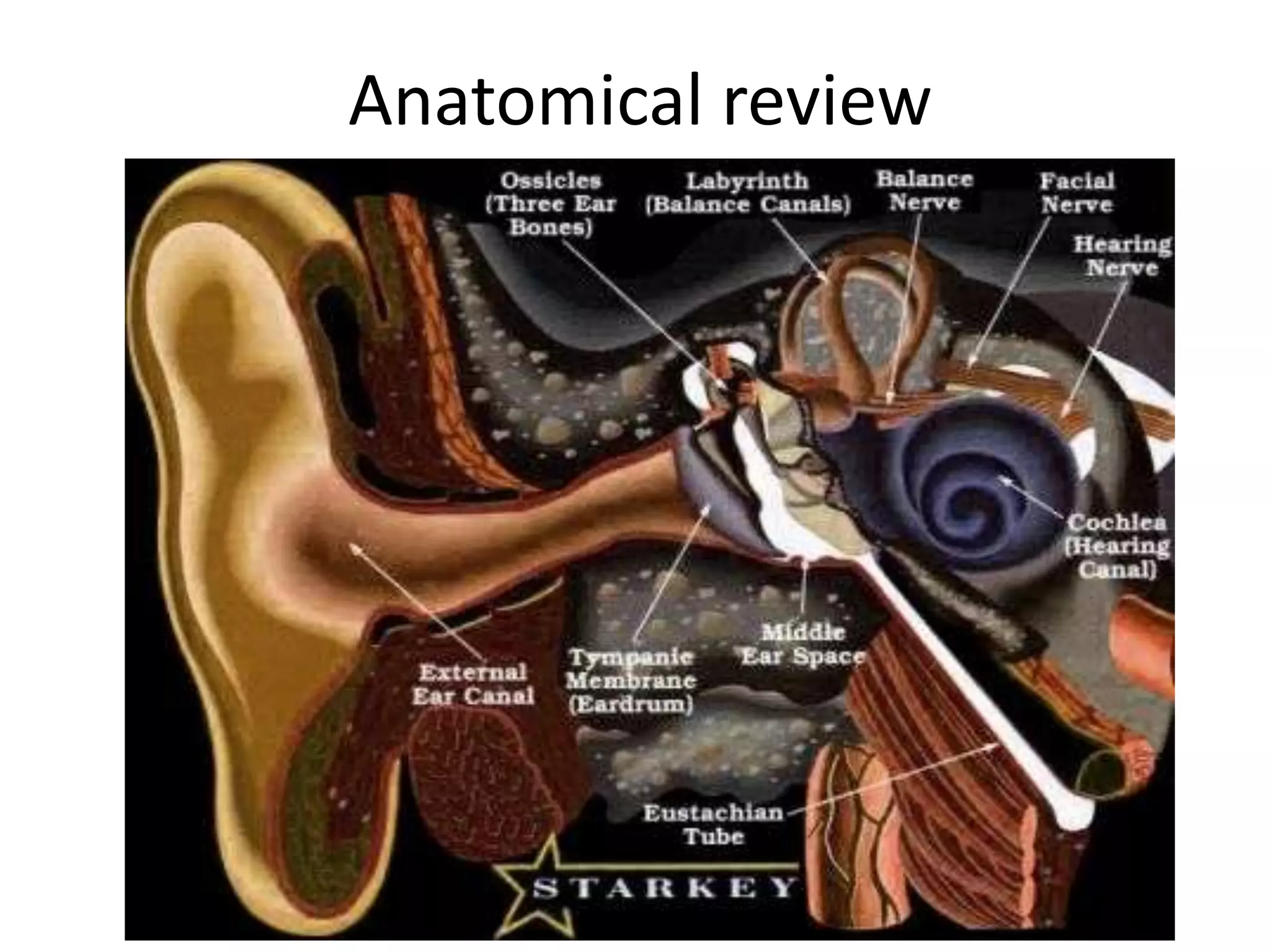
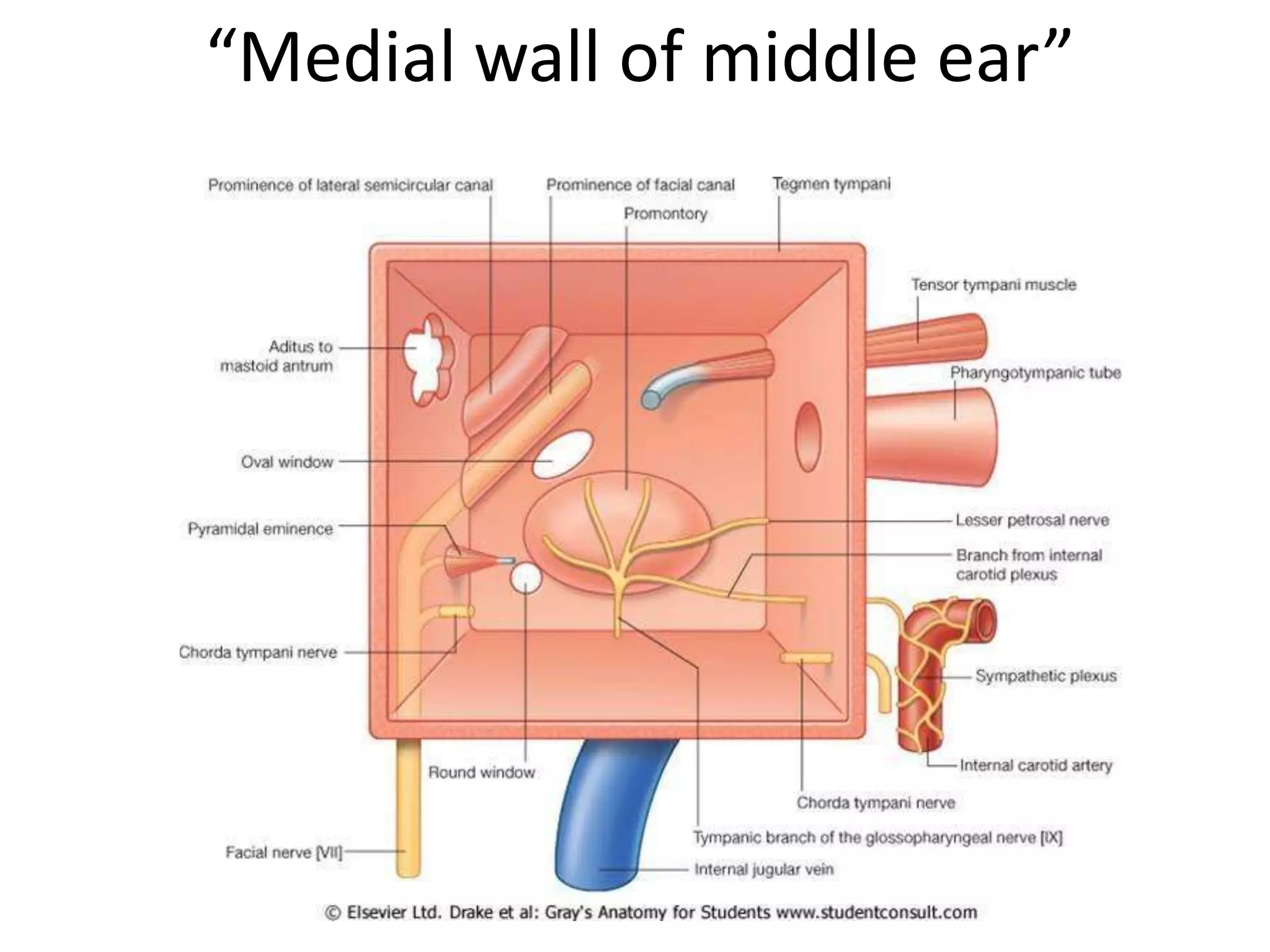
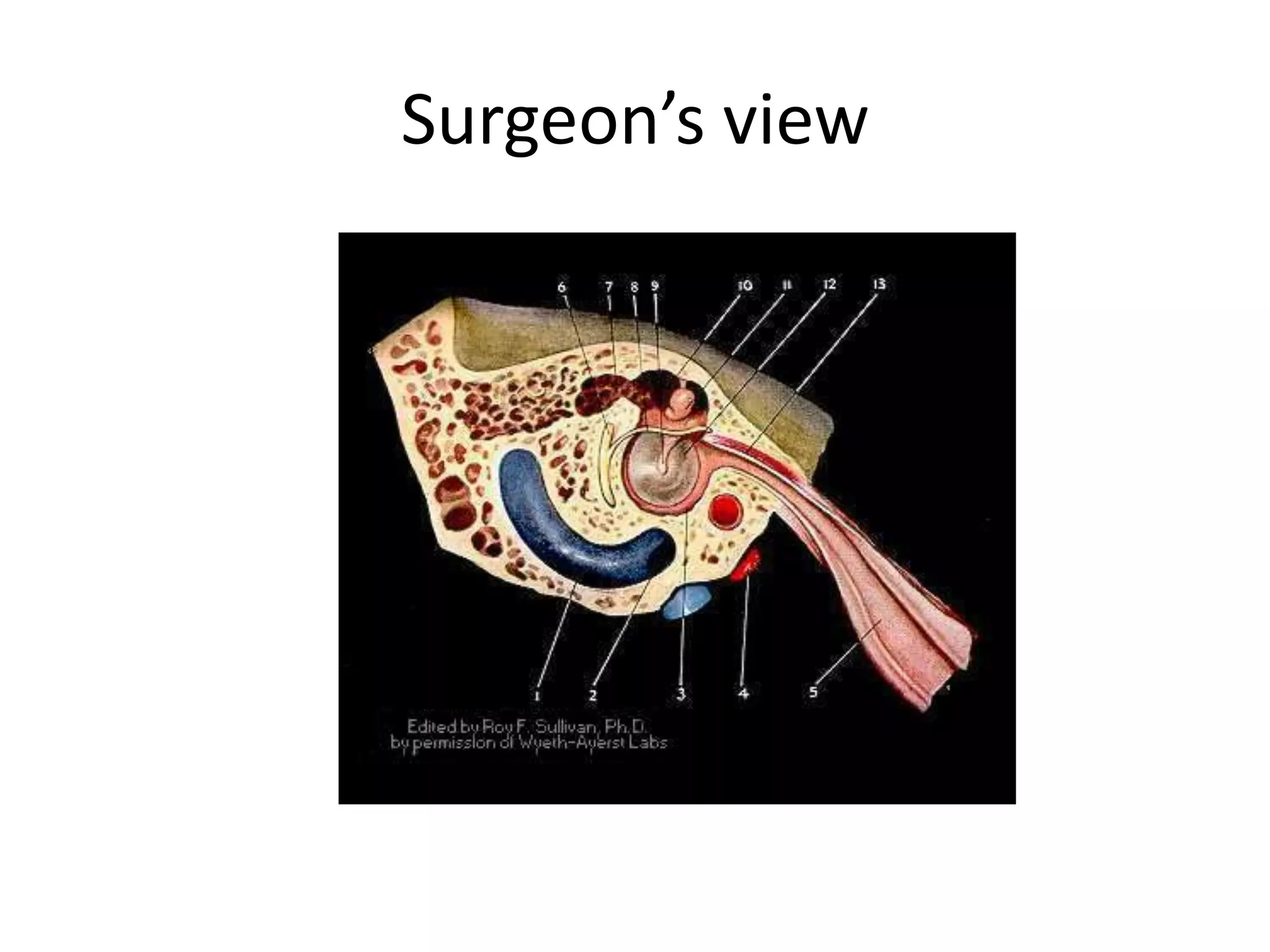
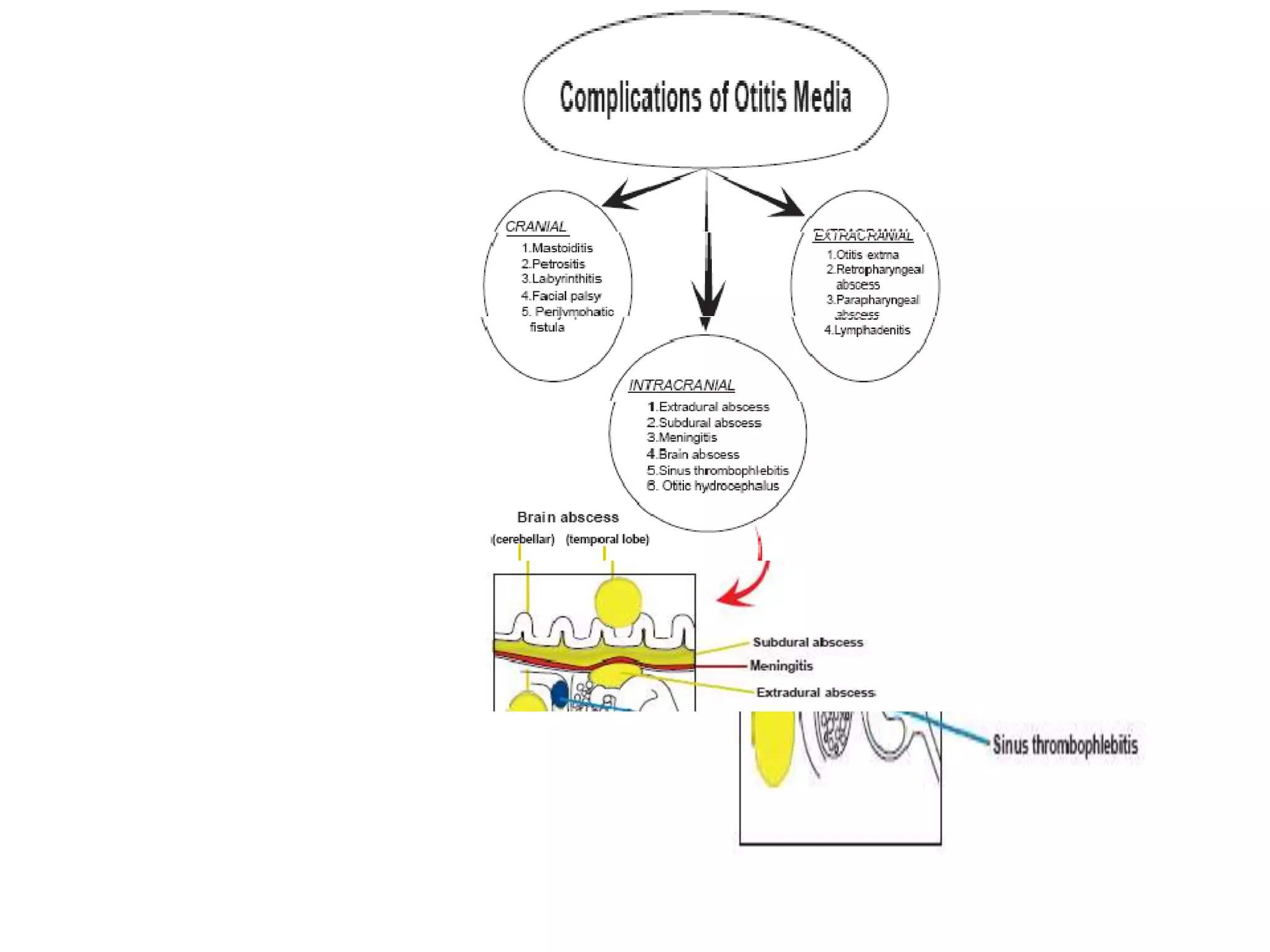
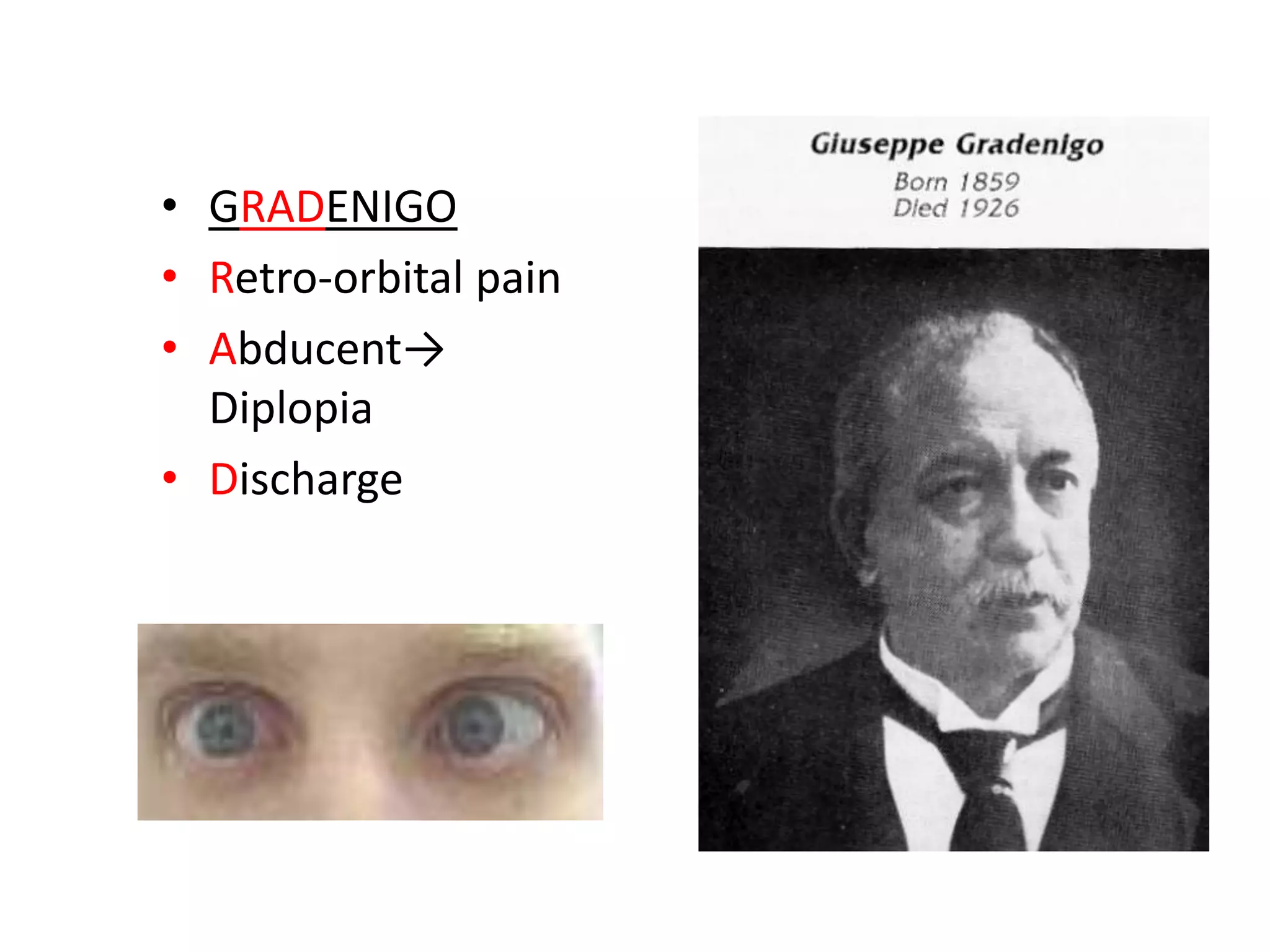
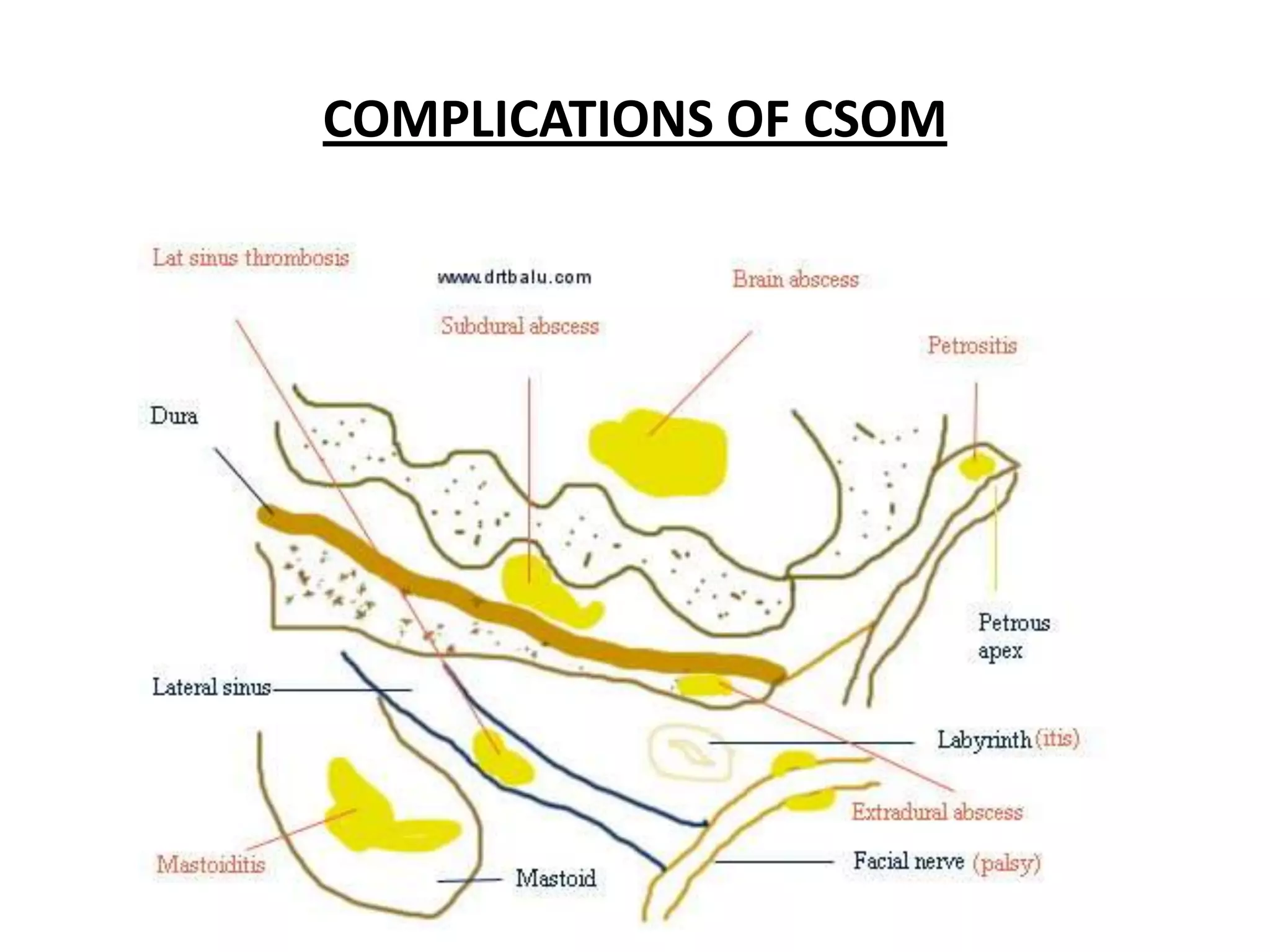
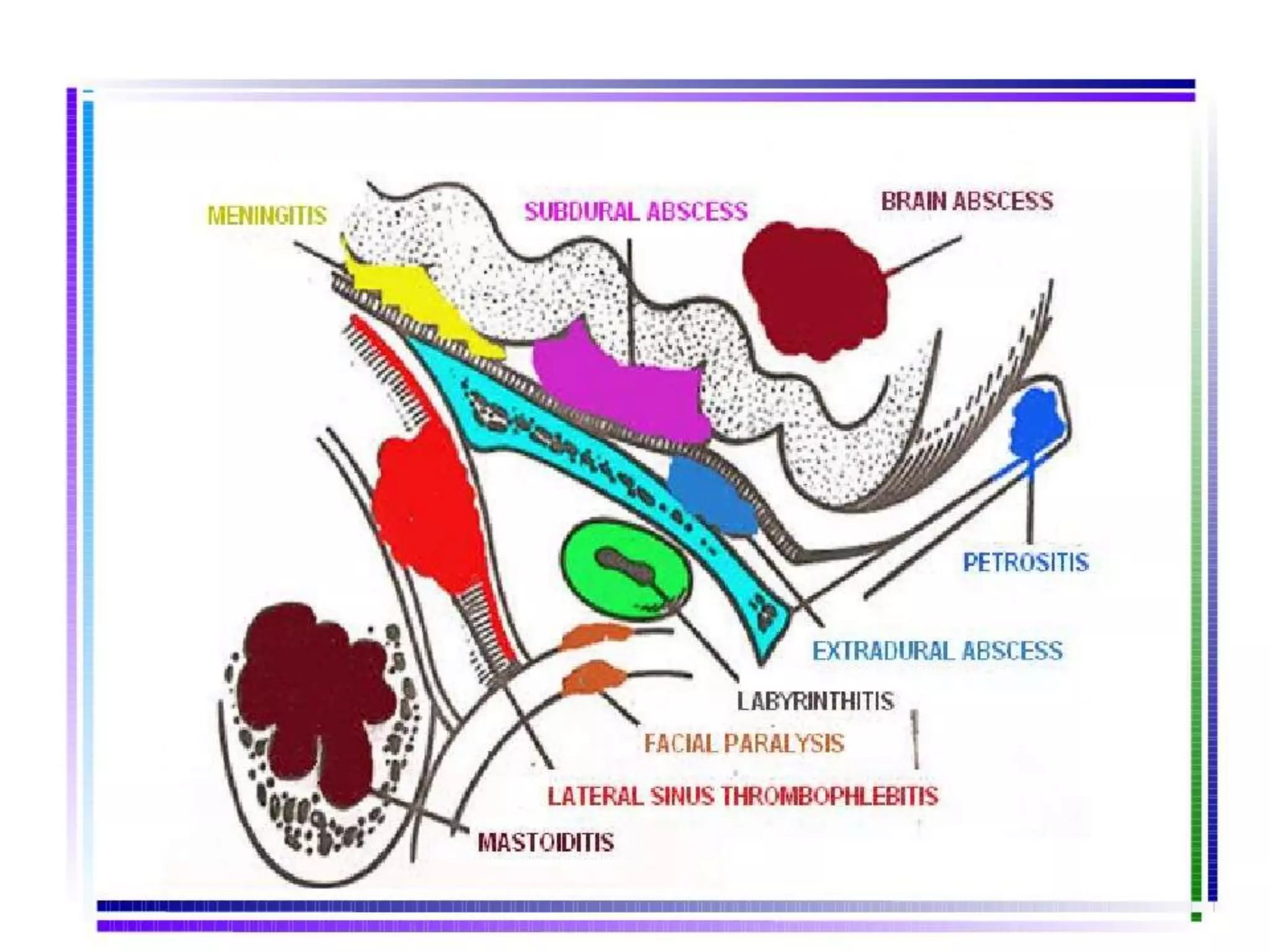
1. Chronic suppurative otitis media (CSOM) can lead to both cranial (intratemporal) and extra-cranial complications. Cranial complications include mastoiditis, petrositis, labyrinthitis, facial paralysis, and perilymphatic fistula.
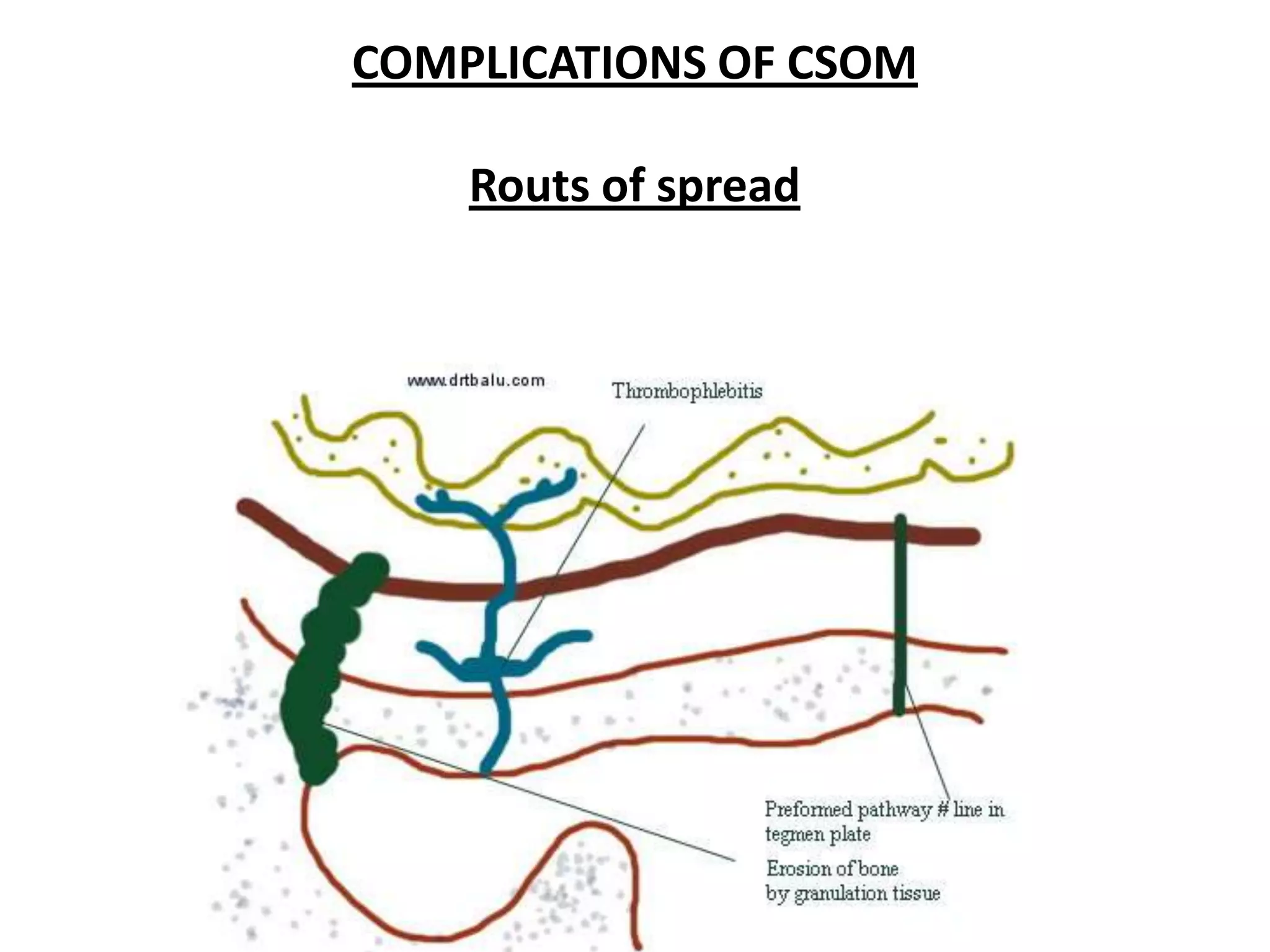
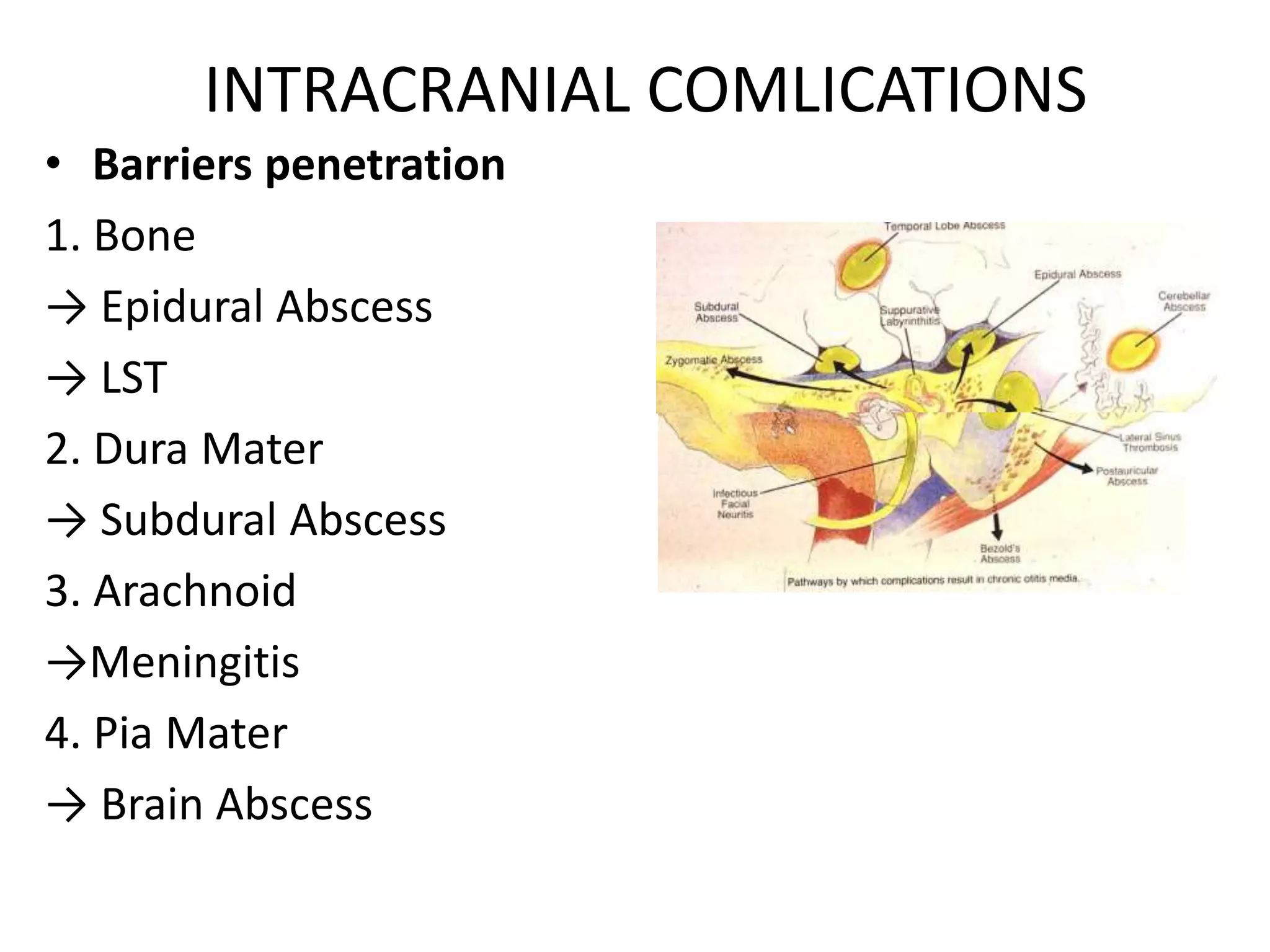
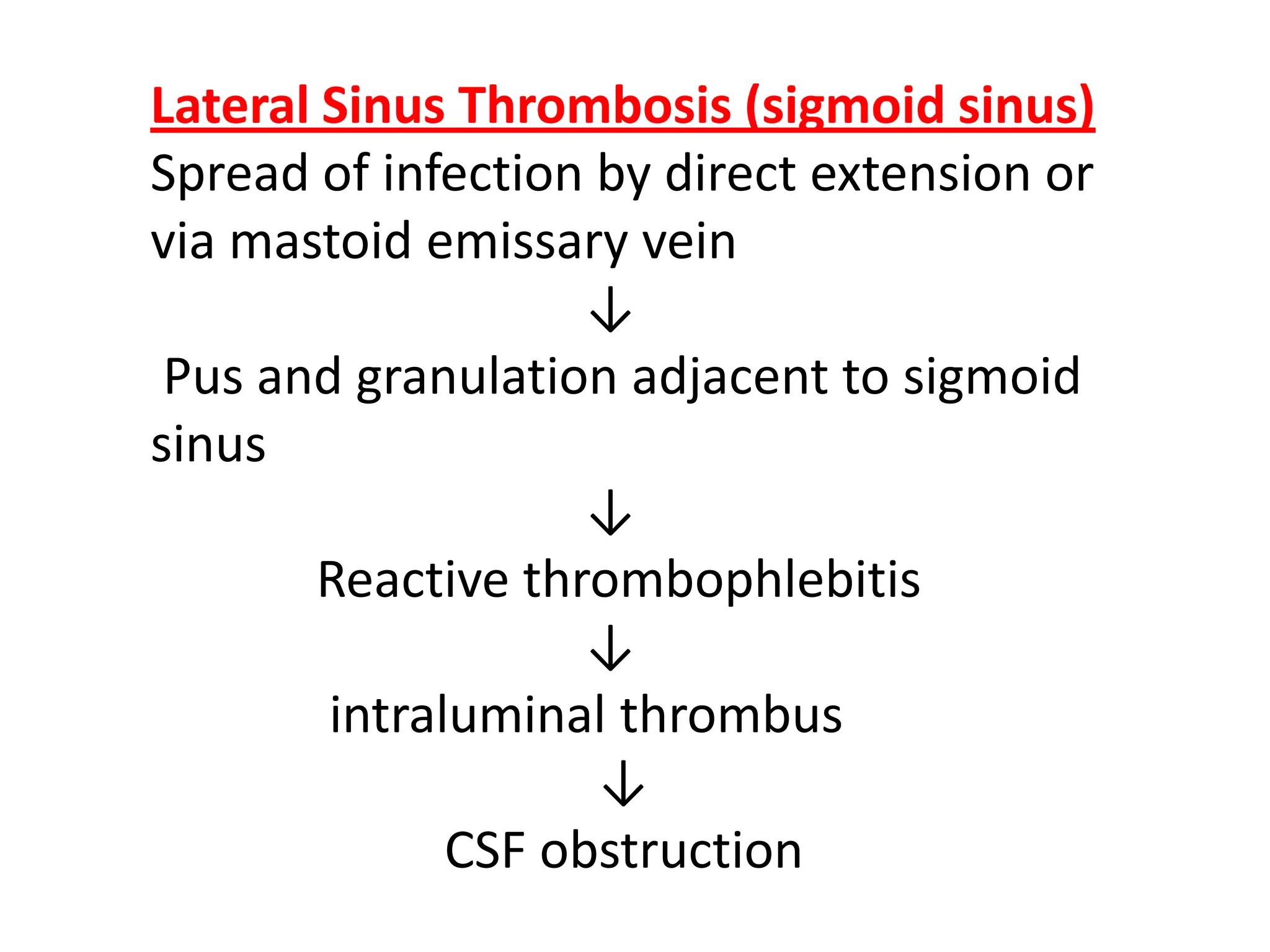
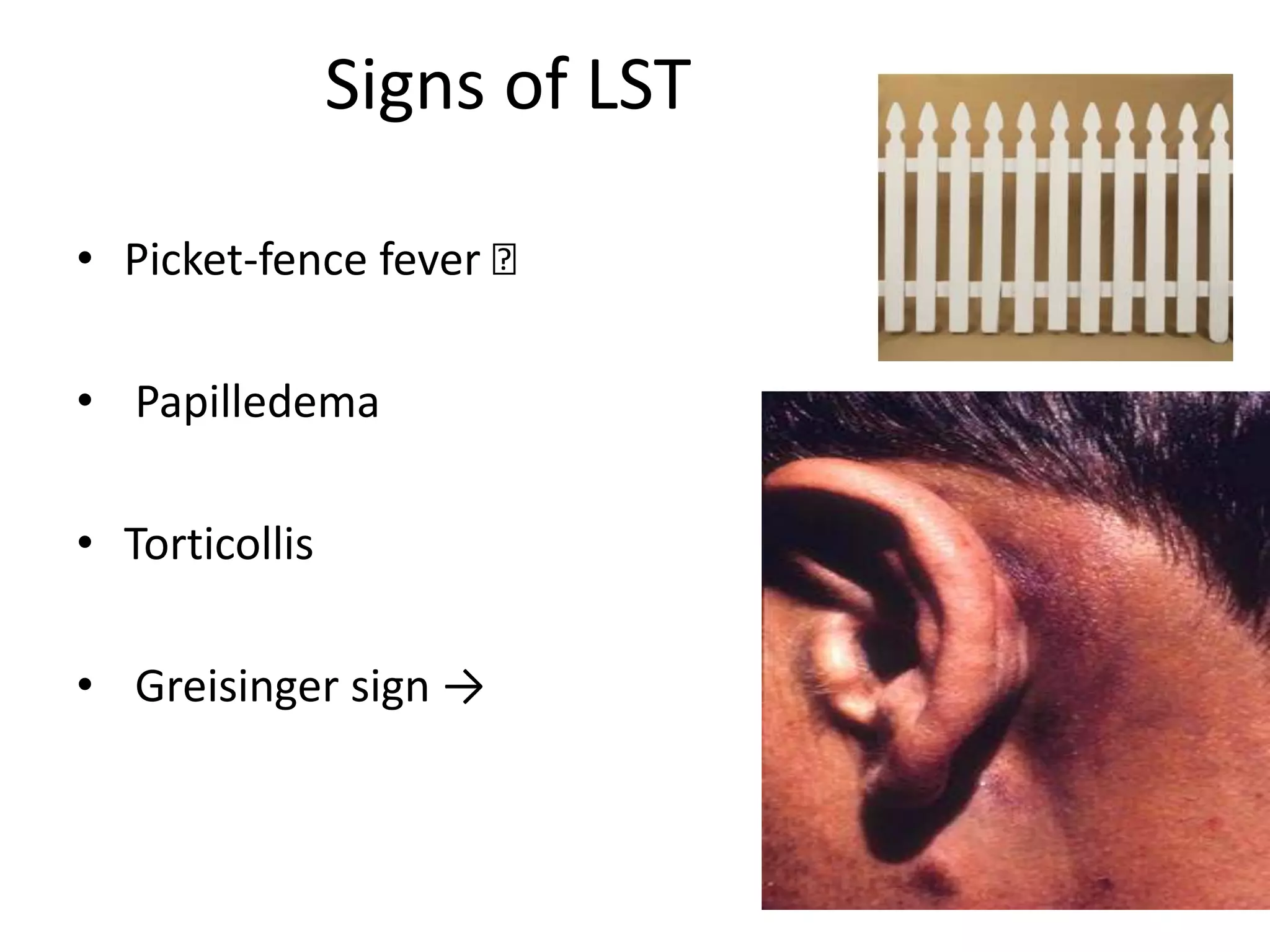
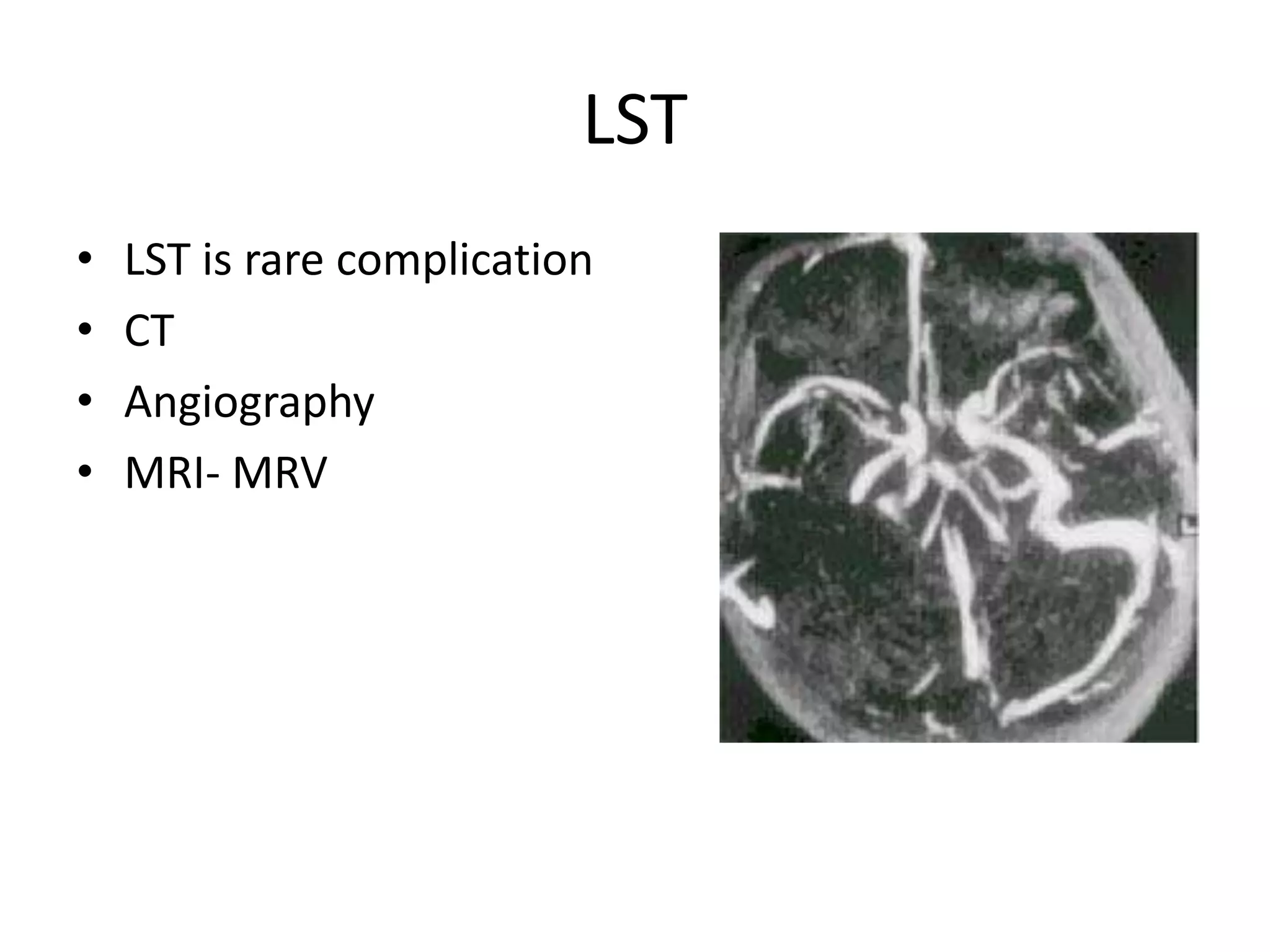
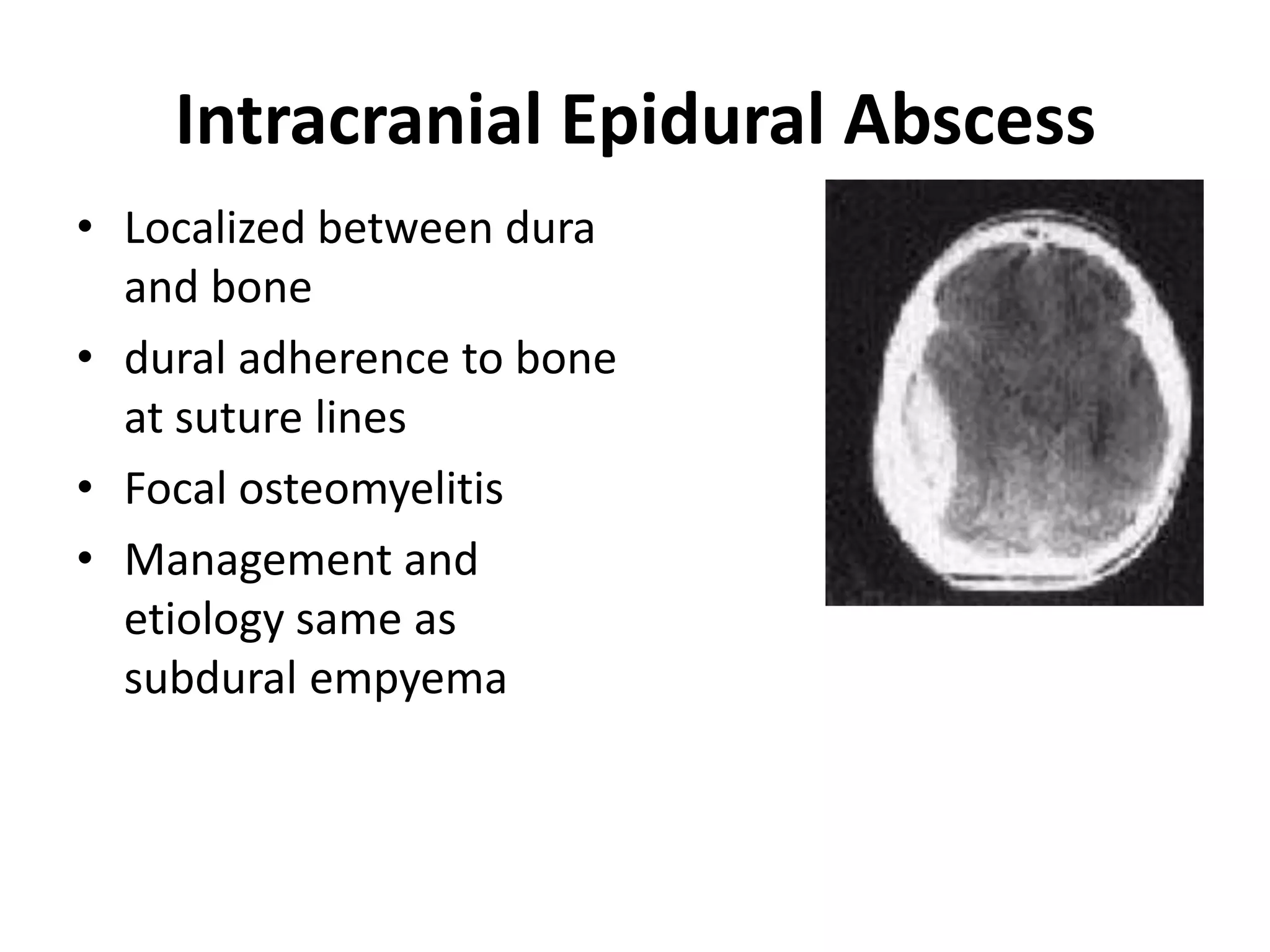
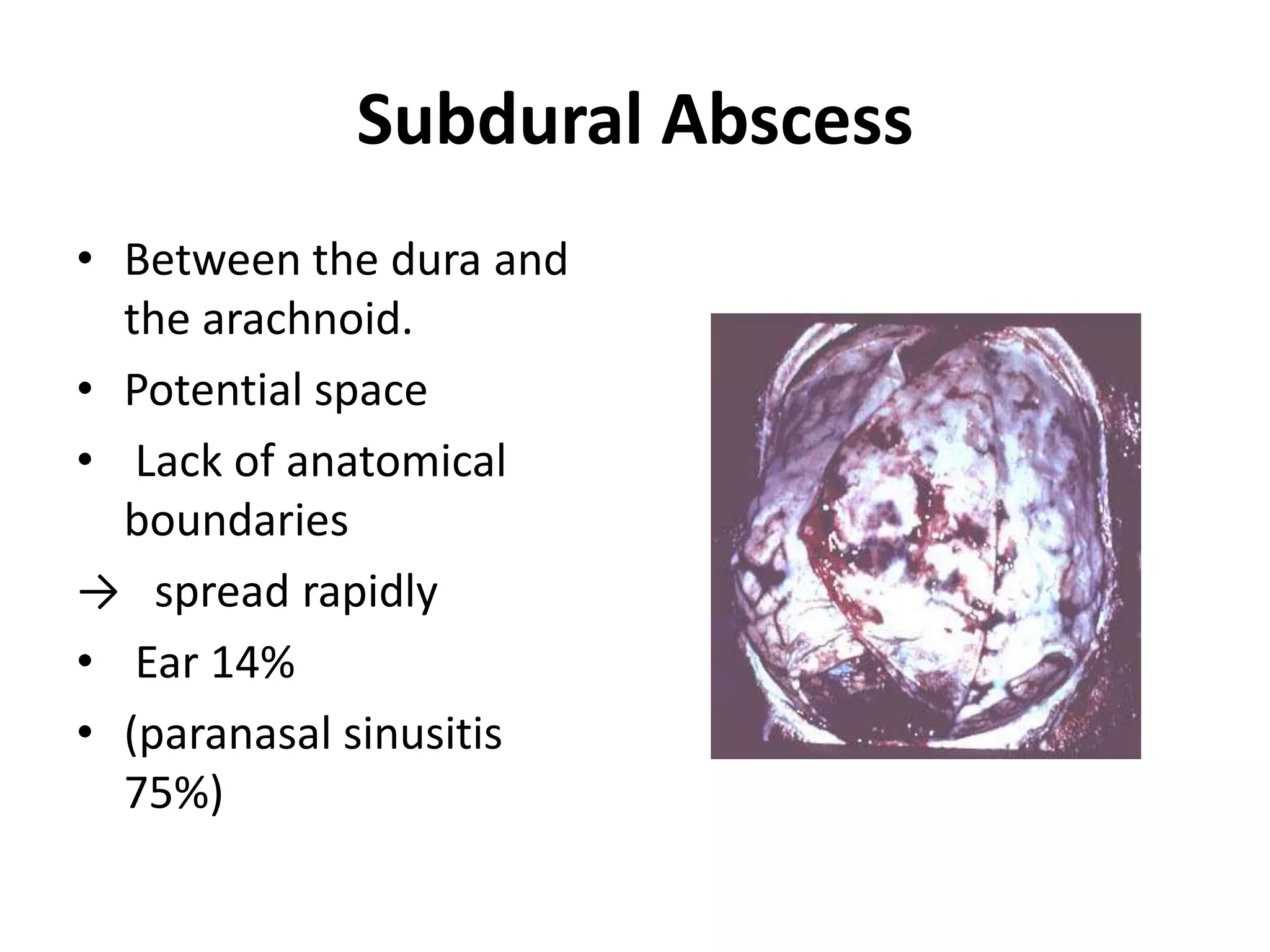
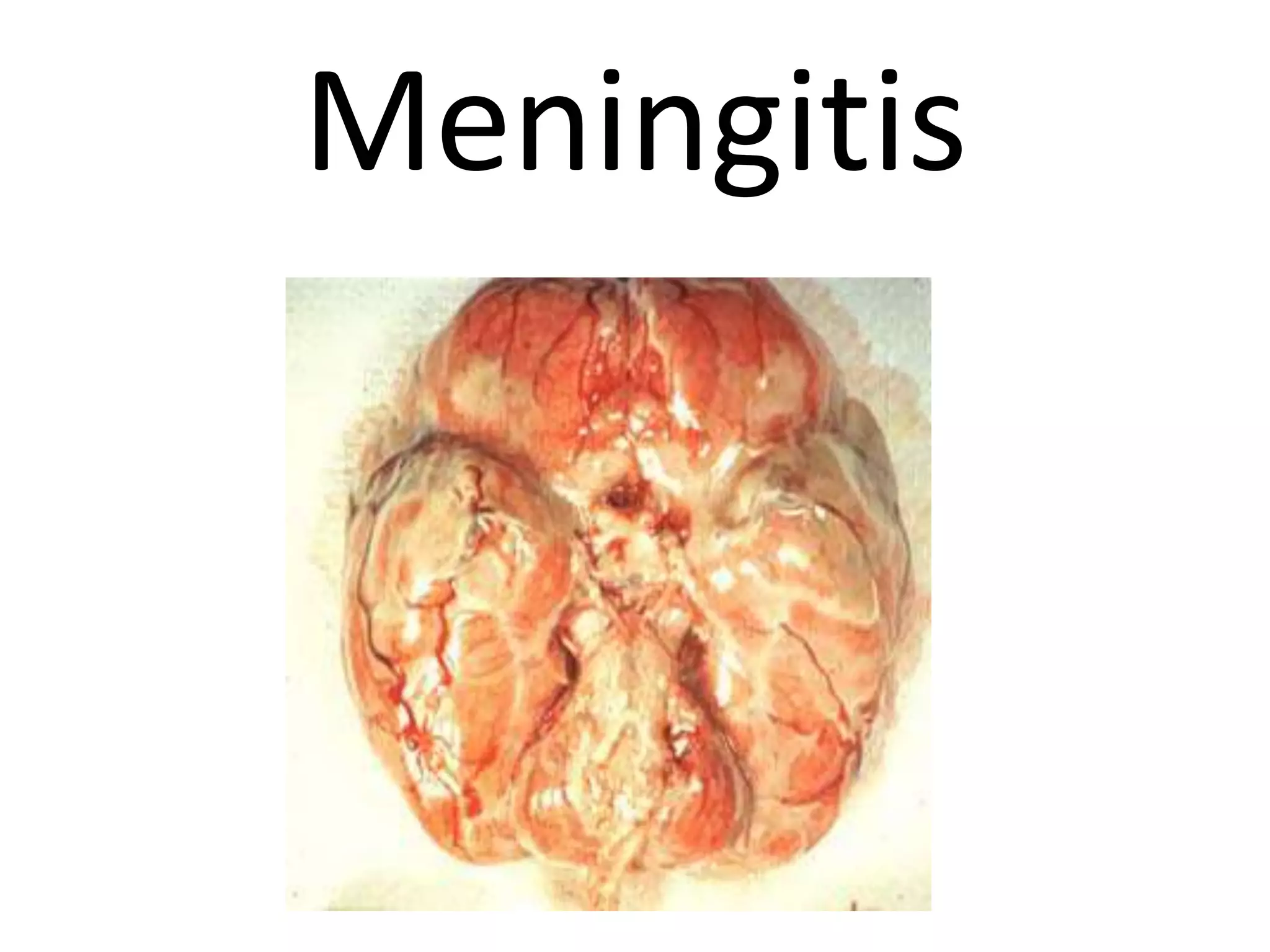
2. Intra-cranial complications occur when infections penetrate bony barriers and spread to the dura mater, arachnoid, or pia mater, causing epidural abscesses, subdural abscesses, meningitis, or brain abscesses. Lateral sinus thrombosis is a serious complication resulting from direct extension or via the mastoid emissary vein.
3.