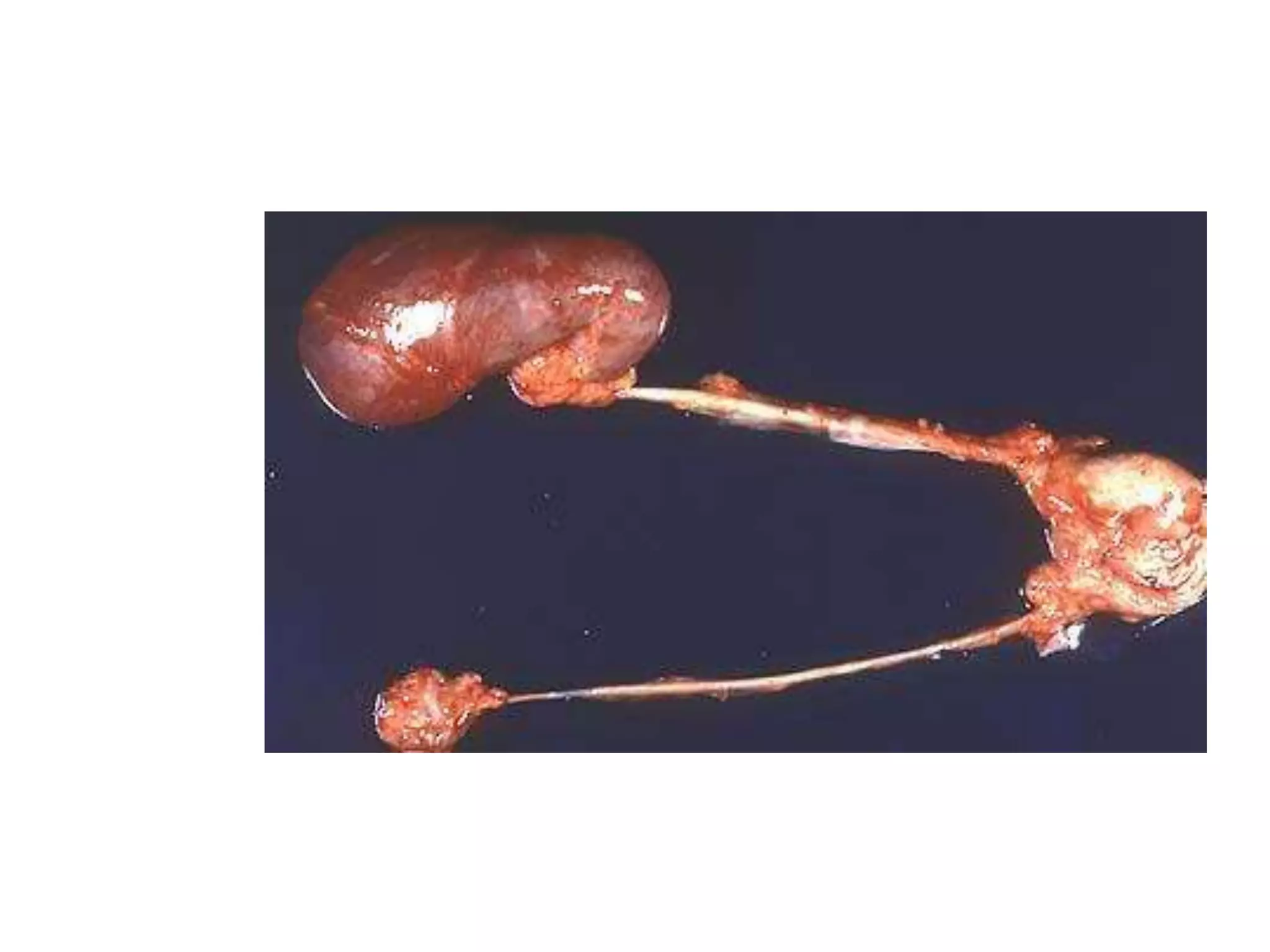
Cellular adaptations like hyperplasia, hypertrophy, atrophy, and metaplasia allow cells to respond to physiological and pathological stresses in order to preserve viability. Hyperplasia is an increase in cell number, hypertrophy is an increase in cell size, atrophy is a reduction in cell and organ size, and metaplasia is the replacement of one adult cell type with another. These adaptations can be physiological responses to normal stimuli or pathological responses attempting to cope with abnormal stimuli.