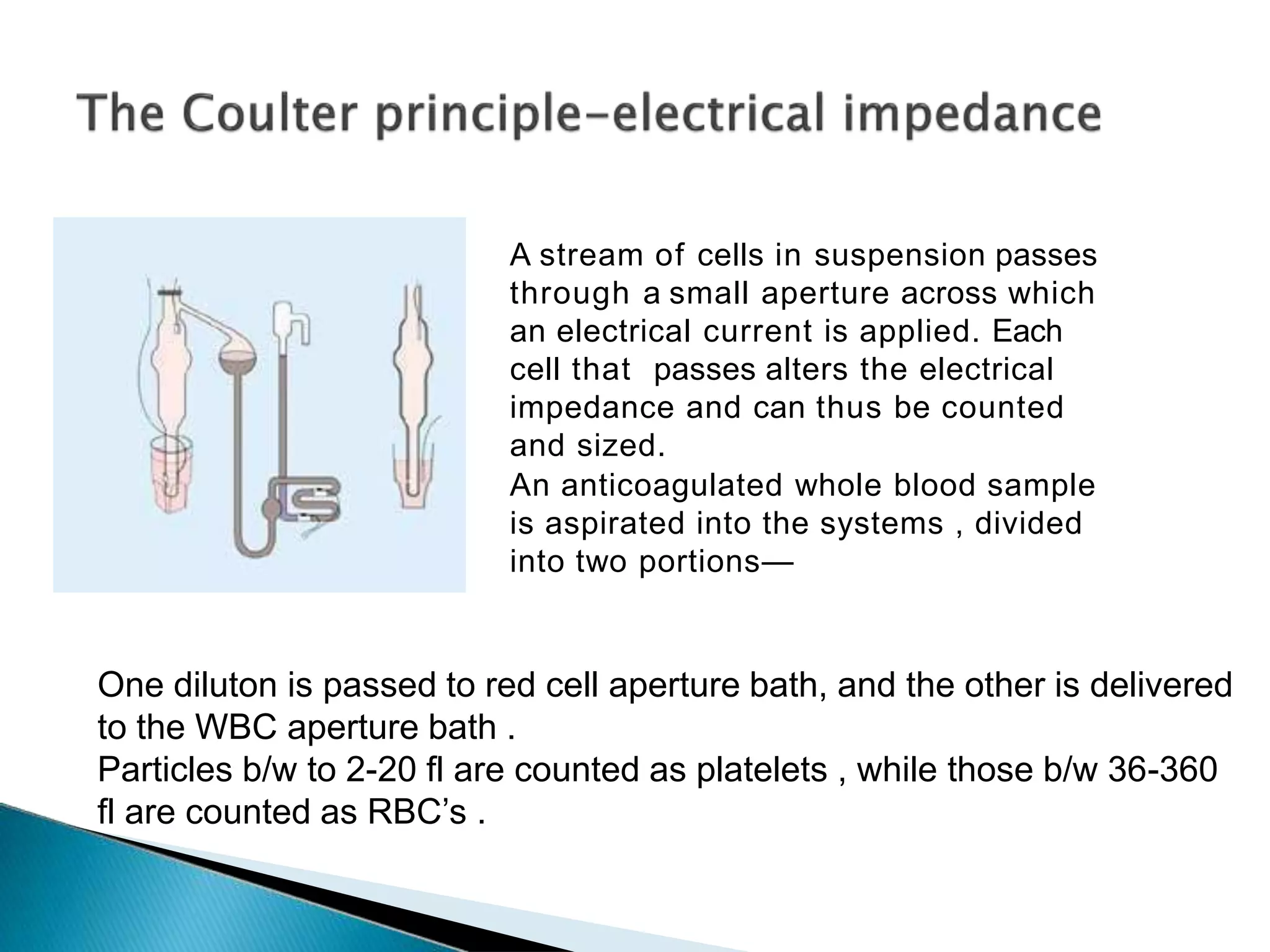
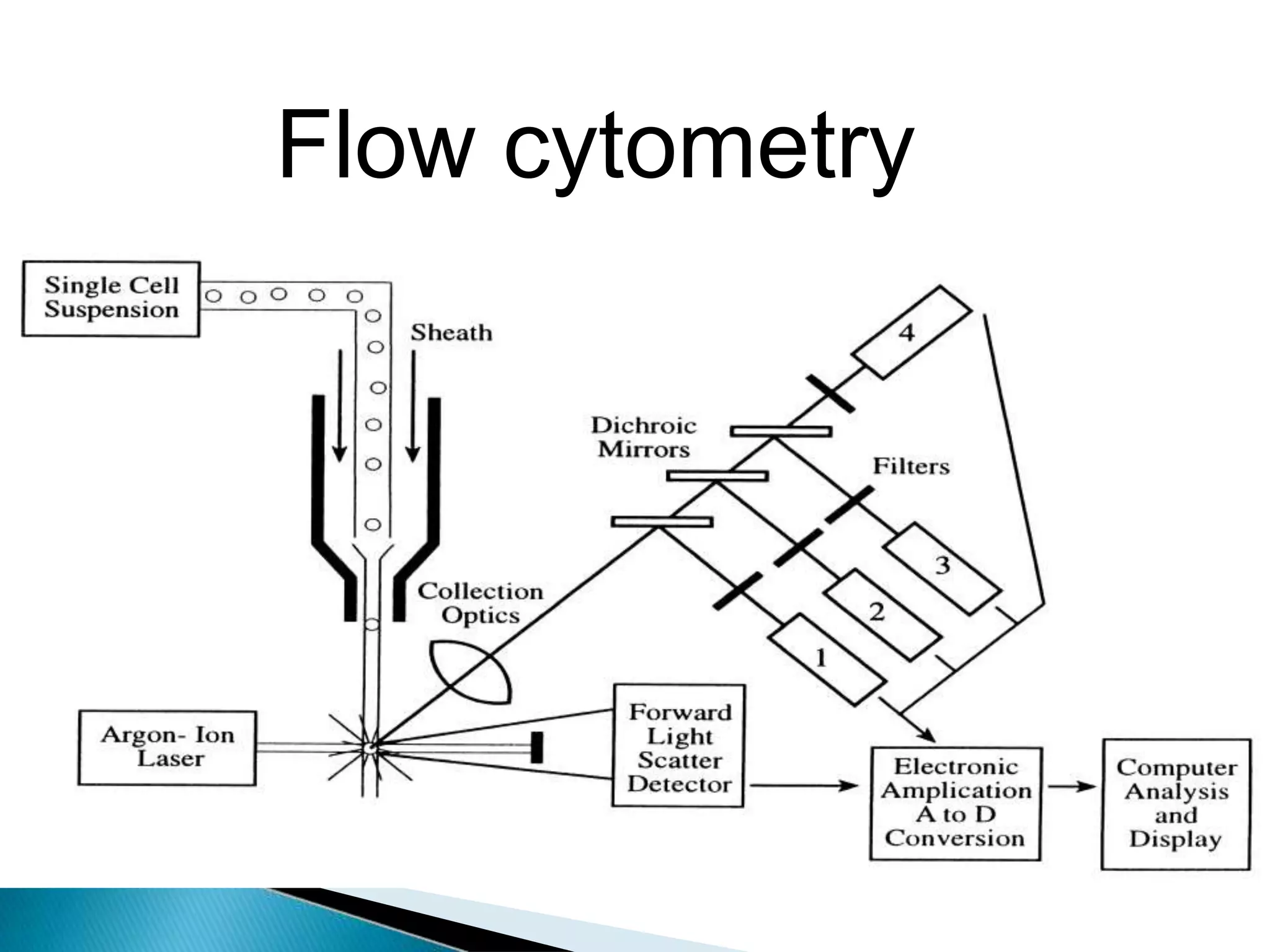
Automated hematology analyzers can perform complete blood counts through various techniques like impedance, light scattering, and fluorescence. There are two types - semi-automated instruments which require some manual steps, and fully automated instruments which only require inserting a blood sample. Automated analyzers provide precise and rapid results for red blood cell count, hemoglobin, hematocrit, white blood cell count with differentials, platelet count, and other indices. While automated counts are generally more accurate for normal samples, manual examination of blood smears is still needed when flags are raised.