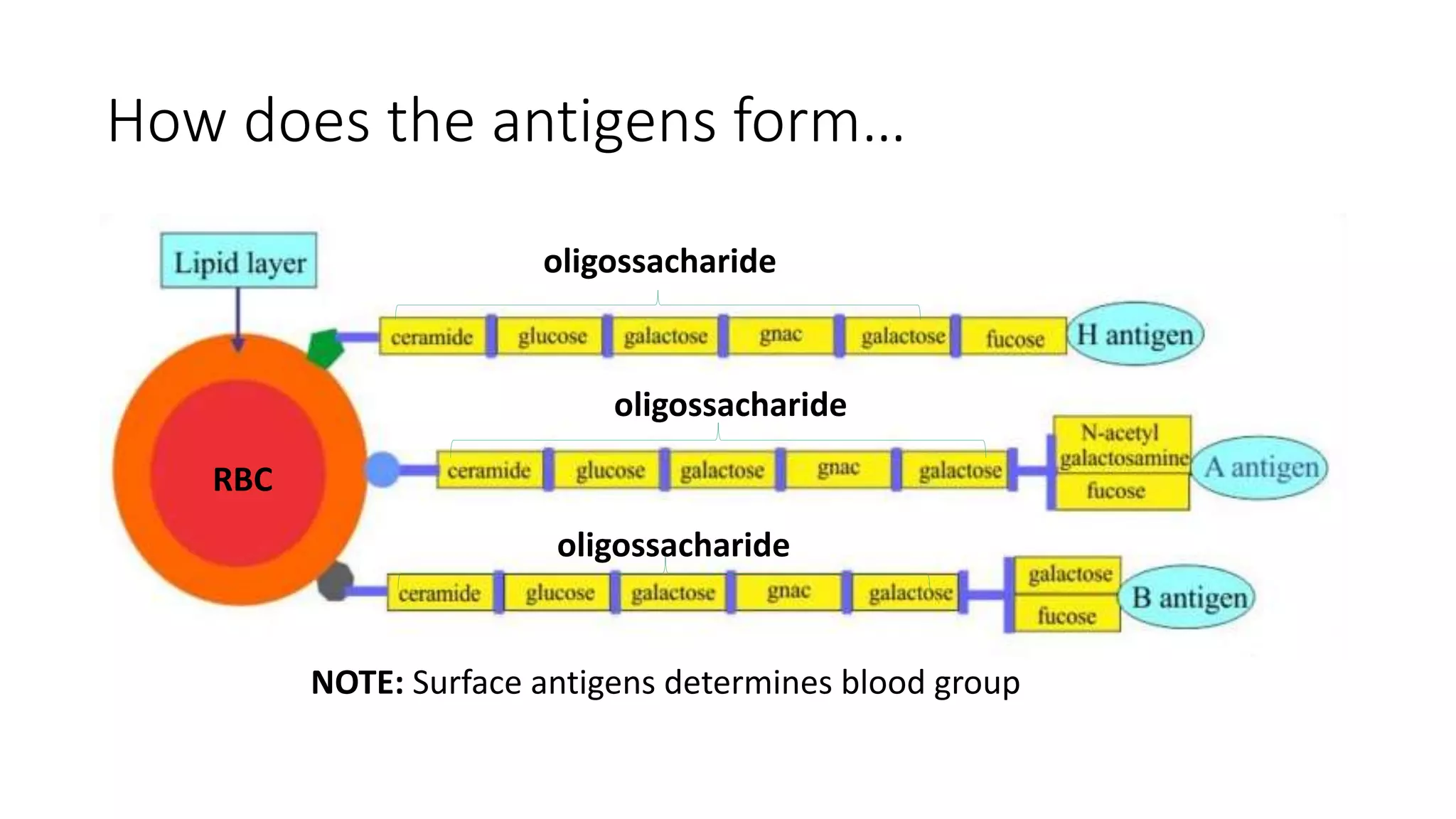
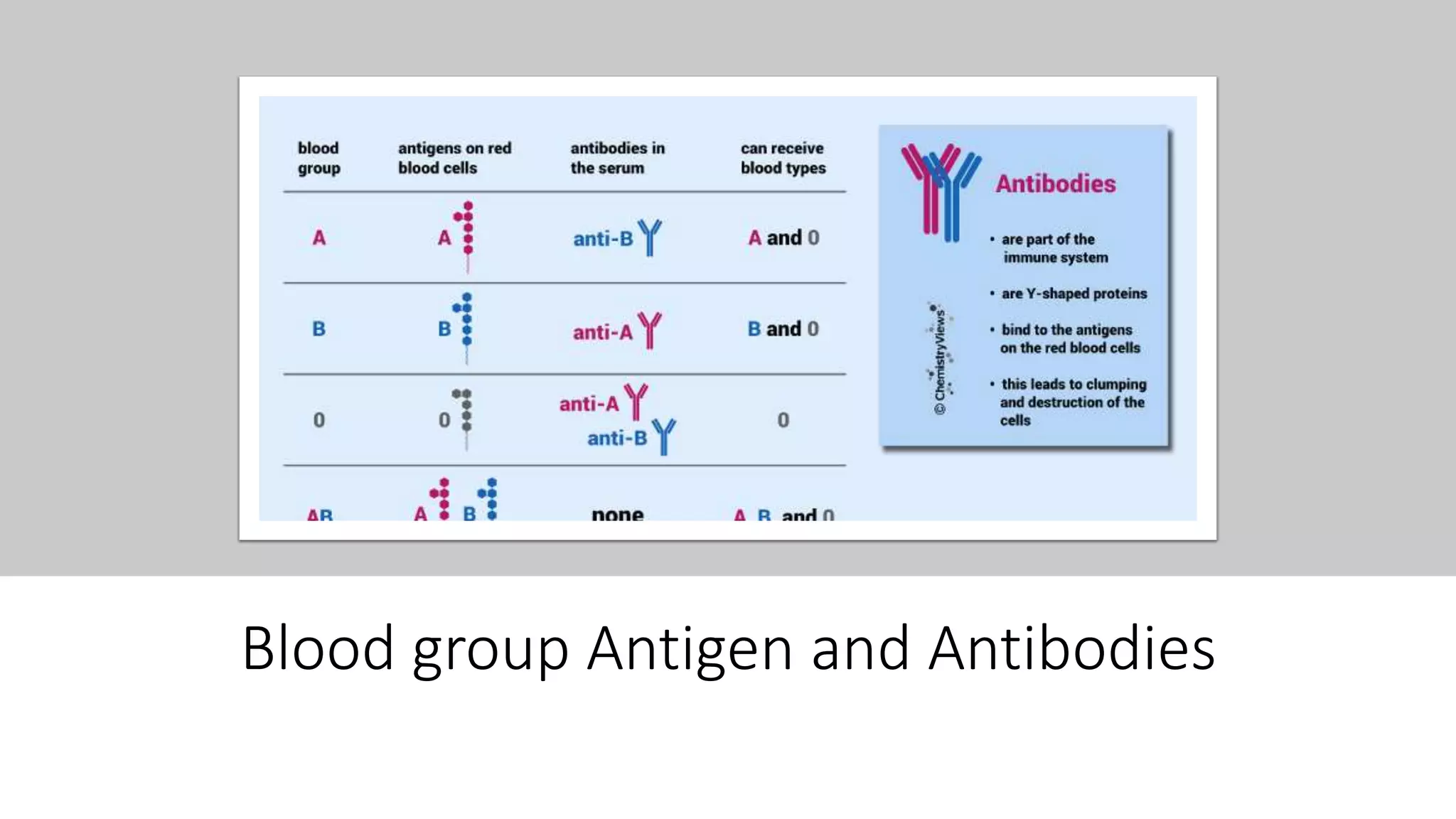
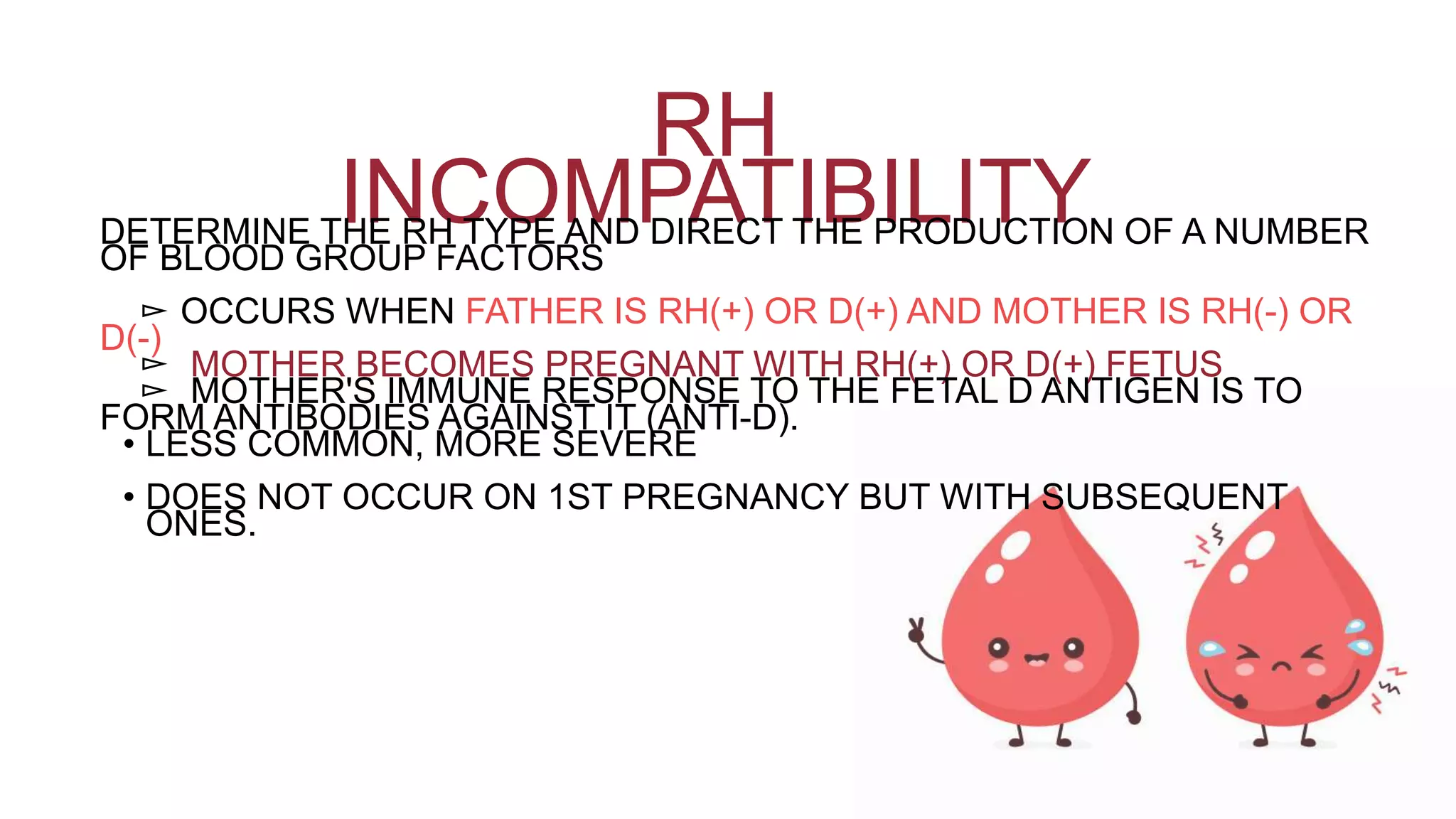
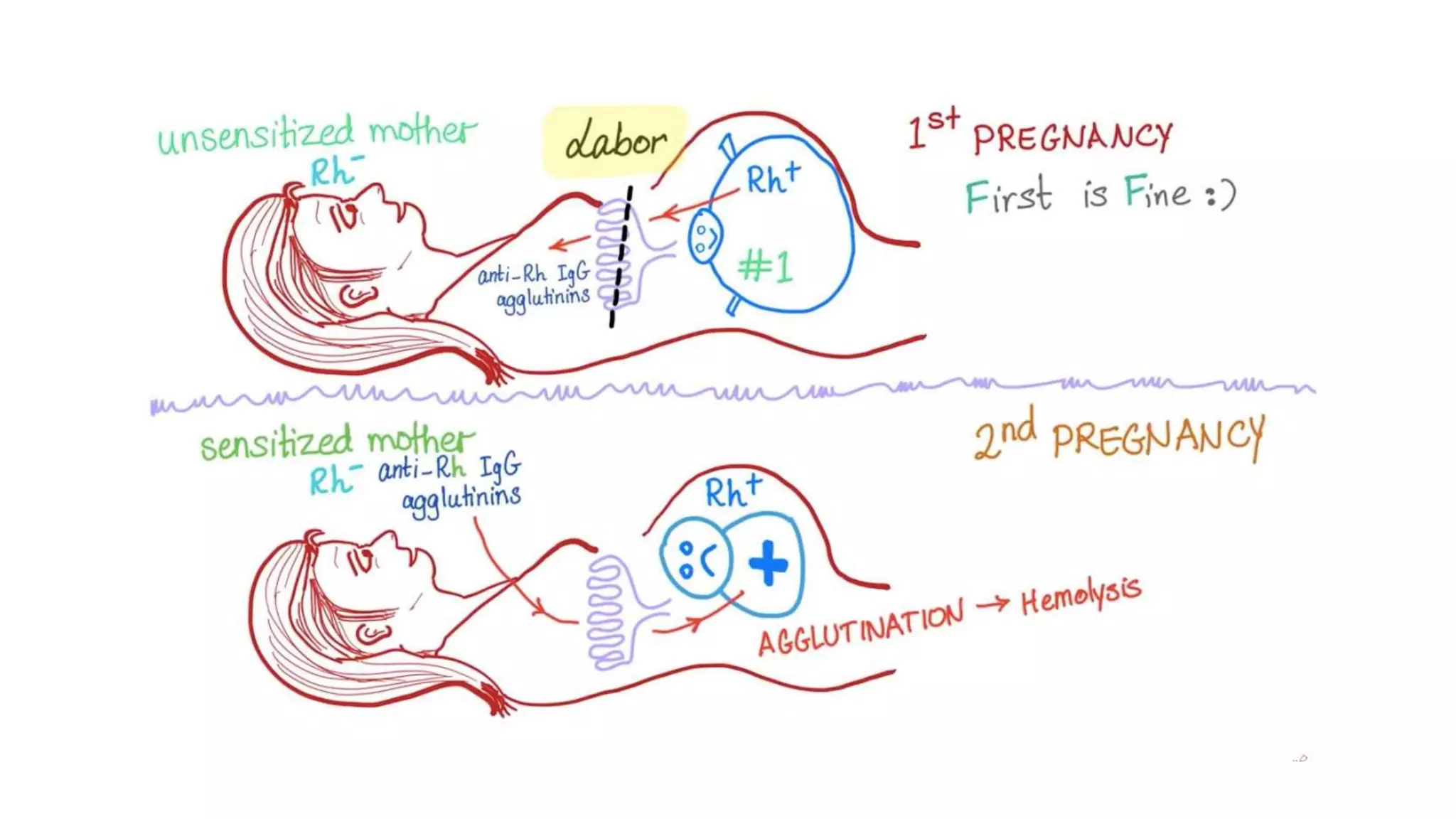
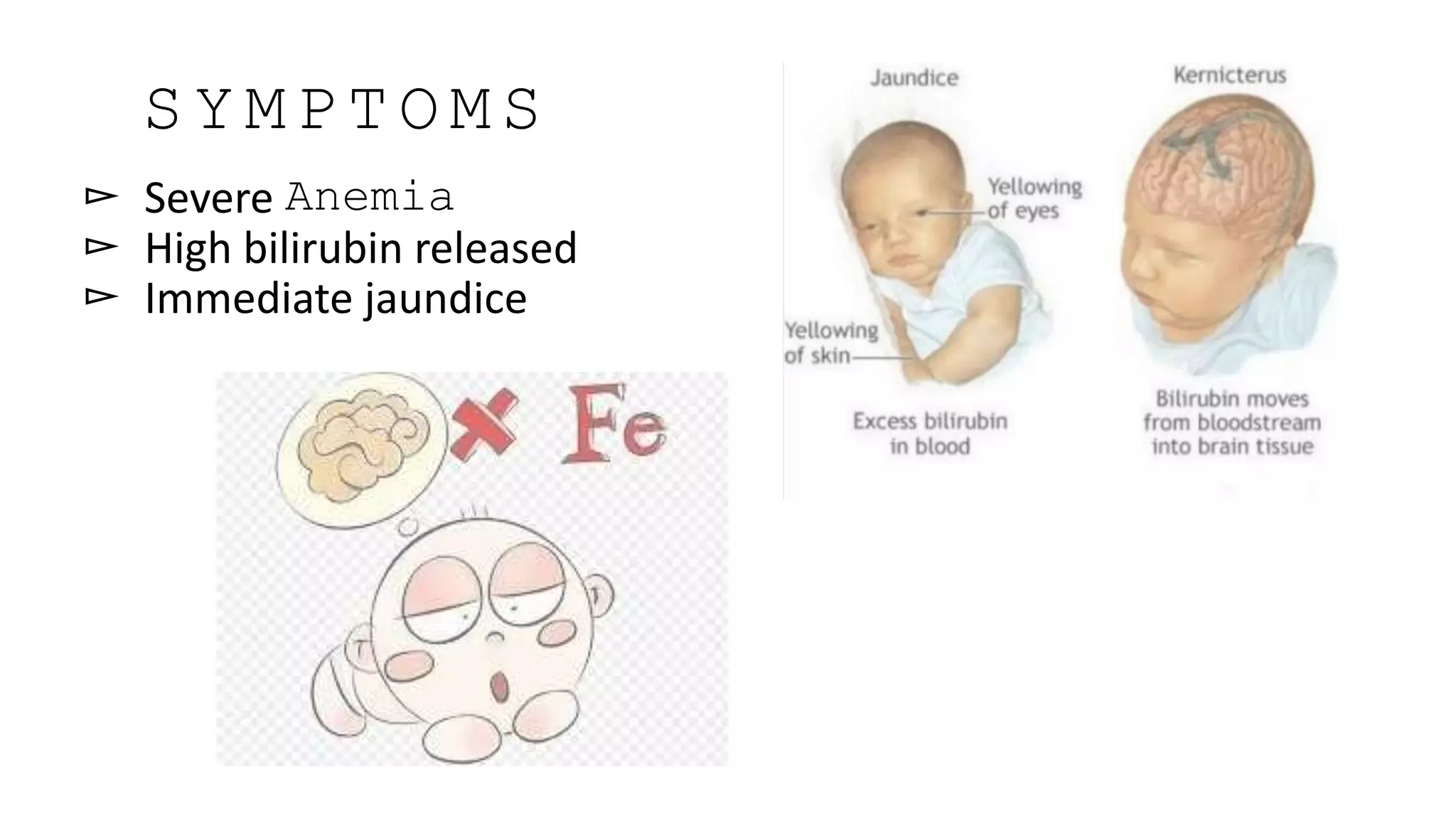
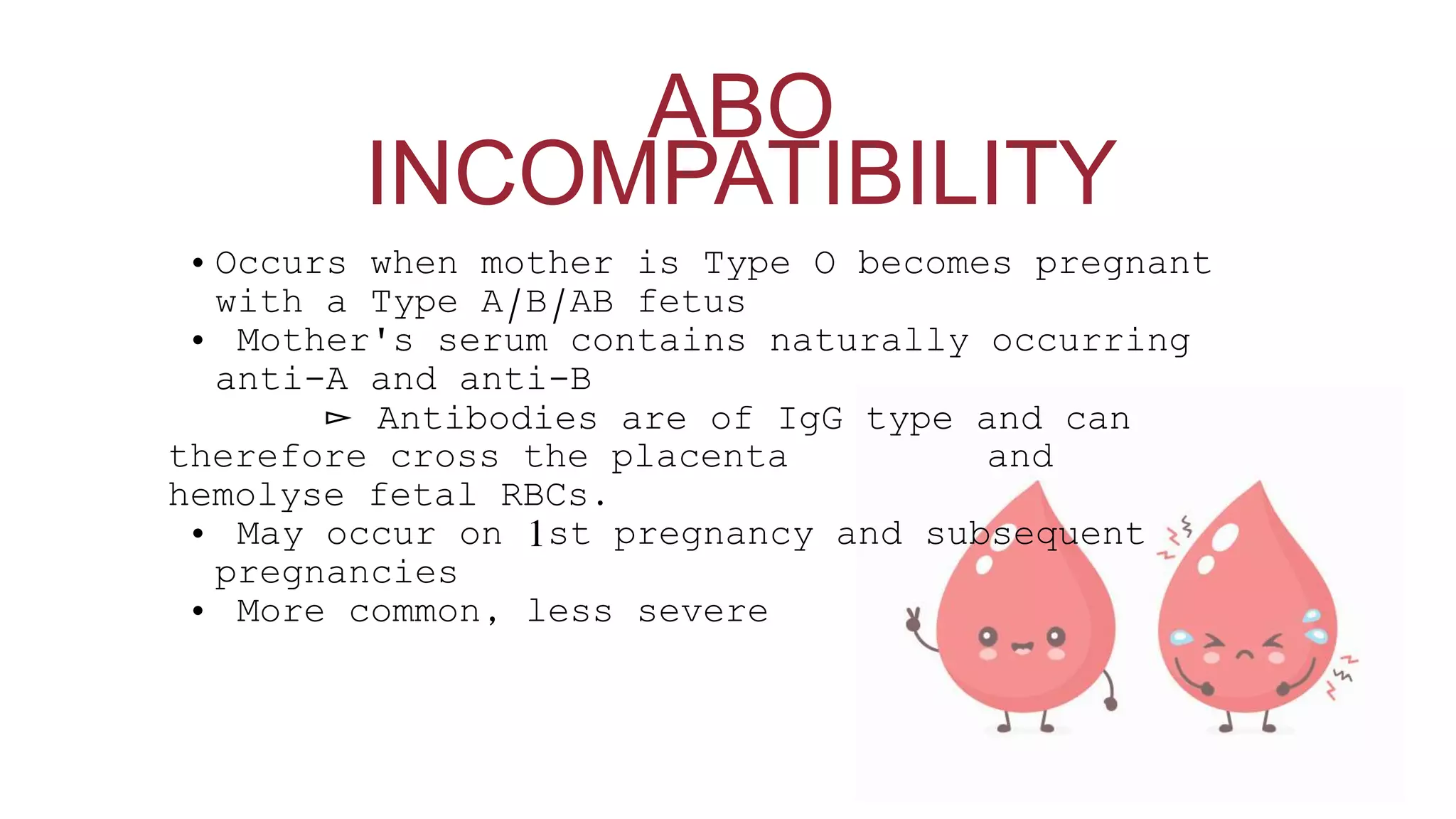
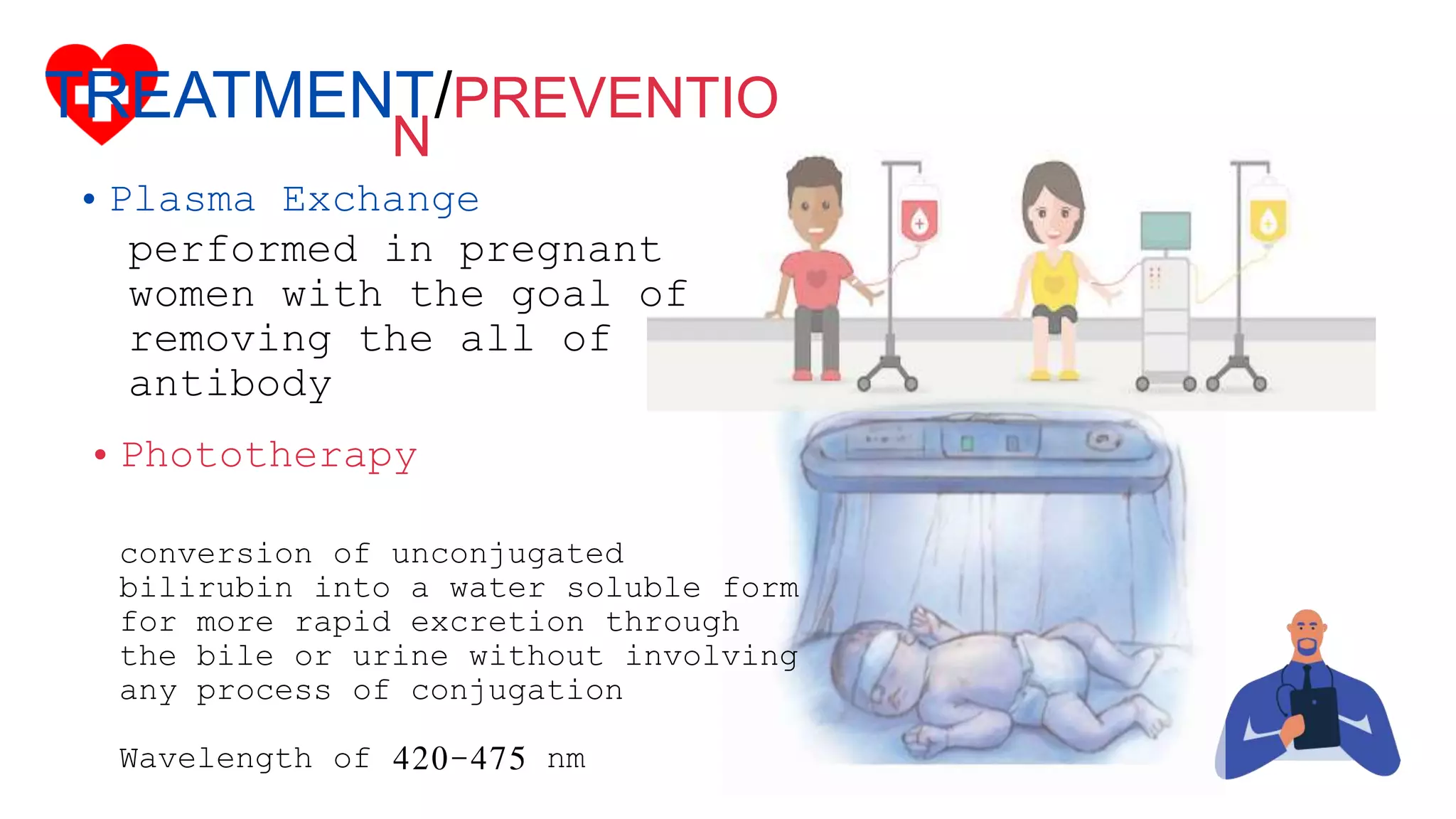
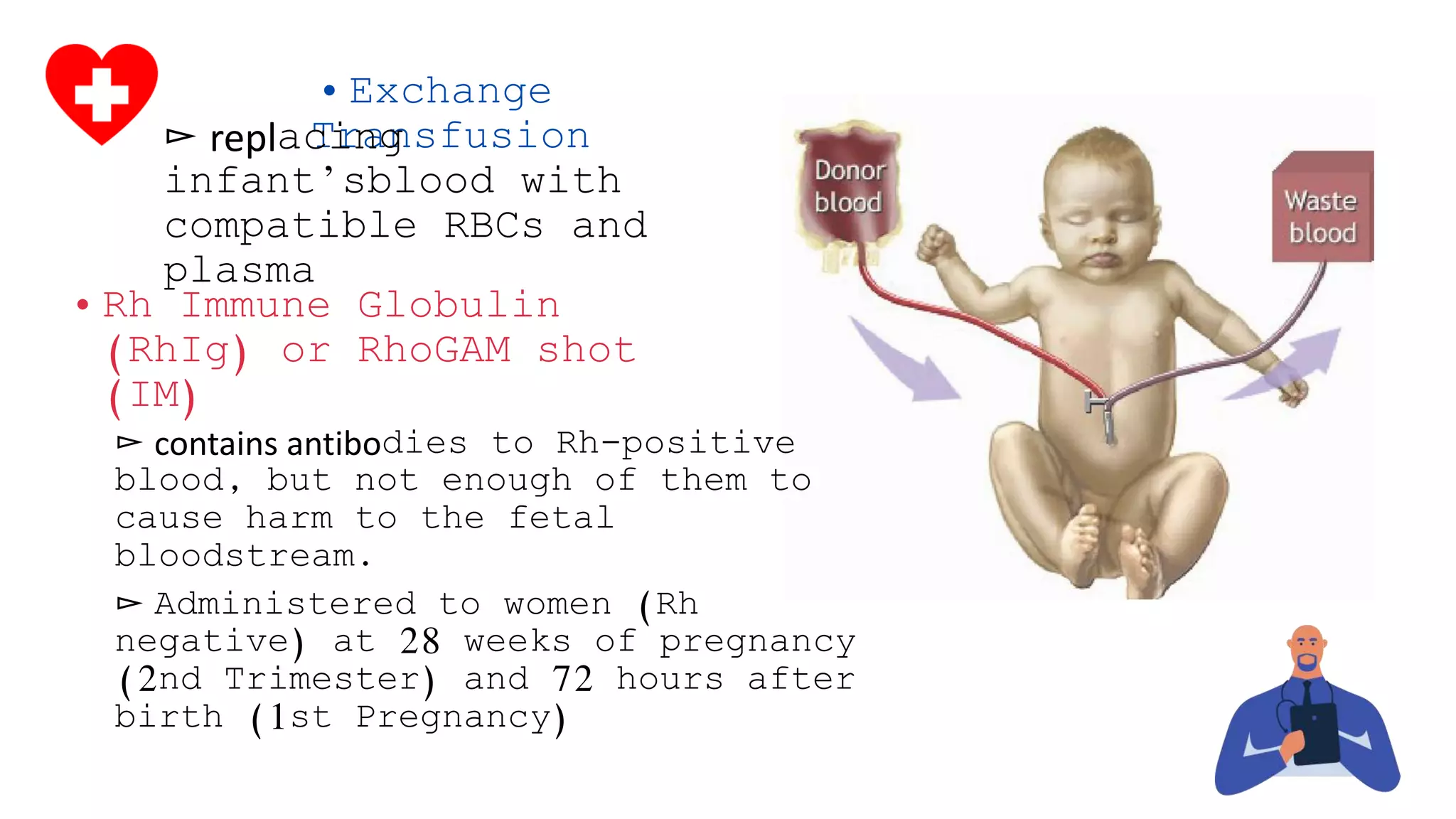
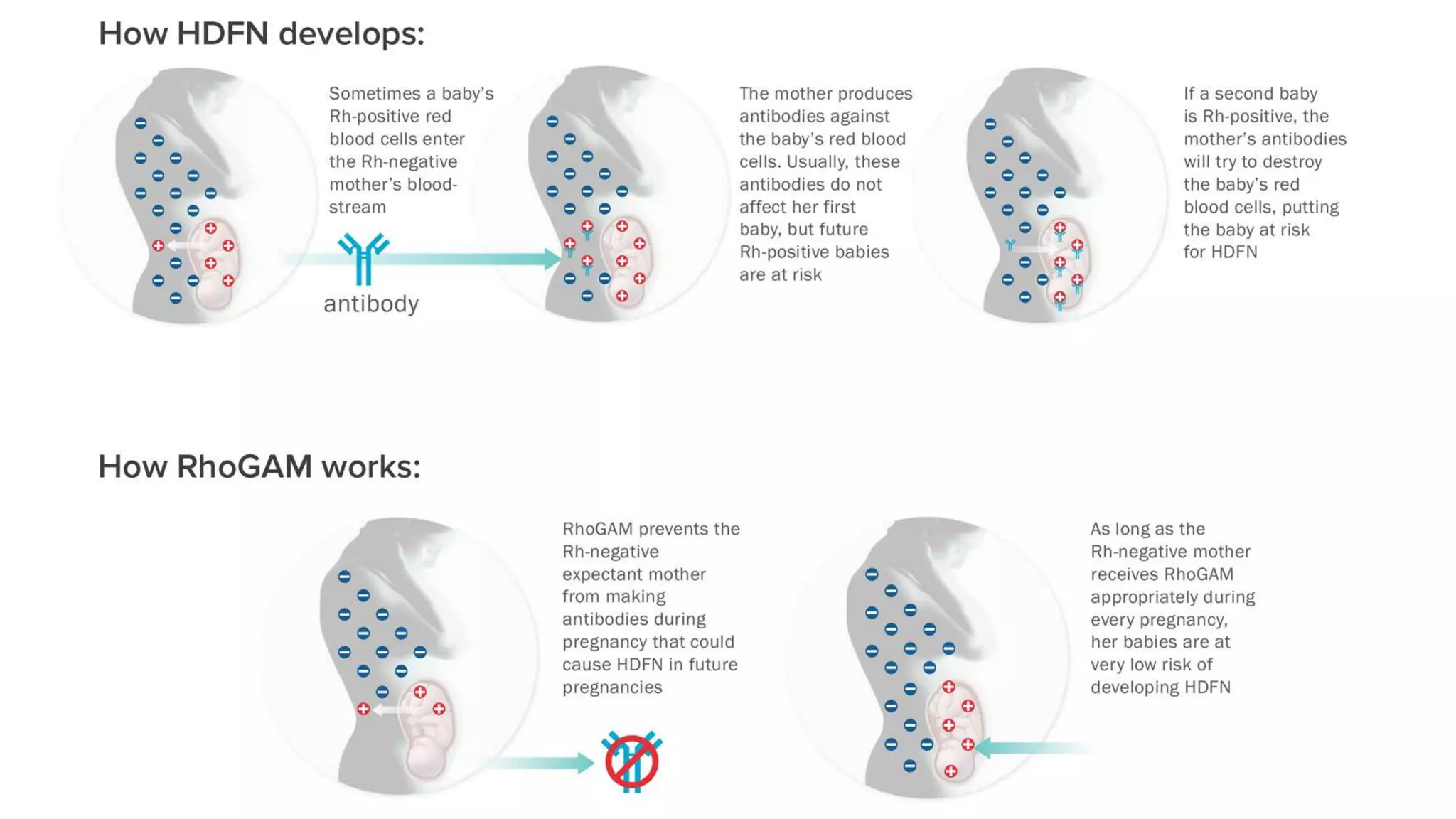
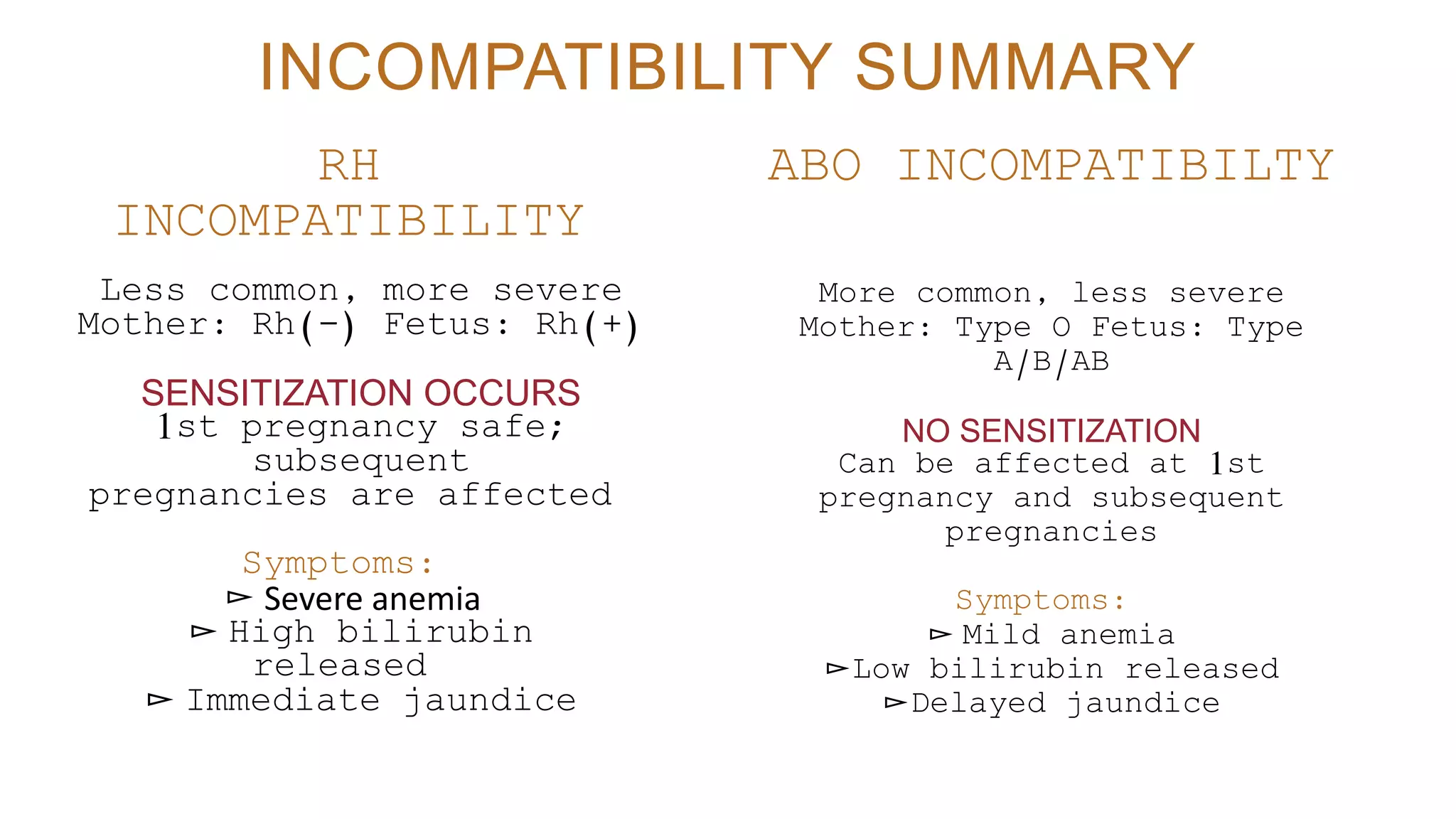
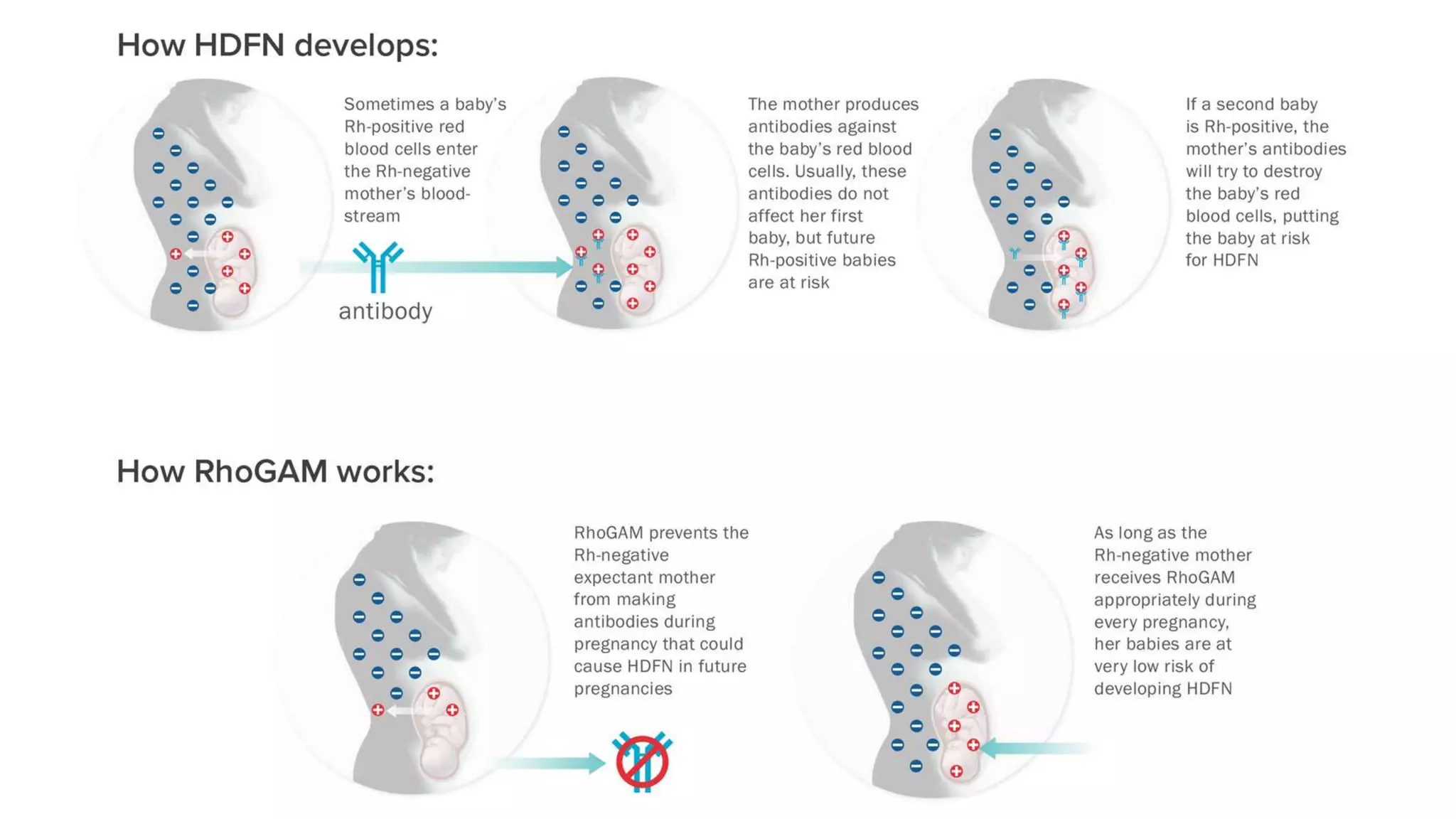
ABO and Rh blood type incompatibilities between mother and fetus can result in hemolytic disease of the newborn. ABO incompatibility is more common but less severe, as the mother's naturally occurring antibodies can cross the placenta and destroy fetal RBCs starting from the first pregnancy. Rh incompatibility is less common but more severe, as sensitization only occurs after the first Rh-positive pregnancy, allowing subsequent pregnancies to be affected. Clinical management includes phototherapy, exchange transfusions, and Rh immune globulin shots to prevent sensitization. Understanding the biochemical basis of blood group antigens and maternal-fetal immune response is important for managing these conditions.
















































![• Hemolytic disease of the Newborn. (2018). Retrieved from Stanford Children's Health:
https://www.stanfordchildrens.org/en/topic/default?id=hemolytic-disease-of-the-newborn-90-P02368
• Dean L. Blood Groups and Red Cell Antigens [Internet]. Bethesda (MD): National Center for
Biotechnology Information (US); 2005. Chapter 4, Hemolytic disease of the newborn. Available from:
https://www.ncbi.nlm.nih.gov/books/NBK2266/
• Rodwell, V., Bender, D., Botham, K., Kennelly, P., & Weil., P. (2015). Harper’s illustrated biochemistry
(30th ed.). New York, NY: Mcgraw-Hill Education.
• Dr. Najeeb Lectures https://www.drnajeeblectures.com/](https://image.slidesharecdn.com/group2-aboreportsept-201019101220/75/ABO-Blood-Type-Incompatibility-76-2048.jpg)
