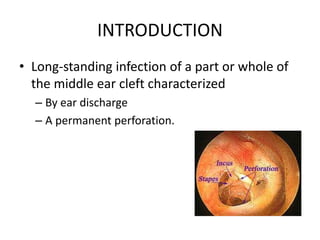
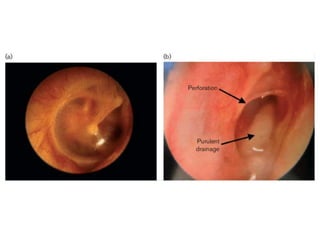
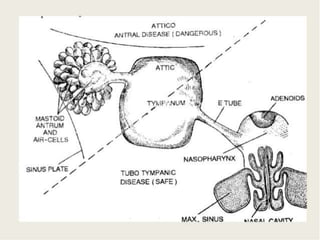
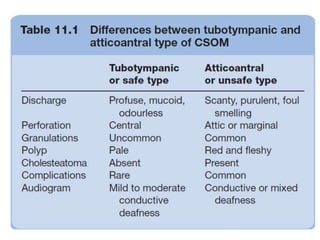
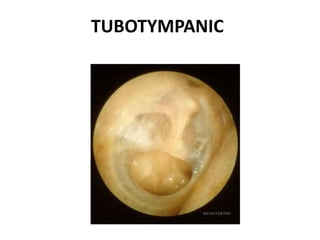
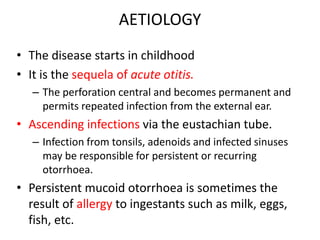
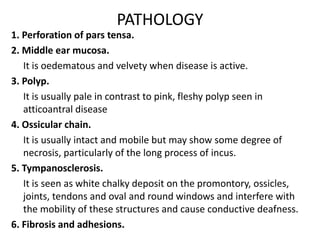
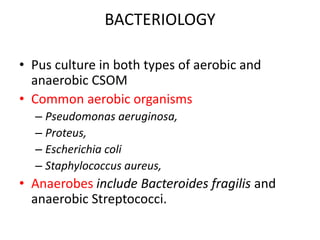
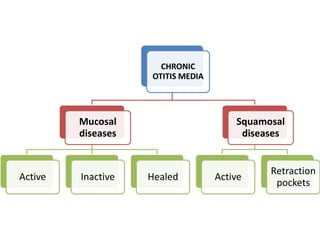
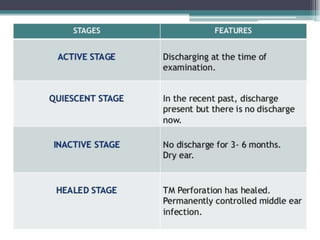
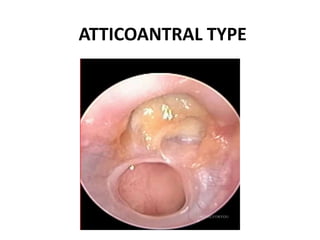
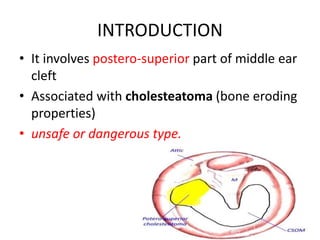
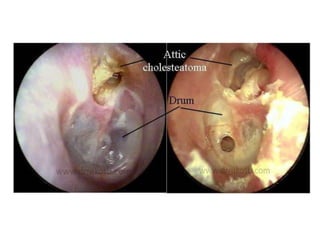
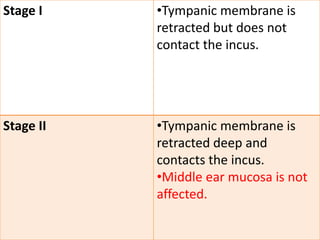
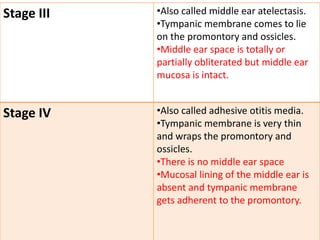
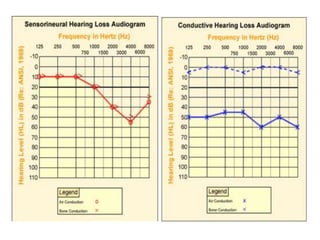
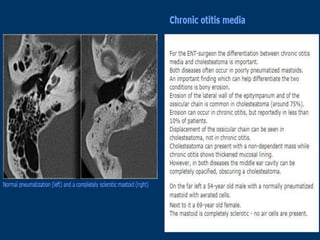
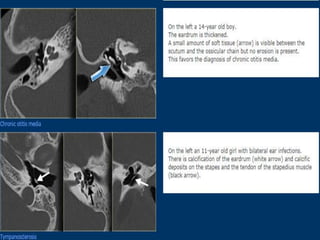
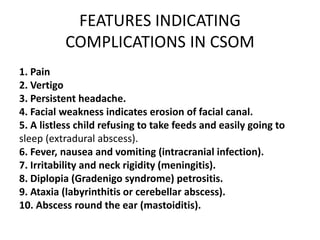
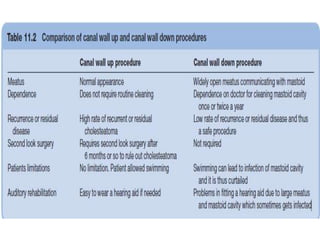
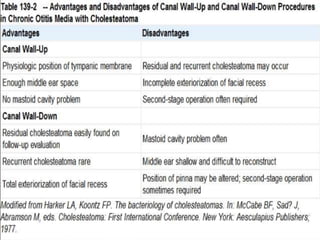
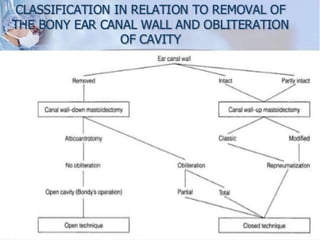
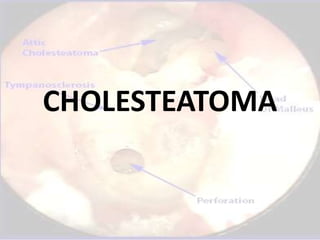
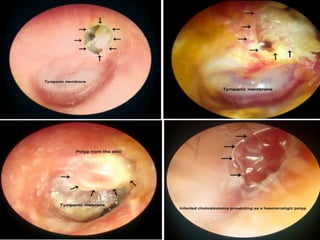
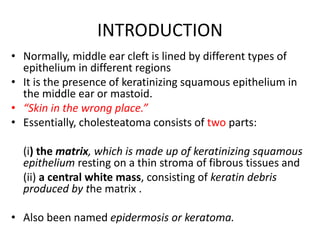
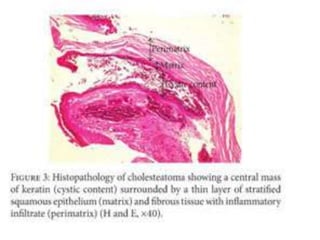
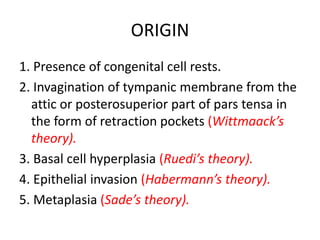
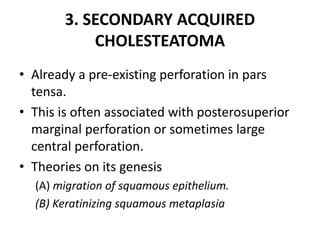
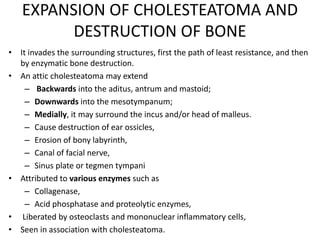
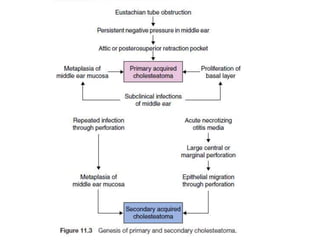
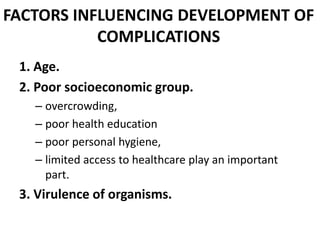
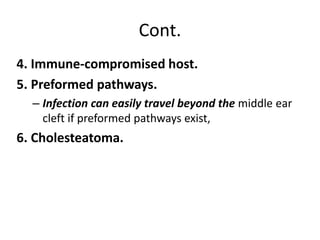
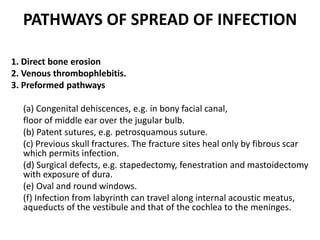
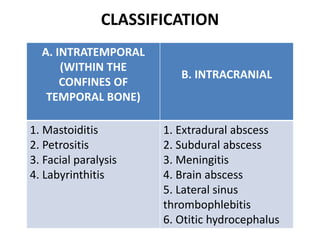
This document discusses chronic suppurative otitis media (CSOM), which is a long-standing middle ear infection characterized by ear discharge and a permanent perforation of the eardrum. It describes the two main types of CSOM - tubotympanic and atticoantral - and covers their etiology, pathology, clinical features, investigations, treatment, and complications. Cholesteatoma, a growth of skin cells in the middle ear, is also discussed in detail including its origin, classification, expansion and bone destruction potential, and role in increasing risk of complications from middle ear infections.